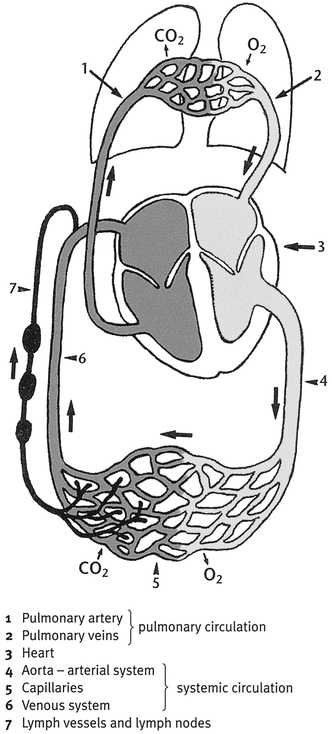
. An overview of the capillary vascular structures and their relationship to each other is a prerequisite for a more detailed discussion of these systems. The vascular structures include the interstitium, the arteriole, and the venule. The interstitium is the space between cells. It contains both the smallest arterial vessel, called an arteriole, and the smallest venous structure, called a venule.1, 2 Both the arteriole and the venule terminate in capillaries, which are joined histologically (Fig. 3-1). The heart is responsible for pumping blood through these structures. The lymphatic system originates in the interstitium with the smallest of the lymphatic vessels, called the initial lymphatic or lymphatic capillary, and culminates in the largest lymphatic structure, called the thoracic duct.2 The venous system has a continuous-loop pump system based on the heart pumping oxygenated blood to the arteries, arterioles, venules, veins and back to the lungs and heart. However, the lymphatic system does not have this continuous central pump system (see Fig. 3-1).3 Also, unlike with venous capillaries in the interstitium, molecules do not diffuse into the lymphatic capillary. Therefore the lymphatic system must be stimulated to activate a force pump, (external and internal vacuum stimulation that moves lymph), creating a vacuum and drawing the lymph proximally.3 Initial lymphatics, which are larger than venules, are finger-shaped tubes that are closed on the distal end and lined with overlapping, oak leaf–shaped endothelial cells. Anchor filaments extend from the endothelial cells to the connective tissue (Fig. 3-2). Movement of the connective tissue pulls on the anchor filaments. This, in turn, pulls on the overlapping flaps (junctions) of the endothelial cells, and water and large molecules are admitted into the initial lymphatic.1,2,4 Large molecules also enter the initial lymphatic when a change in the interstitial pressure causes the junctions of the endothelial cells to spread apart. The initial lymphatic connection forms a netlike structure.1,3 The balance between fluid moving into and out of the vascular vessels on a cellular level, which was first described by Ernest Starling in the early 1900s, is called Starling’s equilibrium.1,2 This balanced movement of fluid functions as a gradient system from high to low pressure. On the capillary level, arteriole hydrostatic pressure (the pressure of the blood fluid exerted on the arteriole vessel wall) is 30 to 40 mm Hg, which is enough pressure to cause filtration of electrolytes, fluid, a few small plasma proteins, and other nutrients into the interstitium.1,2 The colloid osmotic pressure (also called the oncotic pressure) in the interstitium is determined by the concentration of proteins in this intercellular space; this pressure is approximately 25 mm Hg.2 Tissue cells in the interstitium absorb the nutrients, electrolytes, and other substances filtered out of the arteriole. Of the remaining substances, 90% diffuse by osmosis into the venous system.1–3 The residual 10% of leftover substances are large molecules, which are absorbed by the lymphatic system.1–3 These large molecules consist of plasma proteins, minerals, ions, hormone cells, bacteria, fat cells, and fluid.1–5 Once the cells enter the initial lymphatic, they make up a substance called lymph.2 As lymph enters the initial lymphatic, it causes pressure changes that open the valve connected to the next lymphatic vessels, the three-celled collector lymphatics (Fig. 3-3). Clinically, the most important features of the tube-like collector lymphatics are a middle layer of muscle cell and the presence of valves every 6 to 8 mm along the tube.1,3 The chamber between two valves is called a lymphangion.3 As a bolus of lymph enters a lymphangion, the single layer muscle cell contracts against the expanding lymphangion and pushes the bolus proximally into the next lymphangion (see Fig. 3-3). This process continues until the bolus reaches the afferent lymphatic pathways of the lymph node. The pumping movement of the lymphangions resembles the peristaltic movement of the small intestine. The lymphangions pump at a rate of 10 to 20 times per minute,3 and exercise can increase this pumping motion by 10 to 30 times.1 Recent theories hold that peristalsis also creates a negative pressure that opens the junctions of the endothelial cells, enabling large-molecule substances to move from the interstitium into the initial lymphatic.3 Eventually the bolus of lymph moves into the afferent lymphatic pathways of the lymph nodes. Lymph nodes, which perform several immunologic functions, are composed of a series of complex sinuses and therefore often are considered “dams” or “kinks in the hose” in the movement of lymph. Excessive swelling distal to the lymph nodes does not increase their rate of filtration, but rather causes further congestion distally.4 Venous vessels do not connect to lymph nodes and therefore do not reflect this slowing of fluid movement. Also, venous