Chapter 37 Distal Biceps and Triceps Tendon Ruptures
Distal biceps tendon ruptures
Introduction
Distal biceps tendon ruptures are relatively uncommon injuries with a reported incidence of 1.2 per 100 000 people.1 They comprise 3–12% of all biceps injuries2 with the dominant arm affected in 86% of cases. The average age at presentation is around 50 years with a range from the second to the eighth decade.3 Recognized risk factors include male gender, smoking,1 anabolic steroid use4 and body building/weight lifting.2 Distal biceps tendon ruptures are often debilitating injuries and recovery can be time consuming and incomplete. Surgical repair techniques have traditionally been associated with high complication rates but recent advances have resulted in more favourable outcomes.
Background/aetiology
Anatomy
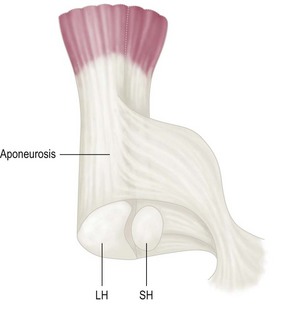
The two fleshy bellies of the biceps muscle lie side by side as they pass down the anterior aspect of the arm loosely connected by areolar connective tissue. The long head and short head of the biceps have separate distal tendons with defined footprints onto the radius.5 Both are ensheathed by the bicipital aponeurosis (lacertus fibrosus) that consists of three layers (Fig. 37.1). The long head passes radial to the short head and makes up the bulk of the distal biceps tendon inserting proximally on to the radial tuberosity. The short head inserts just distal to this in a fan-like fashion. A bursa lies between the tendon and the anterior part of the tuberosity. At the cubital fossa, the bicipital aponeurosis (lacertus fibrosis) comes off the medial aspect of the distal biceps tendon to insert into the subcutaneous border of the ulna via the deep fascia of the forearm.
Pathophysiology
The pathophysiology of distal biceps tendon ruptures remains unclear despite numerous hypotheses having been proposed. Davis and Yassine believed that the presence of a bony prominence or irregularity of the radial tuberosity resulted in rupture.6 The proposed mechanism was that hypertrophic lipping on the anterior margin of the radial tuberosity led to friction at the insertion of the biceps tendon resulting in a minor tear in the tendon. This tear would then extend as the tendon was pulled against this knife-like projection.
Morrey suggested that the presence of radial bursitis played a role in weakening the tendon.7 Seiler et al also proposed that weakening of the tendon predisposed to tendon rupture but suggested that this was due to a watershed area in the arterial supply.8
The tendon most commonly tears at its insertion. Tears within the length of the tendon and at the musculotendinous junction are rare.9 Schamblin and Safran presented the largest series of musculotendinous tears of the distal biceps brachii with a total of six patients over 2 years. Although most tears are full thickness, partial thickness tears can also occur.10 The proximal portion of the tendon is more likely to retract into the brachium if the bicipital aponeurosis is also torn.
Summary Box 37.1
Presentation, investigation and treatment options
History
The patient with a tear of the distal biceps brachii tendon will usually give a history of having sustained an unexpected, sudden and sharp extension load to an elbow flexed at 90° with the biceps brachii in a contracted state (eccentric contraction). This is followed by a sharp sudden pain, typically in the antecubital fossa, but sometimes felt in the posterolateral elbow, which then subsides. The patient may give a history of having heard an audible ‘pop’. The patient will usually report a sensation of immediate weakness of elbow flexion, which may then subside. Commonly the patient experiences ongoing weakness and dull pain on supination and flexion of the elbow particularly with physically demanding activities.3
Examination
The examination findings of a partially ruptured distal biceps tendon are more subtle. Clinical examination will reveal a palpably intact biceps tendon, although there may be tenderness over the radial tuberosity. Crepitus or grinding on passive supination and pronation of the forearm10 may also be present together with weakness and pain when assessing supination strength against resistance.
