Chapter 24. Disorders of the hip and knee
Osteoarthritis of the hip
Clinical features
Osteoarthritis of the hip is one of the commonest causes of disability in the western world. The condition is essentially mechanical wearing out of the hip joint rather than a disease and can be caused by many things. Trauma, obesity and previous infection can all be followed by osteoarthritis but there is probably a genetic element as well. The disease is much less often seen in Asiatic races.
The characteristic symptoms are:
1. Pain.
2. Loss of hip movement.
3. Abnormal gait.
Pain. The pain is worse on weight-bearing and movement of the hip but also occurs at rest and disturbs sleep. The pain is dull and aching in character at first but becomes sharper as the disease progresses.
The pain is usually felt in the groin but pain down the outer side of the thigh is also common. Some patients also have pain low in the thigh, around the knee, and become convinced that the trouble lies in the knee, not the hip. Referred pain of this type is a well-known diagnostic pitfall but still confounds the unwary.
Loss of movement. Movement is lost because osteophytes form around the joint and change the shape of the joint surfaces. As movement is lost, a flexion, adduction and external rotation deformity develops. The flexion deformity is compensated for by hyperextension of the lumbar spine, and this can cause backache. The adduction deformity causes apparent shortening of the leg and patients often complain that ‘my leg is getting shorter’.
The stiffness makes it difficult to tie shoe-laces, put on socks or cut toenails.
Abnormal gait. The limp is due partly to the restriction of movement in the joint, and partly to an antalgic gait (p. 25); i.e. walking so that the load on the hip joint is reduced. The limp is usually observed by other people rather than the patient but a few are more worried by the limp than anything else.
Clinical examination
Patients with osteoarthritis of the hip are ideal subjects for the clinical section of final medical examinations, and it is only the most foolhardy student who will attend the examination without being able to examine the hip easily and confidently.
Radiology
Osteoarthritic hips show characteristic radiological changes (Fig. 24.1).
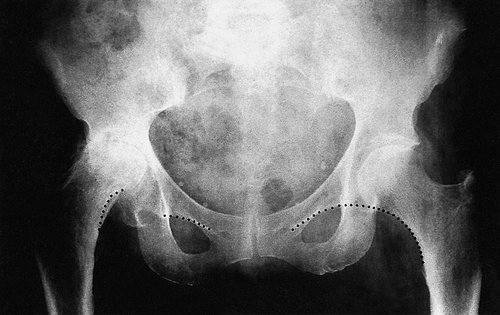 |
| Fig. 24.1 Osteoarthritis of the hip showing joint space narrowing, cyst formation, subchondral sclerosis, osteophytes, thickening of the femoral head and bone destruction. Shenton’s line (dotted) shows collapse of the femoral head. |
Radiological changes in osteoarthritis of the hip
1. Narrowing of the joint space.
2. Cyst formation in the femoral head and the acetabulum.
3. Sclerosis of subchondral bone.
4. Osteophyte formation.
5. Subcortical thickening on the medial side of the femoral neck.
6. If there is bone destruction as well, Shenton’s line will be disturbed, indicating true shortening of the limb.
Pathology
Osteoarthritis of the hip begins with fibrillation of the articular surface and the formation of wear particles. The wear particles are swept to the side of the joint where they irritate the synovium and are responsible for some of the patient’s pain and the formation of osteophytes.
As the disease progresses, articular cartilage is lost, subchondral bone is exposed and the bone surfaces become eburnated (Fig. 24.2). Grooves form in the joint surfaces and the hip is gradually converted from a ball and socket into a roller bearing. Later, cysts form in the bone and the femoral head may collapse.
 |
| Fig. 24.2 Osteoarthritic femoral head. |
Untreated, the hip becomes fixed in flexion, adduction and external rotation, a position which interferes seriously with mobility.
Treatment
The conservative treatment of osteoarthritis of the hip includes the following:
Conservative treatment of osteoarthritis of the hip
Conservative treatment of osteoarthritis of the hip
1. Anti-inflammatory drugs.
2. Weight reduction.
3. A stick, which is only helpful if it is held in the opposite hand and used correctly.
4. A raise to the shoe of the shorter limb to correct the apparent shortening and relieve the abnormal strain on the lumbar spine and opposite hip.
5. Aids to daily living to help the patient put on shoes and stockings and pick up dropped articles.
All these measures are important and must be considered, even if not adopted, before operation is recommended. There is some evidence that an arthroscopic washout and debridement is useful in the early stages. The results of this in established osteoarthritis of the elderly are poor.
Rheumatoid arthritis of the hip
As elsewhere, rheumatoid arthritis destroys bone, but the osteophytes and sclerosis of osteoarthritis are usually absent. Instead, the femoral head is gradually eroded or collapses suddenly, resulting in true shortening of the leg (Fig. 24.3).
 |
| Fig. 24.3 Rheumatoid arthritis of the hip. Note the thinning of the medial wall. |
Treatment
If conservative measures fail, joint replacement is the only effective treatment. Rheumatoid patients do well because their activity is limited by disease elsewhere and also because they are generally lightweight.
Total hip replacement
Total hip replacement is the most popular operation for osteoarthritis of the hip and consists of replacing both surfaces of the joint with artificial materials (Fig. 24.4). The acetabulum is reamed out to take a cup and the femoral head replaced with a metal ball attached to a stem inserted in the femoral shaft. A resurfacing component that does not use a long stem has recently been introduced and is often used in younger patients to prevent bone loss (Fig. 24.5).
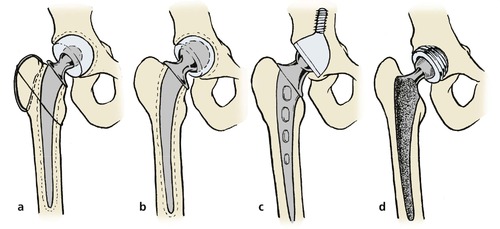 |
| Fig. 24.4 Types of total hip replacement: (a) Charnley hip replacement with greater trochanter reattachment; (b) Müller type replacement with larger femoral head; (c) ring-type replacement using a long, threaded acetabular component without cement; (d) uncemented prosthesis with sintered surfaces and screw-in acetabular prosthesis. |
 |
| Fig. 24.5 Hip resurfacing components. |
There are many types of hip replacement but most have a femoral component made of either stainless steel or a chrome cobalt molybdenum alloy and a cup made of high density polyethylene. Both components are usually fixed to the skeleton with cold curing acrylic cement (p. 49 and p. 299). Metal on metal articulation is possible and reduces the amount of wear debris within the hip capsule, as do ceramic bearings.
Some prostheses are inserted without cement, fixation relying on bone growing into irregularities on the surface of the component. The size and shape of the pores into which bone can grow is critical in securing fixation. A covering of hydroxyapatite may enhance this ingrowth; ceramic components are also used and new designs are continually being introduced.
Of the many different types of hip replacement, the Charnley low friction arthroplasty, the Exeter and the Stanmore are the best known (Fig. 24.6 and Fig. 24.7).
 |
| Fig. 24.6 A Charnley hip prosthesis. |
 |
| Fig. 24.7 A Charnley total hip replacement. |
The friction in most total hip prostheses is about 40 times greater than that of a normal healthy hip and this imposes a strain on the fixation of the components to bone. Furthermore, the rigid femoral stem causes stress risers in the femoral shaft.
Types of total hip prosthesis
• Cemented. In this, the most commonly used type, the components are fixed to bone with an acrylic cement. The acrylic cement can cause bone destruction if the components become loose, e.g. Charnley. Designed by Sir John Charnley, this prosthesis has been used since the late 1960s. It is made of stainless steel, has a small femoral head, a high density polyethylene cup and is secured with acrylic cement.
• Hybrid. In this, only one of the components is fixed by cement.
• Isoelastic. The femoral stem is designed to have the same flexibility as bone in order to minimize stress risers within the femoral shaft. These have not been shown to offer any great advantage.