vessels do not carry bacteria or tissue waste products and therefore do not pass these substances through the lymph nodes for cleansing. Lymph nodes present significant resistance to the flow of lymph and must be massaged to facilitate a faster flow of the distal congested lymph.4 The MEM method of massaging healthy and uninfected nodes uses MEM pump point stimulation, which is a method of simultaneously massaging two groups of nodes, bundles of lymphatic vessels, or watershed areas (anatomical drainage dividing areas), which theoretically speeds up the movement of lymph through the nodes. From the nodes, lymph can enter the venous system directly, through lymphovenous anastomoses (areas where the small vessels of the lymphatic and venous systems join), or it can continue on in the lymphatic vessels and empty into either the right lymphatic duct or the largest lymphatic vessel, the thoracic duct. The thoracic duct lies anterior to and parallel with the spinal cord from approximately L2 and empties into the left subclavian vein.2,3 The right lymphatic duct terminates in the right subclavian vein. The movement of lymph in the thoracic duct is affected by changes in thoracic pressure. Diaphragmatic breathing expands the abdomen, causing changes in thoracic pressure that move the contents of the thoracic duct more proximally.1,3 This action creates a vacuum, drawing lymph from the more distal vessels toward the thoracic duct.1,3 Treatments such as MEM, therefore, begin with diaphragmatic breathing and trunk exercise. This is analogous to removing the plug from a drain or a clog from a backed-up sink. The clog must be removed before the water can flow out. In terms of clinical application, the vacuum created by diaphragmatic breathing moves lymph more proximal in the thoracic duct, creating a space into which the more distal peripheral edema can move. Before they reach the thoracic duct, the deep lymphatic trunks share a common vascular sheath with the venous and arterial structures.3 Therefore exercise increases the rate of arterial flow and passively stimulates the lymphatic vessels, increasing the rate of lymph flow. Also, at least 200 lymph nodes are located centrally and around deep venous and arterial structures. Exercise of the abdominal muscles increases the pumping of blood, which stimulates the lymph nodes, moving lymph through them more rapidly—a force pump action. “Exercise is key to lymphatic activation” is a frequently heard statement. Yet therapists know that in most cases, simply exercising the edematous hand or arm in the subacute phase does not significantly or permanently reduce edema. Lymphatic structures can exceed 30 times their normal capacity before edema becomes visible;1 this means that proximal to the visible edema is the beginning of non-visible edematous congestion. Exercise and light massage significantly proximal to the visible edema create a negative pressure, drawing lymph proximally and thus removing the “clog.” The results of research by Pecking and colleagues6 present a strong argument for stimulating lymphatic absorption and conduction significantly proximal to visible edema. In these researchers’ study, manual lymphatic drainage (MLD) (the manual decongesting of lymph through activating the lymph uptake through massage, low-stretch bandaging programs, and so on) was performed exclusively to the contralateral, normal upper quadrant on 108 women with lymphedema caused by mastectomy; this resulted in a 12% to 38% lymph uptake in the hand, even without massage of the involved area.6 The contralateral massage created a negative pressure (vacuum), drawing the lymph from the involved to the uninvolved area, where it could be absorbed into the normal system. The venous and lymphatic systems have many pump-like structures that help propel the blood back to the heart. Because of the descending gradient of hydrostatic pressures from the arteriole capillary to the venule capillary, small-molecule substances diffuse easily and are reabsorbed into the venous capillary through its thin wall.2 Active muscle contraction acts as a pump as it compresses and empties the large deep venous vessels. As this blood is propelled proximally toward the heart, a negative pressure is created, which draws blood from the periphery into the deep veins. Edema develops when the descending gradient of Starling’s forces are disrupted by an interruption and an imbalance. The cascade of events that occurs after tissue laceration is a good example. Initially, an outflow of water and electrolytes (transudate edema) into the wound occurs. The mast cells then release histamines, which greatly increase capillary permeability, and plasma proteins, phagocytic cells, and other substances leak into the area. Plasma protein fibrinogen is converted to fibrin, which plugs the endothelial cells lining the lymphatics.7 This prevents the lymphatics from temporarily removing the large molecules as the various phagocyte cells perform their “cleanup” function.7 Edema results when excess fluid and plasma proteins