Distal Femur Fractures: Open Reduction and Internal Fixation
Brett D. Crist
Mark A. Lee
INTRODUCTION
The treatment of distal femur fractures is challenging due to disruption of the joint surface, metaphyseal comminution, bone loss in open fractures, and limited space for fixation in fractures with small articular segments. Most distal femur fractures in adults are managed operatively due to poor outcomes with nonoperative management even in elderly patients. High-energy fractures typically occur in younger patients and are associated with open fractures, diaphyseal extension, and intra-articular comminution. Lower-energy fractures usually occur in elderly females secondary to ground-level falls and may be extra-articular or intra-articular. Periprosthetic femur fractures above a total knee or below a total hip arthroplasty create unique problems in treatment. For all of these reasons, fixed-angle devices (including locking plates) and indirect reduction techniques for the nonarticular fracture components have been developed to decrease the need for bone grafting, prolonged external fixation, or medial plating. For the most of these fractures, plate osteosynthesis is the implant of first choice.
INDICATIONS AND CONTRAINDICATIONS FOR SURGERY
While the vast majority of distal femur fractures in adults are managed surgically, there are a few indications for nonoperative treatment. These include truly nondisplaced fractures that can be managed for a short period of time in a cast or hinged knee brace. Occasionally, an impacted stable supracondylar fracture in an elderly patient can be managed without surgery. Similarly, adolescents with open epiphysis and minimally displaced fractures are often well managed in a cast. Lastly, in extremely frail patients with multiple medical comorbidities who do not walk, nonoperative management should be considered.
On the other hand, displaced distal femur fractures that occur in adults are primarily managed surgically to restore stability and allow early range of knee motion and rehabilitation. Even in elderly patients, nonoperative management of displaced fractures is associated with poor outcomes because of an increased risk of pneumonia, deep vein thrombosis, pressure ulcers, and knee stiffness (1).
PREOPERATIVE PLANNING
History and Physical Examination
As with all patients that sustain trauma, a complete history and physical should be performed. Critical factors include mechanism of injury and associated medical comorbidities that might increase the risk of intra- or postoperative complications. These include underlying cardiovascular disease, diabetes mellitus, osteoporosis,
tobacco use, a preexisting surgical history (particularly arthroplasty), and preinjury ambulatory and functional status. A complete physical should include evaluation of the patient, their extremity, pelvis, and spine to avoid missed injuries. Typically the affected lower extremity is shortened and externally rotated. Careful skin inspection and neurovascular exam should be done to avoid missing an open fracture wound posteriorly or neurovascular compromise including compartment syndrome. Ecchymosis and swelling develop rapidly and should be noted. If there is diminished or absent pulses, gentle longitudinal traction should be applied to the lower extremity, and reexamination should be performed to see if the vascular status improves. This often distinguishes whether the difference in the pulse is secondary to fracture displacement or due to an arterial injury that requires vascular consultation. Once the physical examination is complete, either a well-padded long-leg splint or knee immobilizer is applied to relieve pain and provide support to the injured limb. If surgery is delayed, frequent skin and neurovascular checks should be performed. When the fracture is significantly shortened or the patient is not comfortable in a splint or brace, proximal tibial skeletal traction should be considered.
tobacco use, a preexisting surgical history (particularly arthroplasty), and preinjury ambulatory and functional status. A complete physical should include evaluation of the patient, their extremity, pelvis, and spine to avoid missed injuries. Typically the affected lower extremity is shortened and externally rotated. Careful skin inspection and neurovascular exam should be done to avoid missing an open fracture wound posteriorly or neurovascular compromise including compartment syndrome. Ecchymosis and swelling develop rapidly and should be noted. If there is diminished or absent pulses, gentle longitudinal traction should be applied to the lower extremity, and reexamination should be performed to see if the vascular status improves. This often distinguishes whether the difference in the pulse is secondary to fracture displacement or due to an arterial injury that requires vascular consultation. Once the physical examination is complete, either a well-padded long-leg splint or knee immobilizer is applied to relieve pain and provide support to the injured limb. If surgery is delayed, frequent skin and neurovascular checks should be performed. When the fracture is significantly shortened or the patient is not comfortable in a splint or brace, proximal tibial skeletal traction should be considered.