• Ceramic. The bearing surfaces are made of aluminium oxide. Mechanical characteristics are good but the components can crack and ceramic particles may be irritant.
• Resurfacing. Use of a metal on metal articulation without a long femoral stem (Fig. 24.8).
 |
| Fig. 24.8 A metal on metal hip resurfacing component. |
Results
The results of total hip replacement are spectacular, with good or excellent results in approximately 98% of patients. The operation is most successful in relieving pain but some restoration of movement and an improved gait can also be expected.
The results are so good that the operation has revolutionized hip surgery and brought treatment to many who would otherwise have been untreatable. This has in turn brought great pressure on the resources available for orthopaedic surgery.
Indications
The ideal patient for total hip replacement is a lightweight elderly patient who has severe pain and places few demands on the hip. The most unsuitable is a young, heavy, active man who wants to play football and return to heavy work. Between these two extremes the degree of pain and disability is weighed against the patient’s age and physical requirements but, in general, total hip replacement should not be offered to the following types of patient:
1. Those under the age of 60.
2. Those who are obese.
Technique
The operation can be done in several ways and through several approaches. These include:
1. The anterolateral approach, between tensor fasciae latae and the glutei.
2. The posterior approach through the posterior capsule.
3. The Charnley approach with detachment of the greater trochanter.
4. Detachment of the glutei and a portion of the vastus lateralis muscle.
With all these approaches the principle is the same. The acetabular surface is prepared by removing all debris and soft tissue and the femoral head is removed. The acetabulum is then replaced with a prosthetic component, which is fixed either mechanically or with bone cement. The femoral component is then inserted and similarly secured.
Prevention of infection
Infection in a prosthetic hip is a disaster and great care must be taken to prevent it occurring during operation by the following measures:
1. Meticulous asepsis during operation, or
2. Prophylactic antibiotics, or
3. A combination of the two.
Aseptic techniques. Meticulous asepsis in an operating enclosure with ultraclean air changed continuously and impervious operating gowns with individual exhaust systems for expired air (Fig. 24.9) can reduce the infection rate to 0.2%, but the operations may also be done in a standard operating theatre.
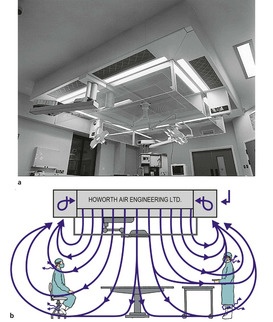 |
| Fig. 24.9 (a) Modern version of the world’s first clean air enclosure for surgery – the Charnley Howorth Exflow Ultra-Clean Air System. (b) The flow of air using an ultraclean system with exponential flow. By kind permission of Howorth Airtech. |
Prophylactic antibiotics used in a standard operating theatre will produce a similar infection rate to the operating enclosure. A regimen of flucloxacillin 500 mg started with the premedication and continued for three doses is effective. If the patient is allergic to penicillin, vancomycin may be used.
Combining antibiotics with a clean air enclosure can reduce the infection rate still further.
Catheterization. Inserting catheters immediately after operation runs the risk of infection. If it cannot be avoided, catheterization should be done gently with complete sterility and covered with an appropriate antibacterial drug.
Cross-infection. Patients with clean joint replacements should not be nursed in the same ward as those with abscesses, colostomies or open infection.
Postoperative care
Some surgeons prefer to hold the hip in abduction by placing a wedge-shaped pillow between the patient’s thighs for 2 days. This is particularly helpful if a Charnley hip prosthesis with a small femoral head has been used.
The suction drains are usually removed after 2 days, when the patient may sit out of bed. They should not sit in a low chair because this flexes the hips beyond 90° and can, in some circumstances, cause the hip to dislocate. Most patients should mobilize the next day with a frame and be walking reasonably with elbow crutches, ready for discharge, after 4–5 days. By then the patients should be able to climb stairs and be able to cope with many activities of daily living.
