Endocrine & Metabolic Disorders: Introduction
Endocrine disorders commonly cause musculoskeletal symptoms and may even present with rheumatic syndromes before the nature of the underlying endocrinopathy is apparent (Table 55–1). On occasion, endocrine disorders can mimic rheumatic diseases and be a source of diagnostic error (Table 55–2). Rheumatic manifestations of endocrine diseases are usually a consequence of the hormonal abnormalities but, in the case of autoimmune thyroid disease, also can be a result of the underlying autoimmune process.
| Rheumatic Disorder | Endocrinopathy |
|---|---|
| Carpal tunnel syndrome |
|
| Flexor tenosynovitis |
|
| Chondrocalcinosis/pseudogout |
|
| Osteopenia/osteoporosis |
|
| Destructive arthropathy |
|
| Premature/unusual osteoarthritis |
|
| DISH | Diabetes |
| Myopathy |
|
| Manifestation | Endocrine Disorder | Mimics |
|---|---|---|
| Myalgias, arthralgias, fatigue |
|
|
| Proximal muscle weakness |
| Polymyositis |
| Shoulder girdle pain and stiffness | Hyperthyroidism | Polymyalgia rheumatica |
| Degenerative arthritis |
| Osteoarthritis |
| Distal soft-tissue swelling and periostitis | Graves disease (thyroid acropachy) | Hypertrophic osteoarthropathy |
| Synovitis with ANA | Hashimoto thyroiditis | SLE, RA |
| CPPD, pseudogout |
| Idiopathic CPPD |
Diabetes Mellitus
Patients with either type 1 or type 2 diabetes mellitus frequently have musculoskeletal complaints. Although relatively little is understood about the pathophysiological effects of hyperglycemia on bones, joints, tendons, and muscles, there are well-established associations between diabetes and certain musculoskeletal syndromes (Table 55–3).
- Most commonly seen in hands.
- Limited flexion and extension of finger joints.
- Skin becomes progressively puffy and appears shiny and waxy.
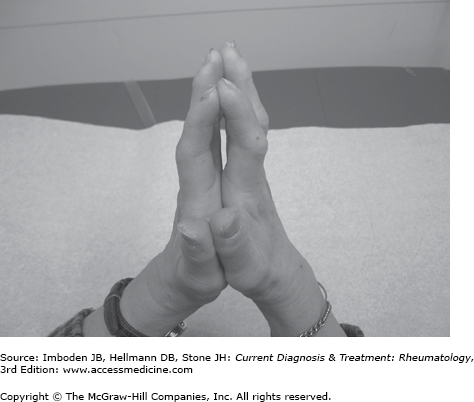
- “Prayer sign” is simple diagnostic maneuver.
Diabetic cheiropathy, or limited joint mobility syndrome, usually develops after 10 or more years of diabetes (type 1 or 2), particularly when glycemic control has been suboptimal, and likely is due to abnormal glycosylation of connective tissues. Although most frequently recognized and encountered in the hands, this condition can involve the shoulders, knees, and feet.
The limited mobility results from a generalized palmar fasciitis and from progressive thickening and tightening of the skin. In many instances, the skin becomes progressively puffy, shiny, and waxy in appearance, mimicking sclerodactyly. In a simple diagnostic maneuver, referred to as the prayer sign, the patient places his or her hands together, as if in prayer. Patients with limited mobility syndrome are unable to make complete contact between the palmar surfaces of their fingers (Figure 55–1). Improved glycemic control as well as physical and occupational therapy may help slow the progression of diabetic cheiropathy.
- Presents with an isolated nodule on one of the flexor tendons of the hand, most commonly of the long or ring fingers.
- Nodules become symptomatic when they impede tendon motion.
- Dupuytren contractures may develop with chronic tenosynovitis of the flexor tendons.
Flexor tenosynovitis of the hand, which develops in 12–15% of patients with diabetes, also may be due to abnormal glycosylation of collagen. Early in its course, this condition presents with an isolated nodule on one of the flexor tendons of the hand, most commonly of the long or ring fingers. These nodules become symptomatic when they impede tendon motion, locking the finger in flexion or creating a racheting sensation when the finger is flexed and then extended. The nodules can be palpated just distal to the palmar crease of the affected finger. Local glucocorticoid injections into the tendon sheath usually reduce the size of the nodule and alleviate symptoms (see Chapter 6).
Chronic tenosynovitis of the flexor tendons can progress to Dupuytren contractures. These contractures most commonly involve the fourth finger and can result in significant disability when the affected fingers become locked in flexion. The fibrotic tendon is usually palpable as it courses through the palm proximal to the palmar crease.
Glucocorticoid injections have little efficacy, but there may be benefit from injections of collagenase. The standard recommendation for surgical referral is contracture at the metacarpophalangeal joint of at least 30 degrees or any contracture at the proximal interphalangeal joint.
- Loss of the range of motion of the shoulder is significant and develops rapidly.
- Plain radiographs reveal few abnormalities of the glenohumeral joint.
Adhesive capsulitis, commonly referred to as “frozen shoulder,” occurs in up to 12% of patients with diabetes. Relatively rapid and significant loss of the range of motion of the shoulder develops in affected individuals. Some patients have antecedent calcific tendinitis, peritendinitis, or bursitis of the affected shoulder. Plain radiographs reveal few abnormalities of the glenohumeral joint, despite the degree of immobility. Early and aggressive physical therapy must be used to preserve range of motion and minimize the time of immobility.
- Numbness or paresthesias in a distribution consistent with median nerve involvement.
- Can progress from an irritating sensory neuropathy to weakness and wasting of the thenar muscles of the hand.
Diabetes and carpal tunnel syndrome are prevalent, and the frequent coexistence of these disorders has led many to believe that diabetes predisposes to carpal tunnel syndrome. Patients with carpal tunnel syndrome usually complain of numbness or paresthesias in a distribution consistent with that innervated by the median nerve (see Chapter 6). These symptoms are often exacerbated at night and may awaken a patient from sleep. Carpal tunnel syndrome can progress from an irritating sensory neuropathy to weakness and wasting of the thenar muscles of the hand. Provocation of paresthesias in a median nerve distribution by either a Phalen maneuver or Tinel sign can help confirm the diagnosis. Nerve conduction studies localize the site of the nerve compression to the wrist and differentiate carpal tunnel syndrome from other types of neuropathy.
Initial treatment focuses on conservative measures. Patients are asked to wear wrist splints, particularly at night, and refrain from various activities that may exacerbate the condition. Local glucocorticoid injection into the carpal tunnel or surgical decompression should be used if symptoms persist or motor signs develop.
- The usual presentation is a single, painless (or relatively painless), swollen, and deformed joint, but bilateral disease also occurs.
- The metatarsophalangeal, tarsal, and talar joints are most commonly involved.
- Radiographs confirm the diagnosis.
Diabetes mellitus is the leading cause of neuropathic arthropathy, which was first described by Jean Martin Charcot in patients with tabes dorsalis. A common complication of diabetes is a progressive sensory neuropathy that preferentially affects axons with the greatest length (ie, those innervating the extremities) and produces the classic “stocking and glove” distribution of paresthesias and numbness. The neurotraumatic hypothesis of joint damage postulates that the sensory neuropathy impairs normal protective mechanisms of the regional joints, particularly those of the foot and ankle. The lack of proprioceptive protection leads to progressive microfractures and subsequent destruction of the joint with little or no pain or recognition of what is developing. The neurovascular hypothesis of Charcot arthropathy proposes that an aberrant sympathetic tone results in increased blood flow to the bones with subsequent bone resorption and susceptibility to bone structural damage.
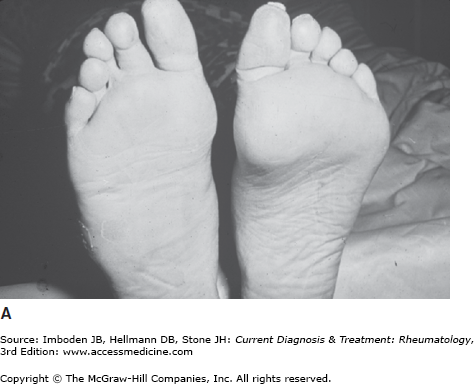
Patients usually have a single, painless (or relatively painless), swollen, and deformed joint, but bilateral disease also occurs. There may be overlying warmth and erythema. The metatarsophalangeal, tarsal, and talar joints are most commonly affected (Figure 55–2), but the knees, spine, and shoulders may also be involved. There are signs of a sensory neuropathy on neurologic examination.
Figure 55–2.
Charcot arthropathy. A: Deformity of the left foot of a patient with chronic diabetes mellitus and long-standing peripheral neuropathy. B: Radiograph of Charcot arthropathy involving the first and second metatarsals. (Used with permission, from Dr. Carl Grunfeld, San Francisco Department of Veterans Affairs Medical Center, University of California, San Francisco.)
Radiographs confirm the diagnosis. Classic radiographic findings of Charcot arthropathy include subluxation, fracture, bony fragmentation, exuberant sclerosis, and destruction of the joint (Figure 55–2). Sometimes there is dramatic osteolysis of the bones of the feet, with involvement ranging from areas of patchy osteopenia to marked distal bone resorption. The destruction can be so dramatic as to cause concern for osteomyelitis or a septic joint, especially when there is a contiguous diabetic ulcer. The radiographic appearance sometimes mimics severe osteoarthritis, leading to the admonition to consider Charcot arthropathy when a radiograph reveals “degenerative arthritis times ten.” The combination of an unusually destructive degenerative disease in a location not usually affected by osteoarthritis (eg, the tibiotalar, subtalar, and glenohumeral joints) should raise the suspicion of a Charcot joint.
Unfortunately, the treatment of Charcot joints, particularly those below the knee, remains suboptimal once the destructive process has become advanced. If detected early, the progress of disease can be somewhat slowed by various protective measures, including the limitation of weight-bearing on the affected joint and the use of specially crafted orthotic supports for the surrounding joint structures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree