Eisenmenger Syndrome
Stephen M. Paridon
Eisenmenger syndrome comprises a group of cardiac defects that share a common pathophysiology: pulmonary vascular obstructive disease resulting in a right-to-left cardiac level shunting of blood. Although the syndrome has been described since the nineteenth century, generally its currently accepted definition is credited to Wood (late 1950s). With the diagnostic approaches to and surgical therapies for congenital heart defects that have been developed since the 1960s, the incidence of Eisenmenger syndrome has decreased greatly. However, a certain population with this syndrome is too old to have benefited from the newer medical techniques or is the result of failure of current medical understanding.
ETIOLOGY AND PATHOPHYSIOLOGY
Eisenmenger syndrome is not a discrete cardiac defect. Rather, it is a group of cardiac defects with the common components of a large cardiac defect that allows the intracardiac shunting of blood with superimposed obstructive pulmonary vascular disease.
Lesions most likely to lead to Eisenmenger syndrome are those that allow high pulmonary-to-systemic flow ratios to occur in the presence of high pulmonary pressures, such as large defects of the ventricular septum, atrioventricular canal lesions, and patent ductus arteriosus. The presence of hypoxemia, such as occurs in D-transposition of the great arteries with a ventricular septal defect or truncus arteriosus, hastens the development of pulmonary vascular disease. Generally, defects with low pulmonary pressures, such as atrial septal defects, are much less likely to lead to Eisenmenger syndrome. Usually, despite their high rate of pulmonary blood flow, these lesions are tolerated well for decades, whereas high-pressure defects may result in changes in the pulmonary vascular bed that occur within several years or, occasionally, months.
As obstructive pulmonary vascular disease develops, resistance increases in the pulmonary vascular bed. Systemic venous blood, following the course of least resistance, is shunted away from the pulmonary arteries and through the cardiac defect into the systemic circulation. The result is systemic hypoxemia, the degree of which depends on the relative pulmonary-to-systemic vascular resistance. The more severe the pulmonary resistance or the lower the systemic resistance, the greater is the right-to-left shunting.
Generally, at the time diagnosis of heart disease is made, the clinical presentation is that of pulmonary overcirculation, which results from a high rate of pulmonary blood flow caused by large cardiac defects with low pulmonary vascular resistance. In lesions that result in hypoxemia and a high pulmonary blood flow rate, such as D-transposition of the great arteries with ventricular septal defect, cyanosis is superimposed on pulmonary congestion.
As pulmonary vascular resistance increases, signs and symptoms of pulmonary congestion decrease. The duration of this change varies from months to decades, depending on the presenting cardiac defect and the rate at which vascular changes occur. When pulmonary resistance exceeds systemic resistance, hypoxemia ensues and then progresses as pulmonary vascular resistance rises.
CLINICAL MANIFESTATIONS AND COMPLICATIONS
Physical Findings
Findings on physical examination of patients with Eisenmenger syndrome vary depending on the severity of pulmonary obstructive disease. In advanced stages, cyanosis is pronounced. Usually, clubbing of the extremities is present. In early cases, cyanosis may be mild or absent, or it may become noticeable only when systemic resistance drops, such as with exercise.
Findings of the cardiovascular examination are typical of patients with pulmonary hypertension. The precordium is hyperdynamic, and a right ventricular lift may occur in patients with defects that include a normal right ventricle. The second heart sound is very loud and frequently is palpable at the left upper sternal border because of the pulmonary (P2) component of the second sound. Generally, splitting of the second sound is absent or very narrow as a result of the decreased ejection time of the right ventricle in the presence of high pulmonary resistance.
Usually, murmurs are soft because the intracardiac defects are large, with little pressure gradient present between the chambers, and most of the right-to-left shunting of blood in these defects occurs during diastole, a period of relatively low pressure. The findings typical of left ventricular failure, such as rales caused by pulmonary edema, are absent. In severe cases, evidence of right ventricular failure may be present. Hepatomegaly and peripheral edema may occur in end-stage disease.
Laboratory Findings
The chest radiograph in Eisenmenger syndrome varies with the clinical course. Early in life, before the onset of increased pulmonary vascular resistance, the size of the heart usually is larger, with increased pulmonary vascular markings. Flooded pulmonary vasculature and pulmonary edema are evident (Fig. 267.1A). The classic chest radiograph for Eisenmenger syndrome develops after the onset of elevated pulmonary vascular resistance. The cardiac silhouette is small to normal. Proximal pulmonary arteries are dilated and tortuous. Generally, a diminished distal pulmonary vasculature occurs, giving the lung fields a black appearance in the periphery (Fig. 267.1B). Late in the clinical course, cardiomegaly also can be seen in which right-sided cardiac decompensation has occurred. Pulmonary vasculature, however, remains sparse and tortuous (Fig. 267.1C).
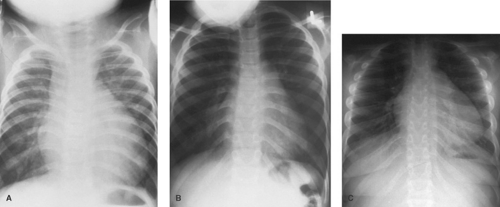 FIGURE 267.1. Progressive changes observed with pulmonary vascular obstructive disease in a series of chest radiographs from a patient with an unrepaired complete atrioventricular canal. A: At age 6 months, cardiomegaly with increased pulmonary vascular markings caused by pulmonary overcirculation is noted. B: At age 4 years, cardiac size is only slightly enlarged, with prominent main pulmonary arteries but diminished peripheral lung field vasculature. C: At age 15 years, cardiomegaly is caused by dilated, poorly functioning ventricles. The main pulmonary arteries are prominent, but the peripheral vasculature remains sparse.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