Several clinical tests have been described to aid the diagnosis of distal biceps tendon rupture. The senior author’s preference is to simply perform passive rotation of the patient’s forearm with the elbow flexed to 90° and observe the biceps muscle belly. If there is no movement a complete rupture is likely. Ruland et al have described a squeeze test which they report to have 96% sensitivity for diagnosing a complete distal biceps rupture.11 The patient should be seated with the elbow flexed to 60° and the forearm in slight pronation. The surgeon squeezes the biceps muscle belly with both hands, drawing the muscle away from the humerus. Forearm supination should be observed if the distal biceps is intact.
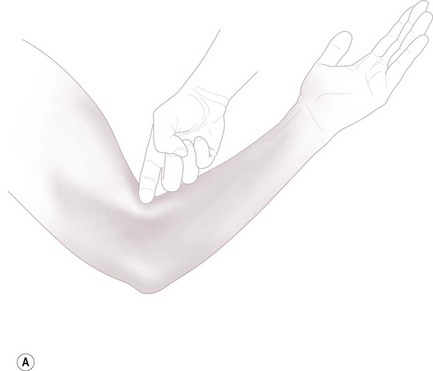
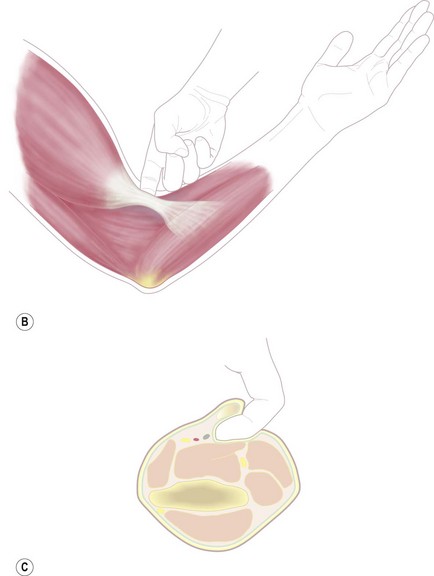
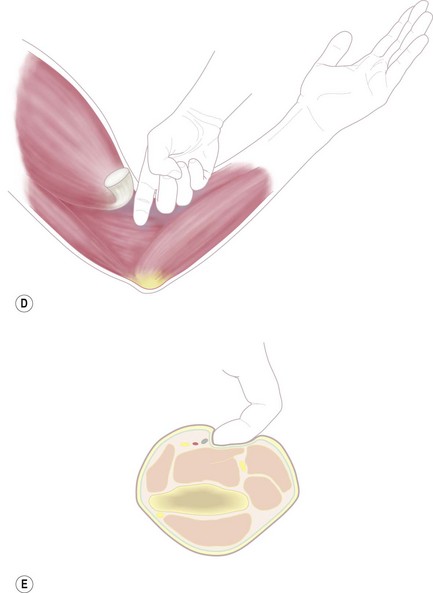
O’Driscoll described the hook sign which is pathognomonic for distal biceps tendon tears (Fig. 37.2). The patient is asked to actively flex the elbow to 90° and actively supinate the forearm. The examiner is then able to hook their finger under the distal biceps tendon from the lateral aspect of the elbow. In the case of a complete rupture of the distal biceps tendon, the examiner is unable to satisfactorily hook their finger under the cord-like tendon.12
ElMaraghy and Devereaux described the measurement of the biceps crease interval as a diagnostic examination.13 The patient begins with a flexed elbow and slowly extends it allowing the examiner to identify the position of the elbow flexion crease. This is marked with a pen. The examiner then runs a finger along the long axis of the biceps belly and identifies the point at which it most sharply turns downwards towards the elbow. This point is also marked. A distance between these points of greater than 6 cm was found to be reliably predictive of a complete tear of the distal biceps tendon. Further, the biceps crease ratio can be ascertained by measuring the biceps crease interval on the contralateral arm and comparing the result. Here it was found that a ratio of greater than 1.2 was reliably predictive of a complete tear of the distal biceps tendon.
Summary Box 37.2
Imaging
Plain radiographs, although important as a primary investigation to assess trauma to the elbow, are not particularly helpful in the diagnosis of distal biceps tendon ruptures. The only positive radiographic finding may be irregular changes in the shape of the radial tuberosity that may predispose the patient to a biceps tendon rupture. Regardless of this, X-ray findings will not significantly affect management decisions.14
Ultrasound has been used to diagnose distal biceps tears. The advantages of this technique are that it is relatively inexpensive, widely available and the contralateral side can be easily imaged for comparison. In addition dynamic imaging may be helpful in revealing partial tears of the distal biceps tendon.15 However it is a less reliable investigation when compared with magnetic resonance imaging (MRI), is unlikely to demonstrate any other pathology that may be present in the elbow and is operator dependent.
In order to obtain maximum information from the MRI scan, however, the patient must be appropriately positioned in the scanner. The anatomical course of the biceps tendon makes acquisition of clear images difficult and, although patients are most comfortable in a supine position with their arms by their sides, this can interfere with fat suppression due to the off axis position of the arm. Giuffrè and Moss15 described a patient position that enables a longitudinal view of the tendon to be obtained in one slice. This allows easier recognition of pathology and is described as the FABS view (flexed, abducted and supinated view). The patient lies prone with the shoulder abducted to 180°, the elbow flexed, and the forearm supinated (Fig. 37.3). This position results in acquisition of superiorly fat-suppressed images and a clear view of the distal biceps tendon (Fig. 37.4).

Figure 37.3 The FABS view allows procurement of a longitudinal view of the biceps tendon on MRI.
(With permission from Giuffrè BM, Moss MJ. Optimal positioning for MRI of the distal biceps brachii tendon: flexed abducted supinated view. AJR Am J Roentgenol 2004; 182:944–946.)
Biceps tendon endoscopy is a minimally invasive diagnostic tool that enables direct examination of the distal biceps insertion (Fig. 37.5). The procedure, described by Eames and Bain16 is most useful in the investigation of partial tears. A small 2.5 cm incision is made longitudinally over the palpable biceps tendon about 2 cm distal to the elbow skin crease. The lateral cutaneous nerve of the forearm is identified and protected. The surgeon uses a finger to palpate the tendon and the bursa. The bursa is then insufflated with 7–10 mL of normal saline, and kept insufflated with a gravity feed. A small entry point is made on the radial side of the bursa to allow access of the arthroscope. The tendon can then be visually followed to its insertion. This technique allows excellent visualization not only of partial tears of the tendon, but also other pathology such as synovitis and bursitis. The introduction of a hook probe will further assist in the assessment of the biceps insertion. Dynamic assessment of the tendon can also be undertaken by pronating and supinating the forearm.
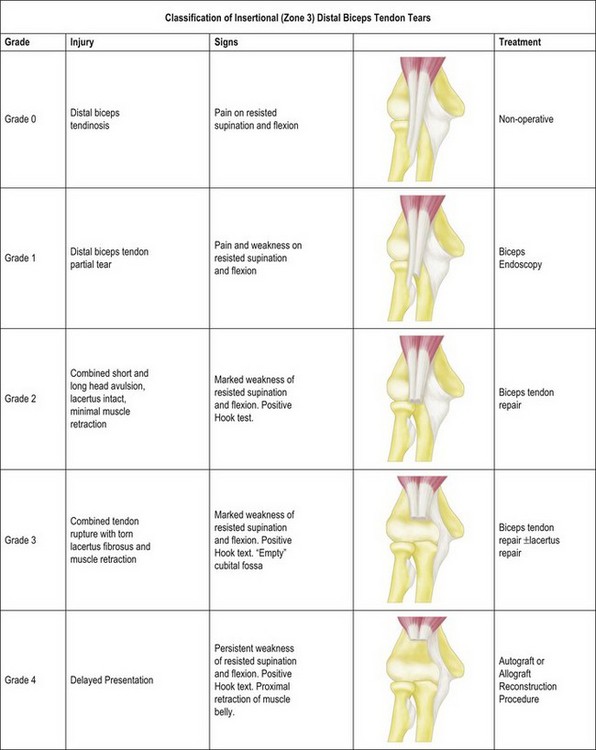
Classification
Distal biceps injuries can be classified: (i) temporally (acute or chronic), (ii) according to degree (partial or complete), or (iii) anatomically (the distal biceps tendon can be divided into three zones in relation to the aponeurosis: zone 1 – pre-aponeurotic (musculotendinous junction), zone 2 – aponeurotic, zone 3 – post-aponeurotic (tendon-bone interface). Most injuries occur in zone 3 at the tendon–bone interface. We have devised a classification for these injuries based on the degree of injury and the chronicity that we use to guide our management (Fig. 37.6).
