Dynamic External Fixation of Proximal Interphalangeal Joint Fracture-Dislocations
Grey Giddins
Alex Cowey
DEFINITION
Proximal interphalangeal (PIP) joint bone injuries may affect the convex side of the joint (end of the proximal phalanx) or the concave side of the joint (base of the middle phalanx).
Convex-side injuries are typically simple (two fragment) injuries best treated conservatively or with open reduction and internal fixation if displaced.
Concave-side injuries tend to be comminuted (multifragmented), presenting either as fracture-subluxations/dislocations or a pilon-type fracture.
Fracture-subluxations/dislocations typically involve dorsal displacement of the main fragment of the middle phalanx (FIG 1A), although volar and lateral subluxations and dislocations do occur (FIG 1B,C).
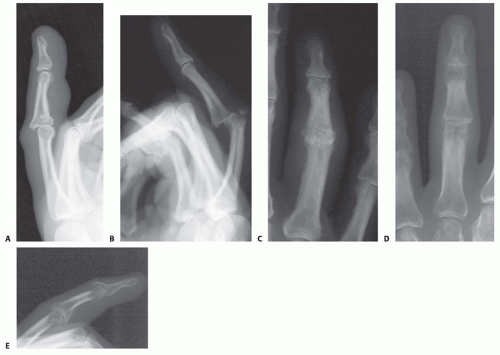
FIG 1 • A. A typical (more severe) dorsal fracture-dislocation with involvement of about 65% of the volar articular surface. B,C. PIP joint volar dislocation. D,E. PIP joint pilon fracture.
Dorsal fracture-dislocations typically occur after a hyperextension injury of the PIP joint.
Pilon-type fractures are compression fractures of the base of the middle phalanx and are characterized by depression of the central articular component and splaying of the articular margins, typically highly comminuted (FIG 1D,E) and there maybe longitudinal extension along the length of the middle phalanx. The classic mechanism is a longitudinal (end-on) force, crushing the base of the middle phalanx, such as fall or miscatching a ball.
ANATOMY
The distal end of the proximal phalanx is a convex surface made up of two condyles. The proximal end of the middle phalanx is a concave surface (FIG 2A).
The stability of the PIP joint is secondary to the bony congruency, the tendons that cross the joint (flexor and extensors) plus a series of ligaments (FIG 2B):
Volar plate—a very strong concave structure, such as the roof of a tunnel, running from the volar surface of the proximal phalanx to the volar surface of the middle phalanx
Radial and ulnar collateral ligaments
True collaterals—run from the proximal phalanx to the volar 50% of the middle phalanx
Accessory collaterals—run from the proximal phalanx into the volar plate
These ligaments work together to resist dorsal subluxation of the PIP joint when loaded and are said to act as three sides of a box with joint instability being inevitable if two of the three sides are injured.
PATHOGENESIS
The extensor tendon attachments are dorsal, proximal, and relatively weak through the central slip, whereas the flexor digitorum superficialis tendon slips insert volarly, more distally, and are stronger. The joint center of rotation is in the middle of the head of the proximal phalanx. Thus, the flexor moment arm is much greater than the extensor moment arm.
The shape of the joint and the soft tissue restraints allow a powerful lever arm to work for flexion. If, however, the volar restraints fail following trauma, the resultant forces lead to dorsal subluxation and proximal migration of the middle phalanx (FIG 3A).
In practice, it is possible for dorsal subluxation to occur with an injury to as little as 10% of the volar joint surface, but this is uncommon. Research has shown that the joint will be stable if less than 42% of the volar half of the middle phalanx articular surface is damaged as measured on a lateral radiograph (FIG 3B). The reason for this is the collateral ligaments remain functional despite the incompetence of the volar plate, hence two sides of the box are competent. Once more than 42% of the volar joint surface is involved, the collaterals become incompetent and all three sides of the box are lost.
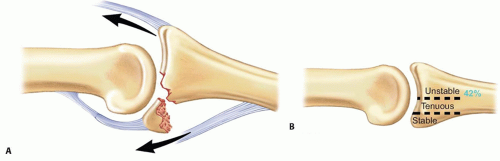
FIG 3 • A. Diagram of fracture-dislocation. B. Diagram showing volar loss, which may lead to instability.