are trapped in the interstitium. Starling’s equilibrium is disrupted, because the trapping of excess proteins in the interstitium increases the colloid osmotic pressure. Several techniques can be used to reduce excessive fluid outflow (edema). For example, a bulky hand dressing applied at the time of surgery gives counterforce to the outflow (filtration) by changing the tissue pressure. It is composed of appropriate wound care dressing, fluffy gauze sponges, and rolled-on gauze. After soft tissue trauma, immobilization for up to a week in a bulky dressing or plaster splint facilitates healing of involved structures by preventing stress on fragile tissue, which could cause microscopic rupture of vessels with resulting edema. The therapist should check the dressing or splint to make sure it is not too tight and should contact the physician immediately if this is a possibility. A bulky dressing that is too tight causes vascular changes, temperature changes, increased edema, or severe, painful compression of the fingers and can lead to tissue breakdown. The capillary refill test can be used to check vascular status (see Chapter 5). The therapist also must teach the client that any vascular changes (that is, changes in tissue color) or sensory changes must be reported immediately to the physician. Procedures, such as tenolysis and flexor tendon repair, involve minimal or no immobilization in a bulky dressing. However, even with these diagnoses, limited motion can increase edema, therefore early motion must be balanced with rest to prevent this. Elevation of the hand above the heart, if not contraindicated, also reduces outflow because it reduces the arterial hydrostatic pressure.10 Elevation in the acute stage facilitates lymphatic flow because hydrostatic gradient pressure is increased along the lymphatic trunks.4 Ideally, the involved extremity is elevated in a plus 45-degree “ski hill” position; this means that pillows are placed so that the elbow is above the shoulder, and the hand is above the elbow and wrist. Keeping the arm elevated while sleeping can be difficult. Often clients use pillows on either side of them. A belt can be fastened around the pillows to keep them together. Also, the bed can be moved against the wall so that one set of pillows is pushed up against the wall, preventing them from falling. For clients with finger replantation, elevation no higher than the heart is recommended to avoid compromising arterial blood flow.11 Cold packs, if not contraindicated for vascular and tissue ischemia reasons or diseases such as Raynauld’s, cause vasoconstriction and thus reduce the outflow of fluid in the acute stage. However, the temperature of the cold pack is a consideration. Research shows that when the temperature is lower than 59° F (15° C), proteins leak into the interstitium from lymphatic structures.12 Excess proteins in the interstitium cause edema. Precaution. To prevent “ice burn” to tissue, always place a dry towel between the skin and the cold pack. Cold packs should not be used on a client with a replanted hand or digit because of the effect of vascular compromise on tissue viability.13 A nerve repair may be injured by cold postoperatively. Clients should get explicit care instructions from their physicians, including precautions on the use of cold packs. Elastic taping is becoming the common generic term used to designate a variety of tapes similar to the original Kinesio Tex tape developed by a Japanese-born chiropractor, Dr. Kenso Kase, in the 1970s.14 The cloth-like tape has acrylic glue applied to one side in a wave-like pattern, such as a finger print swirl. When the tape is applied in a specific manner it is theorized that the edema reduces because patient movement pulls the skin in the opposite direction from where the tape was applied. This movement puts a stretch on the initial lymphatic structures facilitating congested lymphatic absorption.15 Increasing this space, creates a pull on the connective tissue anchor filaments attached to the endothelial cells of the initial lymphatics; this separates the planted endothelial junctions, thereby increasing lymph and fluid flow. Many wonder why MEM is not started in the acute stage. In 1989, Hutzschenreuter and Brummer16 did a research study on this point using sheep. They compared the results in two groups, one in which MLD was performed and one in which it was not over a defined period (that is, immediate postoperative to 3 weeks postoperative). They found that both groups showed minimal fluid reduction during the first week after surgery. However, after the first week, the MLD group had a significantly greater increase in fluid movement and edema reduction than the control group.16 These results are not surprising because initially, acute edema is transudate that is changing to exudate edema as the plasma proteins invade and are contained. Only the lymphatic vessels can remove excess proteins from the interstitium.1,2 MEM and manual lymphatic treatment∗ (MLT) programs are designed to activate lymphatic vessels.