Imaging Studies
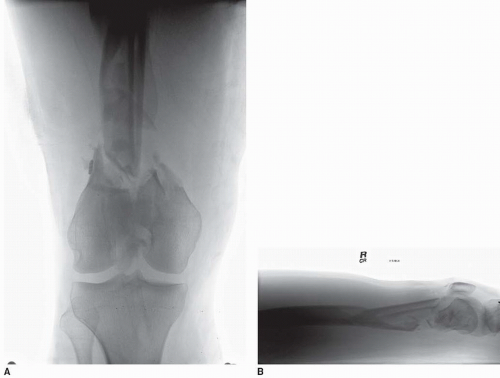
Anteroposterior (AP) and lateral radiographs of the knee and femur are crucial and provide valuable information about the injury and treatment alternatives (Fig. 24.1A,B). Since the fracture is typically shortened and rotated, traction, radiographs can be obtained following appropriate sedation. Full-length femur films are required to avoid missing a more proximal fracture or hip injury. Additionally, bone quality can be assessed on plain films on the basis of the cortical diaphyseal thickness and intramedullary diameter. This information helps guide the choice of implants particularly in the elderly. Computed tomographic (CT) scans with 2D and increasingly 3D reconstructions are obtained for many fractures and virtually all injuries with intra-articular extension.
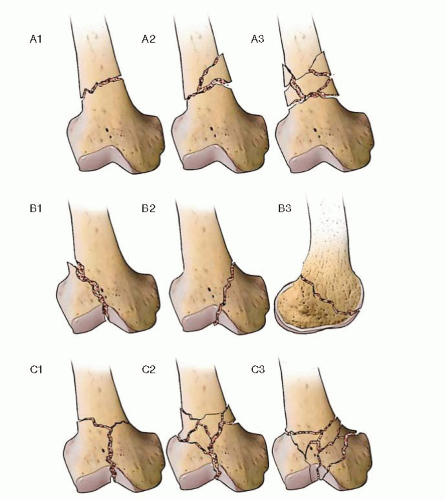
The AO/OTA classification is useful to guide treatment including the surgical approach and fracture implants (Fig. 24.2). The distal femur region is designated as 33 in the comprehensive classification of fractures. Type 33A fractures are extra-articular distal femur injuries and can be fixed with a variety of implants, frequently dictated by surgeon preference. 33B fractures are partial articular injuries and may involve either the medial or lateral femoral condyle. It is mandatory to rule out a coronal plane fracture (B3 component or Hoffa fracture) with even simple supracondylar/intercondylar patterns. This fracture can occur in up to 38% of fractures and if missed leads to poor outcomes (2). It is best seen on the sagittal reconstruction of the CT scan. Type 33C fractures involve both the articular surface and metadiaphysis and range from fairly simple splits to highly comminuted fracture patterns.
We use both plain radiographs and CT scans for preoperative planning. The AP and lateral radiographs of the distal femur are helpful to determine plate length. Many of the high-energy distal femoral fractures with comminution and femoral shaft extension require a total plate length that is two to three times the length of the zone of comminution. It is critical to have a plate of proper length, as short plates are a common cause of fixation failure. Digital imaging software can be used for preoperative planning and to ensure that adequate distal fixation can be achieved with the implant. Finally, we frequently obtain a comparison image of the contralateral femur (if not injured) to determine femoral length when either significant comminution or bone loss exists. This radiograph also determines the normal lateral distal femoral angle (LDFA). Once this is known, the frontal plain reduction angle for the injured side is determined and is used to determine our 95-degree reference path for our implant of choice. Almost all contemporary implants include a 95-degree reference screw or wire to assist in frontal plane reduction and restoration of the LDFA.
 FIGURE 24.3 Sagittal reconstruction CT scan showing coronal plane fracture of the lateral condyle (Hoffa). |
CT scans are very important in preoperative planning for two reasons. First, the CT may reveal unrecognized coronal plane fractures (Fig. 24.3; Hoffa fracture) that usually require independent interfragmentary screw fixation and may affect implant fixation, selection, and location. Second, detailed information is gained regarding the distal extent of the fracture to determine whether or not internal fixation is technically feasible. Current implant designs have increased our ability to gain fixation in increasingly distal fracture patterns, and primary distal femoral replacement arthroplasty is rarely performed today.
Timing of Surgery
To allow for early mobilization, most supracondylar fractures should be surgically repaired as soon as the patient’s overall condition permits, usually within the first 48 hours. Open fractures require urgent irrigation and débridement as soon as operating room resources are available, and the patient is physiologically stable. In patients with open fractures, definitive fixation may be delayed for appropriate imaging, implant availability, and preoperative planning. Staged surgery should also be employed if the soft tissues or patient status or hospital resources preclude early definitive fixation. For most closed fractures in noncritically ill patients, we do not utilize temporary spanning external fixation for distal femur fractures, even for higher energy articular patterns. We favor simple splinting and early definitive internal fixation. This stands in marked contrast to high-energy proximal tibial fractures, where soft-tissue complications are more frequent with early internal fixation (3). Urgent but thoughtful intervention is required, and a detailed preoperative plan remains important especially with intra-articular fracture patterns as this can influence implant selection.