For pilon-type fractures, the condyles of the proximal phalanx are driven up into the base of the middle phalanx, displacing the central part of the articular surface distally and splaying the dorsovolar and lateral margins of the middle phalanx joint surface. This injury is longitudinally unstable and results in proximal migration and diminution or obliteration of the joint space, usually with significant articular incongruity.
PATIENT HISTORY AND PHYSICAL FINDINGS
The majority of patients present acutely within a few days of the injury, although presentation after 2 weeks and even after 6 weeks is not unheard of. The delays are usually due to underestimation of the severity of the injury either by the patient (who thinks he or she has a sprain and it will resolve) or medical/paramedical staff (who fail to perform or interpret properly an adequate radiograph).
The finger will be swollen and tender, centered around the PIP joint.
An angular deformity may be evident.
Subluxation of the joint may be clinically evident, visually or by palpation.
There will be reduced range of movement throughout the finger and particularly in the PIP joint.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The key investigation is plain radiology.
Posteroanterior and lateral radiographs need to be taken, centered on the PIP joint of the injured finger; radiographs of the hand are not adequate (FIG 4).

FIG 4 • A-C. Hand radiographs are interpretable only with a true lateral radiograph of the PIP joint.
Subluxation and dislocation are best visualized on the lateral radiograph and may be quite subtle, appearing as joint incongruity at the dorsum of the joint (the triangle sign, due to dorsal overhang of the base of the middle phalanx) (FIG 5E).
The key information obtained from the radiographs (supplemented by physical examination) can be used to differentiate stable from unstable injuries, either of fracture-subluxations or dislocations or pilon fractures.
Fluoroscopy can be of great value in assessing the injury and joint stability.
DIFFERENTIAL DIAGNOSIS
Soft tissue
Volar plate injury
Collateral ligament injury
Central slip injury
Bone
Proximal phalanx condylar injury
Proximal phalanx distal diaphyseal injury
Middle phalanx proximal diaphyseal injury
NONOPERATIVE MANAGEMENT
If the injury is stable, early protected mobilization can start within 1 week of injury.
Fracture-Dislocation
Mild injuries with limited volar plate avulsion reduce either spontaneously or with assistance, usually under local anesthesia, radiographs may reveal a small volar bone avulsion from the base of the middle phalanx (FIG 5A-D). These injuries are longitudinally stable and can be treated with early mobilization concentrating on regaining extension, which is commonly lost.
Only if there is significant preexisting volar plate laxity (often occurs in young women) is there a need for an extension block splint for up to 6 weeks.
Most patients regain full or nearly full movement but may be left with minor swelling and stiffness and mild cold discomfort.
Heavy activity may cause discomfort.
In approximately 5% of patients, the joint remains significantly swollen and uncomfortable beyond 6 weeks. This is probably due to persistent joint synovitis, which usually resolves with a steroid injection.
If the joint is unstable but there is limited volar joint damage (less than about 30%), it may reduce when held in flexion with a dorsal block splint.
Joint reduction and congruity must be documented radiologically and should not require more than about 50 degrees of joint flexion, or unacceptable PIP joint stiffness may result.
Patients should be encouraged to flex and extend to the splint. They should be seen weekly for 4 weeks. Flexion of the splint is reduced by about 10 degrees each week. At each increase in extension, the reduction needs to be precisely checked radiologically.
A reasonable range of movement with only a mild flexion contracture and loss of flexion is anticipated.
Pilon Fractures
The majority of pilon-type fractures have significant displacement and surgical stabilization is required to achieve longitudinal stability and early movement, but in a small number of cases, there is minimal displacement (<1 mm)
and a reasonable joint space (FIG 6). These are usually stable injuries but must be carefully assessed clinically.

FIG 5 • A. Dorsal lateral fracture-dislocation with a small avulsion fragment before (A,B) and after (C,D) reduction. E. Dorsal fracture-subluxation with joint incongruity and a classic V sign (see Chap. 53 Fig 4B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access







