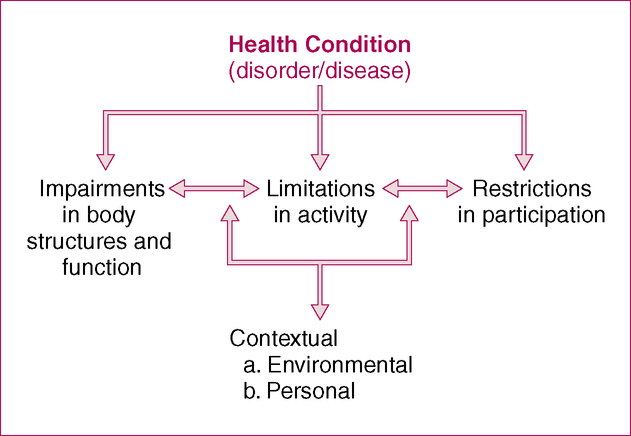
After reading this chapter and completing the exercises, the reader will be able to: 1. Identify and classify various aspects of documenting a patient’s background information and health condition. 2. Explain the three key elements of describing a patient’s current health condition. 3. Discuss the implications of direct access for documenting medical diagnoses. Within the scope of their practice, PTs encounter patients with a variety of health conditions. Health condition, as defined by the ICF framework, is an umbrella term for disease (acute or chronic), disorder, injury, or trauma (Figure 5-1). It may also include other circumstances, such as pregnancy, aging, stress, fitness level, congenital anomaly, or genetic predisposition. Health conditions can result from infections, acute injuries, metabolic imbalances, or degenerative disease processes. In general, health condition information is included early in an evaluation because these data are critical to determining how the PT should proceed with the examination. Therapists perform a process known as differential diagnosis, in which they gather information to confirm or modify any previously determined diagnoses (from other health care professionals) or develop their own diagnosis (see Chapter 9 for more information on diagnosis by PTs). In addition, therapists will ask pathology-related questions, which help identify possible problems that require consultation with or referral to another provider. Certain conditions raise concerns about whether an underlying condition exists in which physical therapy may be contraindicated or in which referral to another health professional would be warranted. In some ways, the health condition information documented by the PT in this section is somewhat limited. At this point, the therapist simply classifies any facts he or she has available before the examination is performed. As the examination proceeds, the PT may uncover information that may help to refine any previously given diagnosis. Any new information obtained during the course of the physical therapy examination that confirms, clarifies, elaborates on, or possibly contradicts the established diagnosis and health condition should be documented in the appropriate section (e.g., Impairments, see Chapter 8) and summarized in the Assessment section (see Chapter 9). Thus information about health conditions and diagnosis does not begin and end in this section. Table 5-1 provides a detailed listing of the types of information that can be included in each of these categories. Case Examples 5-1 through 5-3 at the end of this chapter provide sample documentation in different clinical settings. TABLE 5-1 Components of Documenting Reason for Referral Reason patient is referred, if not evident Concerns that led the patient to seek services of a physical therapist Current and prior therapeutic interventions (if any) Mechanisms of injury or disease, including (see Table 5-2):
Documenting Reason for Referral
Background Information and Health Condition
Documenting Elements of Health Conditions
Component
Information Included
Patient information and demographics
Current condition
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

Documenting Reason for Referral: Background Information and Health Condition,
Only gold members can continue reading. Log In or Register to continue