Temporary Spanning External Fixation
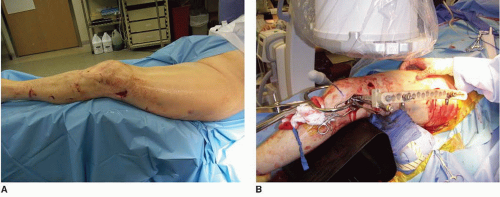
The indications for temporary spanning external fixation have increased over the past 10 years to manage complex extremity fractures in the seriously injured patient. The benefits of temporary external fixation include decreased pain, improved mobilization of the patient, and easier access to the soft tissues when compared to splinting or traction. Furthermore, in complete articular fractures, preoperative planning is improved when radiographs and a CT scan are obtained after closed reduction and external fixation due to ligamentotaxis (Fig. 24.4A,B). The external fixator can also be used intraoperatively as a reduction device.
 FIGURE 24.4 A,B. AP and lateral radiographs of a distal femur fracture placed in temporary knee-spanning external fixator. |
The indications for temporary knee joint spanning external fixation include
Polytrauma patients with multiple orthopedic injuries who are too unstable to undergo definitive fixation
Open contaminated fractures that will require multiple débridements
Closed fractures with significant soft-tissue trauma that precludes early definitive fixation
Complex articular fractures that would benefit from CT imaging after external fixation due to ligamentotaxis
Femoral and tibial external fixation pins should be placed outside of the zone of injury and away from future definitive surgical approaches. Typically, 150- to 200-mm Schantz pins are used in the femur, and approximately 150-mm pins are used in the tibia. Femoral pins can be placed anteriorly, laterally, or anterolaterally. However, if the external fixator is going to be used intraoperatively, a configuration that uses anterior pin placement in the femur is recommended to avoid interfering with plate placement. Furthermore, anterior femoral pin placement avoids any potential contamination of the lateral surgical approach to the distal femur. In order to improve radiographic visualization of the distal femur after external fixation, the bar-to-bar clamps should be strategically placed distal or proximal to the articular surface. The knee should be flexed 10 to 20 degrees to decrease the hyperextension deformity of the distal fragment and relax the posterior neurovascular structures. Standard external fixator pin care should be used. In order to minimize the risk of infection, definitive internal fixation should be performed within 2 weeks whenever possible (4).
Preoperative Surgical Tactic
Once the x-rays and CT scan have been obtained and carefully reviewed, a surgical plan can be developed. Using the tracing technique popularized by the AO or digital templating software, a formal plan should be formulated that includes identifying each fracture fragment that needs reduction and the steps necessary to accomplish it (5). The surgical tactic should describe in detail the procedure from beginning to end. For less experienced surgeons and residents in training, this should include the surgical approach, the equipment required, and the sequence of the procedure including operating room set up, patient positioning; fracture exposure, reduction, and fixation; wound closure and postoperative course. We recommend including specific fracture reduction steps with specific techniques and clamps utilized, provisional fixation, and sequence and location of internal fixation with the specific implants. This ensures that all of the necessary equipment will be available at the time of surgery.
FIXATION DEVICES
Implant selection is dictated primarily by the fracture location and pattern. Extra-articular AO/OTA 33A fractures can be managed with intramedullary nails, traditional fixed-angle implants, or periarticular locking plates. The choice between these implants is largely dictated by surgeon experience and preference as there is little Level I evidence supporting one implant over another. However, a recent study concluded that locking implants may function better in osteoporotic bone than other techniques due to improved fixation in the distal fragment as well as better control of angular stability under physiologic loading (6). Advances in intramedullary nail designs have also improved performance in osteoporotic bone because angular stability is improved by multiplaner fixation with locking options in the distal fragment (Fig. 24.5). Another implant uses a bone-sparing spiral blade in the distal fracture segment with subsequent submuscular plate passage of a plate that is attached to the blade. This type of implant provides the bone-sparing benefit of the first-generation angled blade plates with the submuscular plate techniques seen with modern periarticular locking plates (Fig. 24.6).
Isolated partial articular or AO/OTA 33 type B fractures are uncommon injuries that require internal fixation when displaced conventional nonlocking contoured or traditional buttress techniques are highly effective except in the extremely osteoporotic patients. In this small subgroup, a locking plate is indicated (Fig 24.21A-F).
In North America, the anatomically contoured periarticular locking plates have become the treatment of choice for most intra-articular distal femoral fractures (AO/OTA type C). These systems combine the ability to use both locking and nonlocking screws (hybrid technique) that have addressed many of the major limitations and concerns about the first-generation locking plates such as the Less Invasive Surgical Stabilization (LISS; Synthes, West Chester, PA). The multiple fixed angle screw design provides secure fixation in the distal articular block that can be advantageous in osteoporotic bone or short articular segments. Additionally, multiple points of angular stability can provide fixation around independent articular lag screws. Newer generation multidirectional locking plates allow screws to be directed through an arc of up to 20 degrees in each direction and precisely direct screws around other distal fixation (Fig. 24.7A,B). This has been shown to provide reliable angular stability in bridging constructs (7). Most of the current generation of locking implants includes insertion handles and aiming arms that facilitate percutaneous screw placement along the femoral shaft.
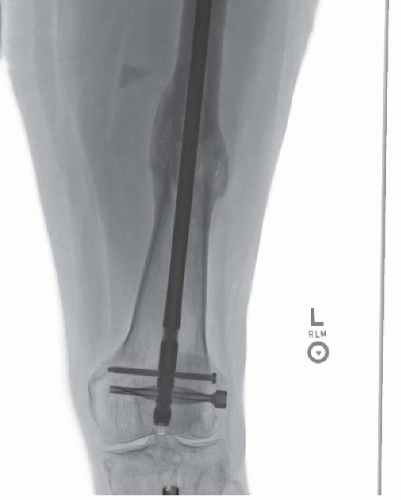 FIGURE 24.5 AP radiograph of a femoral shaft fracture managed with a retrograde femoral nail with fixed-angle blade fixation distally. |
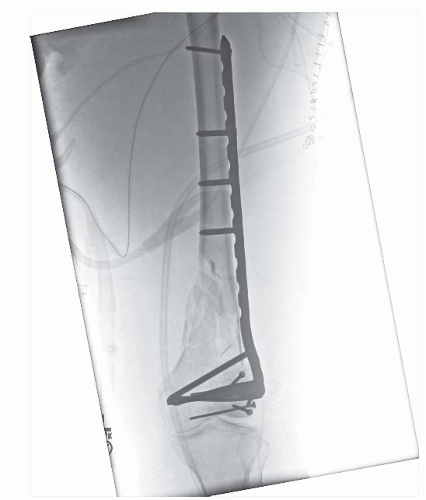 FIGURE 24.6 AP knee radiograph showing comminuted intra-articular distal femur fracture managed with a modular blade plate. |
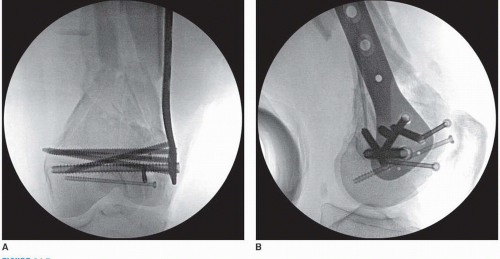 FIGURE 24.7 A,B. AP and lateral knee fluoroscopy views showing multidirectional locking screw fixation used to avoid lag screws placed across the articular fragments. |
Surgical Technique
The patient’s condition and medical comorbidities often influence whether a general or spinal anesthetic is recommended. We prefer general anesthesia to ensure reliable and sustained muscle paralysis that is required for fracture reduction and fixation. Standard antibiotic prophylaxis is utilized. Appropriate blood products should be available, and an arterial line should be considered in unstable patients or if a prolonged procedure is expected. A Foley catheter is utilized in most patients.
Patient Positioning
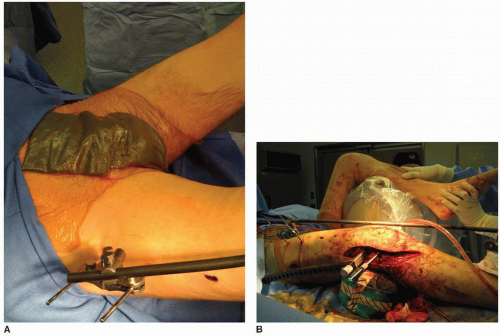
Internal fixation of distal femur fractures is done on a radiolucent table that allows for unobstructed imaging from the pelvis to the foot. The patient is placed supine on the operating table with a small bump placed beneath the ipsilateral hip to allow the leg to lie in neutral rotation (Fig. 24.8A).
The entire lower extremity should be prepped and draped from the iliac crest to the toes to allow for accurate intraoperative assessment of length, alignment, and rotation. In fractures with significant comminution or bone loss, we often include the contralateral extremity in the operative field for comparison and easier fluoroscopic access to the proximal femur for the lateral view (Fig. 24.9). Sterile bumps or towels, custom ramps, or radiolucent triangles can be used to help position the leg (Fig. 24.8B). In very distal fractures, a sterile tourniquet can be used, but for most fractures, it is not applicable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree