Distal Radioulnar Ligament Reconstruction
Brian D. Adams
DEFINITION
Distal radioulnar joint (DRUJ) instability may be classified as acute or chronic, unidirectional (volar or dorsal) or bidirectional, and isolated or in association with other injuries.
There is no consensus regarding the definition of clinically significant instability, although various radiographic criteria have been used. In general, the key physical finding is the presence of increased anteroposterior translation of the DRUJ with passive manipulation when compared with the normal side.
Although the radius actually rotates around the stable ulna, by convention, DRUJ dislocation or instability is described by the position of the ulnar head relative to the distal radius.
ANATOMY
The DRUJ consists of the articulation between the ulnar head and the sigmoid notch of the distal radius and the associated supporting soft tissues.
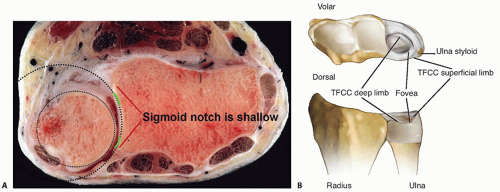
The DRUJ is not a congruent joint, with the radius of curvature of the sigmoid notch being on average 50% greater than the ulnar head. Although the sigmoid notch is shallow, its dorsal and volar rims are typically augmented by fibrocartilaginous extensions that provide important contributions to joint stability (FIG 1A).12 DRUJ surface contact is maximized between neutral and 30 degrees of supination.3
The soft tissue structures that contribute to DRUJ stability are the pronator quadratus, extensor carpi ulnaris (ECU) and its sheath, interosseous membrane, DRUJ capsule, and several components of the triangular fibrocartilage complex (TFCC). Multiple structures must typically be injured to result in joint instability.5
The palmar and dorsal radioulnar ligaments are the prime components of the TFCC that stabilize the DRUJ.10 They are thickenings at the combined junctures of the triangular fibrocartilage articular disc, DRUJ capsule, and ulnocarpal capsule.
As each radioulnar ligament passes ulnarly, it divides in the coronal plane into two limbs. The deep or proximal limbs of the radioulnar ligaments attach at the fovea and the superficial or distal limbs attach to the base and midportion of the ulnar styloid (FIG 1B).
The total pronation-supination arc in a normal individual varies between 150 and 180 degrees. Normal pronation and supination involves a combination of rotation and dorsal palmar translation of the sigmoid notch on the ulnar head.
PATHOGENESIS
The most common cause of DRUJ injury is a fracture of the distal radius.
Distal radius angulation greater than 20 to 30 degrees creates DRUJ incongruity, distorts the TFCC, and alters joint kinematics.1,4 More than 5 to 7 mm of radius shortening results in rupture of at least one of the distal radioulnar ligaments.1
Fractures of the tip of the ulnar styloid are not typically associated with DRUJ instability. Fractures of the base of the ulnar styloid can result in disruption of the radioulnar ligaments, causing DRUJ instability.8
Isolated dorsal DRUJ dislocations (not associated with a fracture) are caused by forceful hyperpronation and wrist extension, such as with a fall on an outstretched hand or the sudden torque of a rotating power tool.
Isolated volar DRUJ dislocations occur with an injury to the supinated forearm, or forceful torque, or a direct blow to the ulnar aspect of the forearm.
NATURAL HISTORY
Delayed diagnosis and treatment of acute DRUJ injuries results in worse outcomes.7
Chronic instability rarely improves spontaneously.
Although there is no proven association between DRUJ instability and the development of symptomatic arthritis, some degeneration should be expected in recurrent dislocations.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients may report falling on an outstretched hand or a forced rotation of the wrist followed by ulnar-sided wrist pain and swelling.
Patients with chronic instability may report a clunk at the wrist during forearm rotation.
Pain and weakness is exacerbated by activities requiring forceful rotation while gripping, such as turning a screwdriver.
Increased passive volar-dorsal translation of the ulna relative to the radius is evidence of DRUJ instability.
When treating an acute distal radius fracture with evidence of DRUJ disruption, the fracture should be reduced and stabilized first, followed by assessment of the DRUJ in comparison with the uninjured wrist.
Distal radius fracture management alone usually provides adequate treatment for the DRUJ.
In the absence of DRUJ arthritis, patients with DRUJ instability typically have full or nearly full wrist range of motion, including flexion, extension, pronation, and supination.
A thorough patient examination should include the following tests:
Passive translation (“piano key” sign). Perform the test and compare results to the unaffected side in pronation, neutral, and supination. A positive test indicates DRUJ instability.2
Modified press test. Increased depression (“dimple” sign) of ulnar head on the affected side indicates instability.2 Pain without increased depression may indicate a partial TFCC tear.6
Passive forearm rotation. A painful clunk indicates joint dislocation and gross DRUJ instability. This should not be confused with more subtle ECU subluxation.
IMAGING AND OTHER DIAGNOSTIC STUDIES
A zero-rotation posteroanterior view is obtained by abducting the humerus 90 degrees, flexing the elbow 90 degrees, and placing the forearm on a flat surface. Signs of DRUJ instability on this view include the following:
Displaced fracture at the base of the ulnar styloid
Fleck fracture from the fovea of the ulnar head
Widening of the DRUJ
Greater than 5 mm of acquired positive ulnar variance compared to the opposite wrist
A true lateral radiograph is performed with the arm at the patient’s side and the elbow flexed 90 degrees. Obtaining a true lateral radiograph is important to avoid inaccurate assessment of DRUJ alignment.
Mino et al9 showed that only 10 degrees of rotation from neutral resulted in an inability to correctly diagnose DRUJ instability on the lateral radiograph.
On a true lateral wrist radiograph, the lunate, proximal pole of the scaphoid, and triquetrum should overlap completely and the volar surface of the pisiform should project between the volar surfaces of the capitate and the scaphoid tuberosity.
Computed tomography (CT) must be performed on both wrists, with axial images obtained with the forearms in identical rotations preferably in neutral and maximum allowed pronation and supination to allow comparison between the normal and symptomatic joints (FIG 2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree