CHAPTER 25 Double-Bundle Posterior Cruciate Ligament Reconstruction
Injuries to the posterior cruciate ligament (PCL), although infrequent, often present as complex problems that can result in severe disability because of the relationship between posterior instability and rotatory instability, combined with other ligamentous injury and cartilage degeneration. It is rare that PCL injuries occur in isolation; they frequently present in conjunction with anterior cruciate ligament (ACL) or posterolateral corner injuries.1 Both the rare isolated and concomitant PCL lesions are often misdiagnosed or overlooked altogether because PCL-specific symptoms can be difficult to distinguish or can be confounding when presenting with additional injuries.2
Joint function impairment in PCL-deficient knees correlates positively with chronicity.3–6 A PCL failure over time imposes additional medial compartment forces, resulting in increased pain and joint effusion. Functional limitations become increasingly frequent, especially with coexisting ligament injuries.7,8 Better understanding of PCL biomechanics has led to improvements in clinical evaluation and resulted in earlier recognition of PCL insufficiency. With earlier diagnoses and improvements in PCL reconstruction techniques, surgical indications for this type of injury have expanded markedly.9–13
ANATOMY
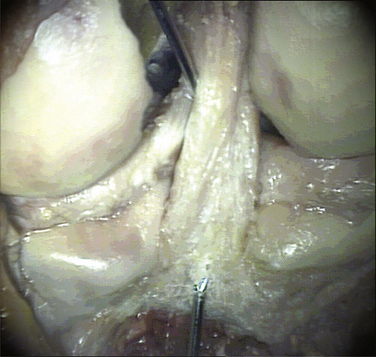
Anatomic descriptions of the PCL vary by degree of detail. The ligament is commonly described as consisting of two fiber bundles, the anterolateral (AL) and posteromedial (PM), with each defined by their relative femorotibial insertion sites, respectively. The anterior section comprises the bulk of the fibers, with the cross-sectional mass almost four times larger than the posterior section. The AL bundle is taut in flexion and becomes lax when approaching extension, whereas the significantly smaller PM bundle is tight in extension (Figs. 25-1 and 25-2) and relaxes toward flexion.14
In close conjunction with the PCL, two meniscofemoral ligaments can be present in some knees. Although their presence can vary, their attachments are uniform. Both ligaments attach distally to the posteromedial aspect of the lateral meniscus. The anterior meniscofemoral ligament (ligament of Humphry) passes diagonally anterior to the PCL and inserts on the lateral aspect of the medial femoral condyle in the roof of the intercondylar notch. The posterior meniscofemoral ligament (ligament of Wrisberg) passes at almost the same angle posterior to the PCL to the femur, blending with the attachment of the posterior longitudinal group of PCL fibers. Literature reviews15–17 have shown that Humphry ligaments are present alone in 25% to 38%, Wrisberg ligaments present alone 39% to 50%, both present in 17% to 20%, and neither in 3% to 8% of knees. Both meniscofemoral ligaments have roles as secondary restraints to posterior tibial translation, which has been noted subsequent to complete transection of the PCL.18,19 With their cross-sectional area at about 10 mm2 and each ligament comprising an estimated 22% of the PCL cross section, the extent of any ligament function potential will vary by the comparative size of the PCL and the presence or absence of either meniscofemoral ligament.
Functional Biomechanics
When the knee is flexed and approaches 45 degrees, the AL bundle fibers tighten and are aligned to resist posterior tibial force. In contrast, the PM bundles exhibit reciprocal behavior, are tight in extension and, when the knee is flexed, begin to slacken. The angle of the PM bundle is not suitable to resist posterior tibial force while tight during knee extension and only provides secondary restraint to resist hyperextension. Once flexion meets or exceeds 120 degrees, the PM bundle femoral attachment moves anteriorly in relation to the tibia so that it is tight and aligned to resist posterior tibial forces, which illustrates its function in deep knee flexion. As complete knee flexion is approached, the AL fibers wrap against the intercondylar notch roof, becoming almost vertical to the tibial plateau, and are thus poorly aligned to control posterior tibial translation. In the presence of collateral ligament and posterolateral corner pathology, PCL injuries have additional rotatory laxity, valgus instability, and posterior tibial translation.20,21
PATIENT EVALUATION
Clinical Assessment
Note that some normal laxity is seen in patients with physiologic genu recurvatum. If posterior translation is normal at 90 degrees but slightly increased at 30 degrees, a PLC injury is likely. Not all patients with PCL tears have a positive posterior drawer test on physical examination.22 Although the PCL is commonly evaluated by performing the posterior drawer test at 90 degrees,23–26 it can also be assessed by other methods, including the dynamic posterior shift test,27 the quadriceps active test, the posterior sag sign, the prone posterior drawer test, and the reverse pivot-shift test.28 Using the quadriceps active test in the presence of a PCL tear, the active contraction of the quadriceps muscle with the knee from 60 to 90 degrees of flexion produces anterior tibial movement and a posterior tibial sag is eliminated.
Diagnostic Imaging
To characterize PCL injury by magnetic resonance imaging (MRI), three planes should be used—axial, coronal, and sagittal. The use of a dedicated knee coil improves signal-to-noise ratio and a small field of view (10 to 14 cm) helps improve spatial resolution.29 The most sensitive views for evaluating the PCL are obtained with the sagittal oblique plane. With MRI, evaluations of PCL tears can be delineated into intrasubstance, partial, complete, or avulsion. Hemorrhage and edema are evident interstitially in intrasubstance tears. Partial tears are evident by interruption of a portion of one of the margins of the ligament and may present a circumferential ring of hemorrhage or edema (halo sign) around the margins. Complete tears have portions of the ligament that are completely absent and may include hemorrhage and edema blurring the margins or in focal areas in lieu of the ligament at tibial or femoral attachments. Avulsions are usually at the tibial insertion and the PCL will retract away with its bone fragment.
Isolated Posterior Cruciate Ligament Injuries
When isolated PLC injury occurs, the following conditions are typically found:
TREATMENT
Conservative Management
In the past, it was assumed that patients with an isolated PCL rupture did well with nonoperative treatment.30,31 Shelbourne and colleagues32 have studied chronic PCL injury nonoperated patients; 170 patients were untreated for their grade II or lower acute isolated PCL injuries. They stated that “…their conditions didn’t deteriorate over time as a group.” However, 20% reported giving way with activities of daily living, 26% reported giving way with strenuous activity, and 54% reported that they did not experience any instability. It is important to note that isolated PCL grade II or lower injuries are atypical. Nonoperative management for isolated PCL injuries (rarely occurring) is not a standard that should be applied universally to multiple ligament injuries.
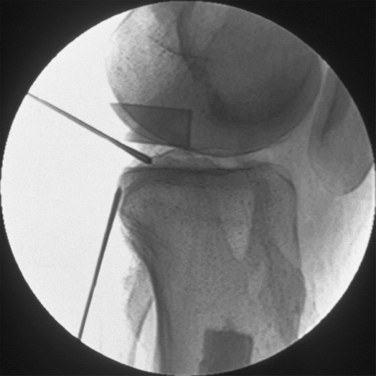
Arthroscopic Technique
Most single-strand techniques attempt to reconstruct the larger anterolateral bundle.33,34 The posteromedial bundle, and the stability it provides in extension, is ignored. Double-bundle techniques have arisen in an attempt to address both the anterolateral and posteromedial bundles.35–37 In vitro research36,38 has suggested that these double-bundle reconstructions can eliminate joint laxity in flexion and extension.