Surgical techniques and rehabilitation
Treatment – partial thickness ruptures
Partial thickness ruptures of the distal biceps tendon have a variable prognosis. The patient is advised to avoid heavy activity and is prescribed non-steroidal antiinflammatory drugs. In addition, a rehabilitation programme of stretching and strengthening exercises is commenced. This treatment is more effective for tears of less than 50% of the tendon. Patients with lower demands are likely to have a successful outcome.3 If this approach fails, however, and pain and limited function persists, operative intervention is indicated. Debridement of the distal biceps tendon has been described, but this may have limited success in improving the symptoms.17 A more successful outcome can be expected by detaching, debriding and then reattaching the distal biceps tendon (see operative techniques below).18,19
Treatment – full thickness ruptures
Full thickness ruptures of the distal biceps tendon usually require operative intervention since conservative treatment is associated with permanent loss of supination strength.10,20 Non-operative management may be considered for very low demand patients or if there is a high surgical morbidity or mortality risk due to the patient’s comorbidities.
Historically, distal biceps tenodesis to the brachialis was performed but anatomical repair to the radial tuberosity using a two-incision technique or a single small anterior incision is now preferred.21
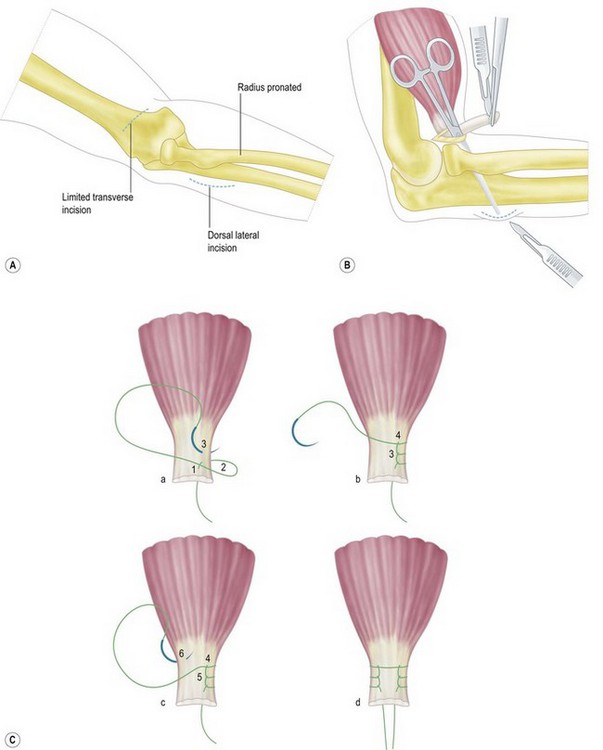
Operative techniques – two incision
The initial approach uses a 3–4 cm transverse incision over the antecubital fossa. Dissection is continued through the deep fascia, protecting the lateral cutaneous nerve of the forearm. The proximal portion of the torn distal biceps tendon is retrieved and trimmed after which two grasping stitches (e.g. Bunnell) are inserted using non-absorbable suture material (Fig. 37.7).
Failla et al highlighted the risk of radio-ulnar synostosis using the two-incision technique, and recommended a limited muscle splitting approach through the extensor muscle mass without exposing the ulna.22 Mazzocca et al advocated the aggressive use of lavage to minimize the risk of heterotopic ossification and synostosis.23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree