Chapter 22. Disorders of the shoulder and elbow
Shoulder
Recurrent dislocation of the shoulder
Acute dislocations of the shoulder are described on page 192. Although most shoulders in elderly patients remain stable after reduction, some dislocate repeatedly with trivial trauma, especially those with ligamentous laxity. The dislocations can be anterior, posterior, inferior or multidirectional, but anterior dislocation is by far the commonest.
Recurrent anterior dislocation
Recurrent anterior dislocation happens when the shoulder is fully abducted and externally rotated, which brings the head of the humerus against the weak inferior joint capsule (p. 193). This position, in which the arm is above the head and the hand facing forwards, occurs when swimming backstroke, reaching for a ball in a rugby line-out, or reaching into the back seat of a car from the front (Fig. 22.1). Patients with ligamentous laxity or those where there is a Bankart lesion (disruption of the anterior glenoid labrum and capsule) are most at risk.
 |
| Fig. 22.1 Movements that can dislocate the shoulder. |
Occasionally the humeral head may be fractured, giving a flat appearance or a hatchet-like deformity on radiographs (Hill–Sachs lesions).
Treatment
The dislocation can usually be reduced easily and many patients are able to reduce their own shoulders. Some learn to avoid dislocations and do not want operation, but others are disabled by their instability, and surgery must then be considered (e.g. Fig 22.2). Unfortunately, in young patients there is a significant chance of recurrence (up to 90%); recent trials of early surgery in these patients have shown a reasonable reduction in the subsequent dislocation rate.
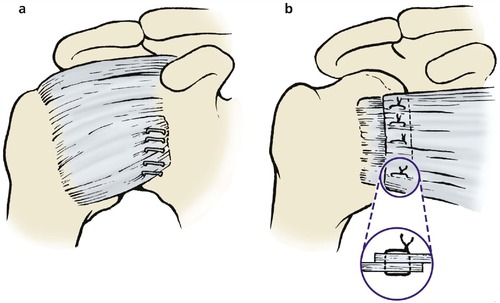 |
| Fig. 22.2 Operations for recurrent dislocation of the shoulder: (a) reattachment of the inferior corner of the capsule; (b) shortening of the subscapularis tendon. |
Methods of correcting recurrent anterior dislocation of the shoulder include:
1. Tightening the inferior pouch of the joint capsule (by open surgery or arthroscopic surgery and/or electrocautery).
3. Tightening the subscapularis muscle to limit external rotation (Putti–Platt operation).
4. A bone block on the glenoid neck.
5. A combination of these.
After operation, the arm is bandaged to the side for 3 weeks. The forearm can then be released to allow rotation, and physiotherapy begun. The results are generally satisfactory.
Recurrent posterior dislocation
Recurrent posterior dislocation is less common than anterior dislocation and is often seen as a ‘party trick’ in teenagers with loose joints. The same patients can usually click their jaws and do weird tricks with their thumbs. The humeral head can become ‘locked’ behind the glenoid (Fig. 22.3).
 |
| Fig. 22.3 Locked posterior dislocation of the shoulder in a patient with a humeral head defect. |
Acute dislocations are described on page 192.
Treatment
The basis of treatment is to tell the patients not to do it on purpose, in the hope that they will learn to avoid the movements that cause the dislocation. It is very rare for recurrent posterior dislocation to cause enough disability to warrant stabilization. If operation is required then either a posterior bone block or a glenoid osteotomy will be needed. Both these operations are formidable and very unreliable.
Internal derangements of the shoulder
The glenoid labrum, like a meniscus in the knee, can be torn or detached at its rim and cause painful clicking or catching within the joint. Lesions of the superior labrum adjacent to the biceps tendon are described as SLAP lesions (SLAP = superior labrum anterior posterior). These occur when the superior glenoid labrum is avulsed or detached from the glenoid. Loose bodies and irregularities of the articular surface produce similar catching and clicking symptoms. MRI scans and, previously, arthrograms are very useful for identifying the lesion.
Treatment
The vast majority of these lesions are now dealt with arthroscopically. Labral lesions can be reattached with sutures or absorbable fixation devices. Loose bodies and chondral lesions are easily seen and removed with the arthroscope.
Supraspinatus tendinitis
The supraspinatus tendon passes through the narrow tunnel between the acromion and the head of the humerus and may degenerate or become inflamed where it crosses the humeral head (Fig. 22.4). With the resultant impingement between the humeral head and the acromion, the affected area of the tendon swells and causes pain during active abduction. The pain goes as soon as the sensitive area has passed through the tunnel. Because the pain is present in a small arc of movement only, usually between 60 and 120° of abduction, the condition is sometimes known as ‘painful arc syndrome’.
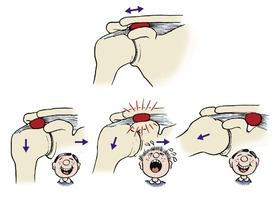 |
| Fig. 22.4 Supraspinatus tendinitis and painful arc syndrome. An inflamed and swollen area of the supraspinatus tendon causes pain as it passes beneath the acromioclavicular joint. |
The diagnosis can be confirmed by comparing passive movement with active. When the shoulder is moved passively there is no pressure on the tendon and movement is painless. During active movement the tendon is compressed against the humeral head and this is painful.
There are effectively three stages of this tendinitis, depending on the severity of the inflammation: stage 1, microscopic changes in the tendon; stage 2, oedema of the tendon; and finally, stage 3, where the tendon starts to rupture and tear.
Treatment
In the early stages, rest and avoidance of activities provoking the inflammation may be sufficient, but with prolonged or severe cases an injection of 25 mg of hydrocortisone acetate and local anaesthetic placed around the tendon (but not into it) is effective in most patients. The injection is given with the arm hanging and the patient sitting and supported. The needle is placed either beneath the acromion from its lateral end or posteriorly in the line of the tendon. In recalcitrant cases that fail to settle with appropriate conservative treatment, or where the supraspinatus tendon has torn, then surgery may be necessary. Arthroscopic (or open) surgery to remove the spur on the under-surface of the acromion or inferior surface of the acromioclavicular joint has a good prognosis, although the recovery for this may be prolonged. Occasionally the acromioclavicular joint needs to be excised. The aim of the surgery is to allow increased room for the inflamed tendon to pass under the acromion without impingement. By removing the cause of the impingement, the tendon will hopefully heal. Where there is a tear of the tendon this can again be repaired to bone or side to side, either arthroscopically or via an open approach. The advantage of arthroscopic procedures is the shortened recovery time postoperatively.
Acute calcific supraspinatus tendinitis
If the symptoms of supraspinatus tendinitis come on rapidly over a period of hours and the pain is intense, radiographs may show a patch of calcification within the tendon, often adjacent to its insertion on the humeral head. It is frequently described as one of the worst pains imaginable. The patients are usually in the second or third decade of life and the condition is probably a variation of crystal arthropathy (p. 305




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