Between 6 and 12 weeks after the operation most patients have little pain from their hip and an improved range of motion that allows them to resume normal activities. However, heavy work, especially lifting and jumping, should be avoided indefinitely in case it stresses the bone–cement interface.
Failure
Not all hip replacements are successful and it is estimated that between 0.5% and 1% of all hip prostheses in position fail each year because of infection or loosening (Fig. 24.10).
 |
| Fig. 24.10 Early McKee–Farrar prosthesis with loosening and fracture of the pelvis. |
Early infection around a total hip replacement almost invariably leads to failure and special care is needed to avoid infection at the time of operation.
Late infection can also occur later via the bloodstream from infections in the urinary tract or elsewhere.
The organisms responsible for infection around total hip replacements include many normally regarded as non-pathogenic, e.g. Staphylococcus epidermidis. The explanation is unknown but it may be that these bacteria flourish in the unusual tissue that surrounds prosthetic materials (glycocalyx), or that the minute amount of metallic salts leaving the prostheses inhibits macrophage activity.
Loosening. Acrylic cement is strong in compression but weak in shear and torque. It causes little soft tissue reaction as long as it is intact but in particulate form it initiates a foreign body reaction that destroys bone. These two factors put together mean that violent twisting stresses may split the cement and allow the two surfaces of acrylic to ‘fret’, creating wear particles which destroy bone, cause more loosening, more fractures in the cement, and failure of the bone–cement interface.
In many ways, a hip prosthesis can be compared with a fibreglass patch on an old car; the repair is perfect as long as the car remains in the garage but it will loosen if driven hard over a bumpy road. The analogy is apt because the cement used in hip surgery is similar to that used for car repairs.
From the clinical standpoint, loosening usually affects the femoral component in active and overweight patients and causes pain on weight-bearing and hip movement.
Pain in the thigh usually indicates loosening of the femoral component, pain in the groin loosening of the acetabular component. The patient does not feel the components moving within the bone until the loosening is very severe indeed.
Treatment of loosening. Replacement of the loose component with another may be successful, but the operation is more difficult and less reliable than a primary hip replacement. Excision arthroplasty may be needed (Fig. 24.11) as a salvage procedure.
 |
| Fig. 24.11 Porotic rheumatoid bone. The prosthetic components have been removed from the right hip and the bone has fractured around the cement on the left. |
Other complications
Other complications include fracture of the components (Fig. 24.12), dislocation (Fig. 24.13) and excessive new bone formation (Fig. 24.14).
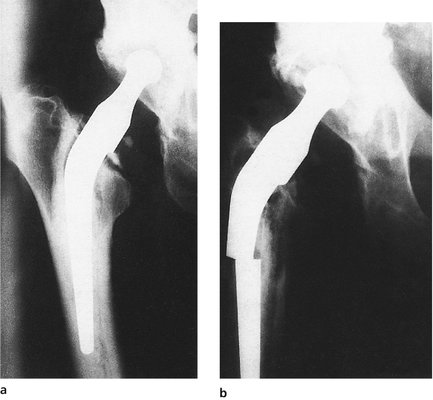 |
| Fig. 24.12 Fracture of a femoral component. (a) Note the ‘windscreen wiper’ gap between the cement and prosthesis; (b) the component has fractured. |
 |
| Fig. 24.13 Dislocation of a prosthesis. The cup was placed too steeply. |
 |
| Fig. 24.14 New bone formation around a total hip prosthesis. |
Investigation of a painful hip prosthesis
A painful hip prosthesis needs investigation by the following means:
• Radiographs.
• Blood tests.
• Isotope scans.
• Aspiration.
Radiographs. A transradiant line is seen around a loose or infected prosthesis, with scalloping of the deep surface of the cortex where it has been eroded by the foreign body reaction or infection.
Blood tests. Infection around hip prostheses is not dramatic and the white cell count is almost always normal. The ESR is usually raised to between 30 and 50 mm/h in both loosening and infection and does not differentiate between the two. The polymerase chain reaction to detect microscopic parts of the bacterial DNA may be the most sensitive.
Isotope scan. Technetium-99m scans show areas of activity in both loosening and infection and a gallium or indium scan may show areas of infection (Fig. 24.15).
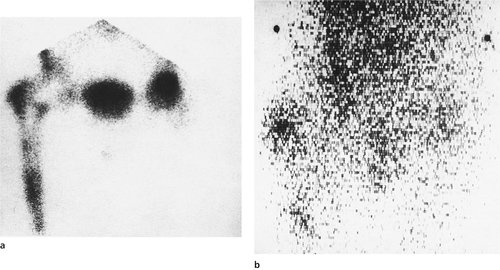 |
| Fig. 24.15 (a) Technetium-99m bone scan showing loosening or infection around the femoral components. (b) Gallium scan showing activity around the tip of the prosthesis and the greater trochanter, suggesting infection. |
Aspiration. Aspiration of the fluid around the prosthesis is helpful if a bacterium is retrieved but a sterile aspirate does not exclude infection. This procedure should be done with full sterile precautions in the operating theatre.
Revision hip replacement
Replacing (revising) a hip replacement is more difficult than the original procedure. Technical problems include dissecting through tissue that has abnormal anatomy. Dense scar tissue may contain the femoral and sciatic nerves.
Removing the prosthesis and the bone cement is difficult. Bone cement is harder than bone and the femur may be split as the cement is removed from the depth of the shaft. There is likely to be such extensive bone loss in both the femur and acetabulum that the standard prostheses do not fit.
Care must be taken to be as certain as possible that the wound is not infected. Tissues can be examined by Gram staining during the procedure but a negative finding does not exclude infection. If it seems likely that infection is present, it is wise to remove all foreign material, irrigate thoroughly, pack the wound with antibiotic-impregnated beads and close it. Antibiotics should be given systemically for at least 8 weeks, by which time any residual infection should be under control. The new prosthesis can then be inserted at a second operation.
For all these reasons, revision surgery of the hip and other joints is a formidable procedure in terms of technique, surgical time and expense.
Other operations for osteoarthritis
Osteotomy
Before total hip replacement was available, femoral osteotomy was commonly done to realign the femur so that the load was taken by a different area of bone (Fig. 24.16). In this respect, the operation was similar in principle to moving an area of worn carpet away from the door. Osteotomy also affects the venous drainage of bone, and perhaps allows microfractures to heal.
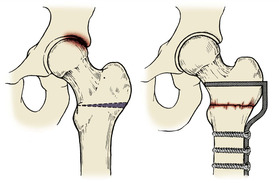 |
| Fig. 24.16 Osteotomy for osteoarthritis of the hip. A wedge is taken from the femur to alter load bearing across the hip. |
Results of osteotomy are satisfactory in about 75% of patients 2 years after operation, but many have pain relief for much longer. The operation is indicated for younger patients who are unsuitable for total hip replacement. Acetabular rotational osteotomies work in the same way.
Excision arthroplasty
Excision arthroplasty was developed by Girdlestone as a primary procedure for osteoarthritis and is still known as Girdlestone’s operation. The hip joint is replaced with a fibrous ankylosis and is similar to Keller’s operation and other excision arthroplasties.
The operation converts a painful but stable joint into one that is unstable but less painful. The limb is shortened but function of the limb is improved. Today, the operation is done as a salvage procedure for failed total hip replacement and not as a primary procedure.
Arthrodesis
Arthrodesis of the hip leaves a solid hip that will last a lifetime and is indicated for gross destruction of the hip in a young patient, e.g. after a motorcycle accident (Fig. 24.17). The alternative operation in such a patient is a total hip replacement, which is doomed to failure in a young and active adult.
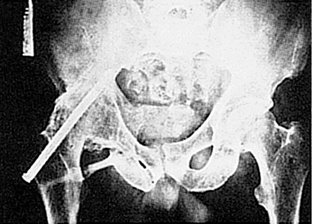 |
| Fig. 24.17 An extra-articular arthrodesis of the hip. |
The operation has the advantage that an arthrodesis can be revised to a total hip replacement but hip replacement can only be revised to another hip replacement or excision arthroplasty.
Arthrodesis also has the disadvantage that the movement lost at the hip is made up for by excessive movement of the lumbar spine and the knee, which then become worn and present problems of their own.
Hemiarthroplasty
Prosthetic replacement of the femoral head alone was once used as a treatment for osteoarthritis of the hip but was unsuccessful because the degenerate acetabulum was eroded by the metal head of the prosthesis. The operation is successful when used as the treatment for fractures of the femoral neck because the acetabulum is healthy in these patients.
Interposition arthroplasty
Cup, or mould, arthroplasty was a standard operation for osteoarthritis of the hip before total hip replacement was introduced, but has now been superseded.
Surface replacement arthroplasty, in which both joint surfaces were replaced but the femoral shaft left intact, was comparable with a mould arthroplasty. The operation was introduced in the 1980s but the results were poor and it became obsolete. New designs of such prostheses are promising (see Fig. 24.5 and Fig. 24.8).
Other hip conditions
Protrusio acetabuli
Protrusio acetabuli is a strange condition for which no cause is known (Fig. 24.18). The medial wall of the acetabulum becomes paper-thin and the head migrates medially. The result is a hip that is virtually ankylosed in the neutral position.
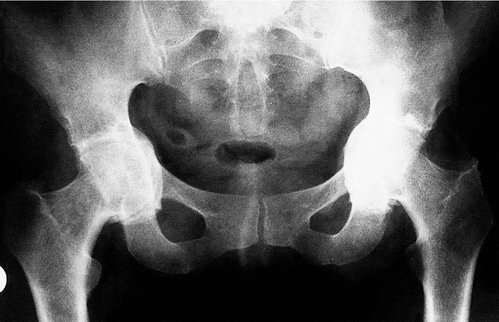 |
| Fig. 24.18 Bilateral protrusio acetabuli. |
Treatment. Untreated, the patient loses both rotation and abduction and in effect has bilateral hip arthrodesis. No treatment is effective except joint replacement.
Ankylosing spondylitis
Ankylosing spondylitis causes stiffness of the spine and large weight-bearing joints, including the hip. The HLAb27 gene is often found in association with this condition.
Treatment. It is tempting to restore joint movement by total hip replacement but the hips may stiffen again with a bony ankylosis around the components. Apart from general conservative management to improve the function of the joint, there is no effective treatment for ankylosing spondylitis of the hip.
Infections
Tuberculosis of the hip was a common cause of hip disease in the past and many older patients still have destroyed or ankylosed hips as a result. Total hip replacement produces a good result. The theoretical risk that the mycobacteria could be lying dormant at the hip and be reactivated at the time of operation does not appear to be justified in practice.
Trochanteric bursitis
The trochanteric bursa lies between the greater trochanter and the insertion of the abductors and, like other bursae, can become inflamed and swollen. Some patients have an acute calcific bursitis comparable with acute calcific supraspinatus tendinitis.
On clinical examination the pain is localized to the greater trochanter and the bursa is tender. Passive hip movements are full but active abduction and abduction against resistance are painful. Radiographs may show a puff of calcification arising from the apex of the greater trochanter.
Treatment. A steroid injection into the bursa usually produces immediate relief of symptoms.
Septic arthritis
Acute septic arthritis is a rare condition today and therefore often escapes diagnosis when it does occur.
Treatment. Left untreated for even 24 h, the articular cartilage of the hip is destroyed and late osteoarthritis becomes almost inevitable. Accordingly, any child with an acute illness and a painful hip should be considered to have septic arthritis until proved otherwise.
The treatment consists of intravenous antibiotics after blood culture specimens have been sent to the laboratory, and immediate exploration of the hip.
Septic arthritis in adults is rare, but gonococcal arthritis is sometimes seen. In debilitated patients, diabetics and those taking steroids, septic arthritis is not uncommon.
Irritable hip (transient synovitis)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








