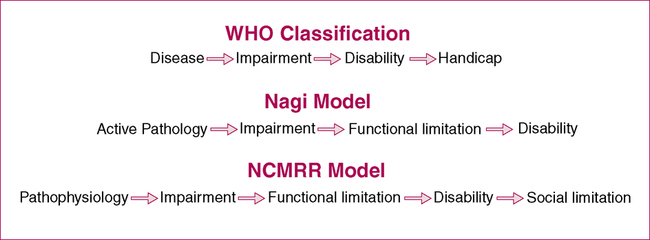
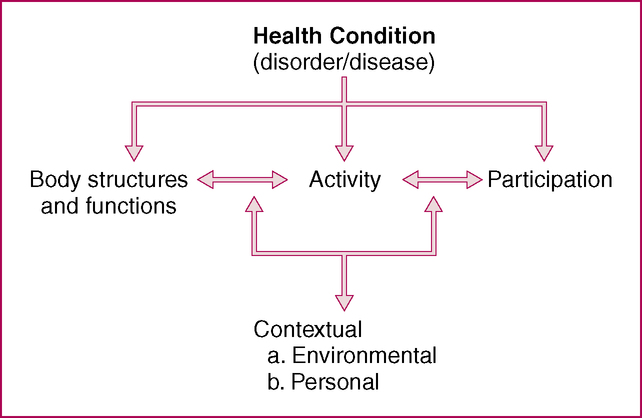
CHAPTER 1 After reading this chapter and completing the exercises, the reader will be able to: 1. Define a functional outcome and discuss its importance in physical therapy documentation. 2. Identify and describe three historical models of disablement. 3. Define the components of the International Classification of Functioning, Disability, and Health (ICF) model. 4. Classify clinical observations and measurements according to the ICF. 1. Examination procedures should determine relevant limitations in functional activities and the impairments that cause those limitations. 2. Goals should be explicitly defined in terms of the functional activities that the patient will be able to perform. 3. Specific interventions should be justified in terms of their effects on functional outcomes. 4. Most importantly, the success of interventions should be measured by the degree to which desired functional outcomes are achieved. The use of disablement models as an organizing framework for physical therapy was one of the key conceptual developments of the 1990s (Jette, 1994). Various models of disablement have been developed and explored, including the original WHO model (1980), the Nagi model (1965), and the National Center for Medical Rehabilitation Research (NCMRR) model (National Advisory Board on Medical Rehabilitation Research, 1991). These models are illustrated in Figure 1-1. Despite differences in terminology, each model provides a framework for analyzing the various effects of acute and chronic conditions on the functioning of specific body systems, basic human performance, and people’s functioning in necessary, expected, and personally desired roles in society (Jette, 1994). Disablement describes the consequences of disease in terms of its effects on body functions, the ability of the individual to perform meaningful tasks, and the ability to fulfill one’s roles in life. The arrows in Figure 1-1 imply a causal chain leading from active pathology to disability using the Nagi model as an example. Indeed, the causal links between elements in the models are useful; they help to conceptualize the relationships between findings at different levels. Nevertheless, the arrows often were interpreted as indicating a temporal series of events, which many health professionals found problematic. Furthermore, it was believed that these models did not capture the complexity of the relationships between different levels that were often multidirectional. In this new model, the process of disablement is a combination of (1) losses or abnormalities of body function and structure, (2) limitations of activities, and (3) restrictions in participation (Figure 1-2). Of note, the terms activity and participation focus on a person’s abilities versus inabilities or disabilities. As shown in Figure 1-2, the ICF model relinquishes the notion of simple, unidirectional causal links between levels. The individual’s pathologic state (health condition) becomes a broader category that influences all other levels. Furthermore, contextual factors—both extrinsic (environmental) and intrinsic (personal)—are specifically identified as affecting the relationship between body structures and functions and activities, and participation. Personal factors can consist of such things as family support, whereas extrinsic factors might include environmental barriers. These important additions highlight the multiple factors that can be related to any one person’s “disability.” The ICF is endorsed by the WHO as the international standard used to measure health and disability (resolution WHA 54.21). In addition to the overall model presented in Figure 1-2, the ICF provides definitions (Box 1-1) and detailed descriptions of what each “level” encompasses (Figure 1-3). Figure 1-3 provides sample descriptions from the ICF framework that could be used for a patient who has had a stroke and has gait impairments, mobility limitations, and faces environmental barriers in the workplace. Within each of the ICF domains there is a hierarchy of description (Chapter, second, third, and fourth levels as needed). This ultimately leads to a code that can be used to refer to a specific domain. These definitions and codes provide common terminology that can be used by all health professionals, whether describing individual patient characteristics (as in Figure 1-3) or conducting large-scale population-based research.
Disablement Models, ICF Framework, and Clinical Decision Making
Historical Perspective of Disablement Models
INTERNATIONAL CLASSIFICATION OF FUNCTIONING, DISABILITY AND HEALTH
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Disablement Models, ICF Framework, and Clinical Decision Making