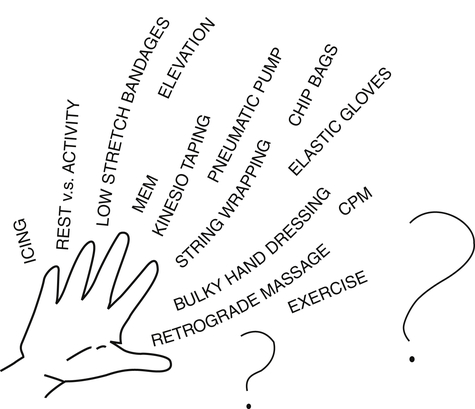
Edema Reduction Techniques
A Biologic Rationale for Selection
Overview of Lymphatic Anatomy Related to Edema Reduction
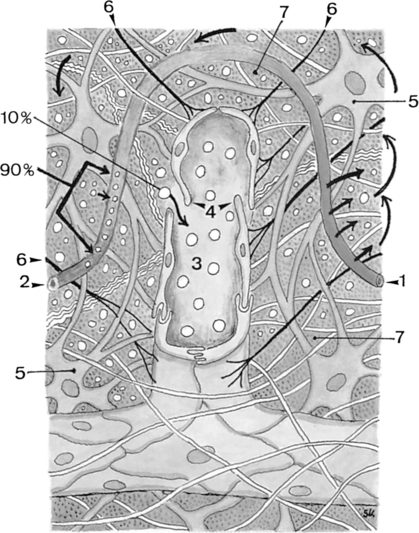
1, Arterial section of the blood capillary; 2, venous section of the blood capillary; 3, lymph capillary; 4, open intercellular groove-swinging tip; 5, fibrocyte; 6, anchor filaments; 7, intercellular space. Small arrows indicate the direction of blood flow; large arrows indicate the direction of intercellular fluid flow. (From Foldi M, Foldi E, Kubik S: Textbook of lymphology for physicians and lymphedema therapists, Munich, 2003, Urban & Fischer Verlag.)
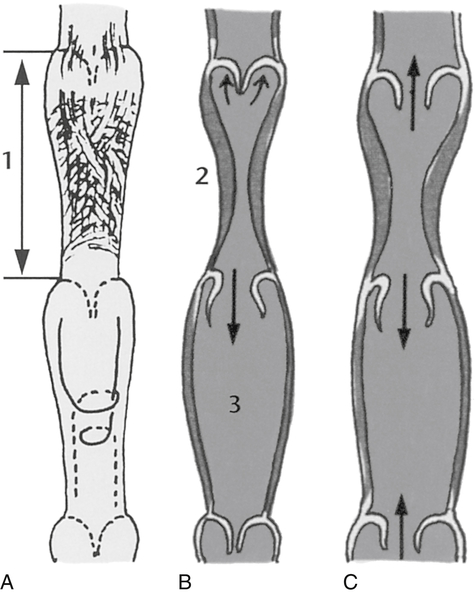
A, Arrangement of the musculature. B, Normal function. C, Dilated lymph vessel with valvular insufficiency and reflux. (From Foldi M, Foldi E, Kubik S: Textbook of lymphology for physicians and lymphedema therapists, Munich, 2003, Urban & Fischer Verlag.)
Acute Edema Related to the Vascular Anatomy
Reduction Techniques for Acute Edema
Bulky Dressing
Elevation
Cold Packs
Elastic Taping
Indications for Manual Edema Mobilization in the Acute Stage
Edema Reduction Techniques: A Biologic Rationale for Selection




