Proximal median (PMNE) and radial (RNE) nerve entrapment syndromes are uncommon. This article provides an evidenced-based treatment guideline for PMNE and RNE based on the available literature. Arriving at an accurate diagnosis must involve an electrodiagnostic (EDx) workup. EDx, including nerve conduction velocity studies and needle electromyography, should corroborate the clinical diagnosis and must be done before consideration of any surgical treatment. Conservative care includes rest, modified activities, splinting at wrist and elbow, physical therapy, antiinflammatory drug therapy, and corticosteroid injections. Conservative care should be required for at least 6 weeks before any operative interventions are considered.
Key points
- •
Proximal median and radial nerve entrapment are rare conditions.
- •
A small number of providers make a disproportionate number of these diagnoses, and conduct multiple surgical interventions.
- •
An accurate diagnosis, including specific electrodiagnostic findings, must be determined.
- •
Conservative care includes rest, modified activities, splinting at wrist and elbow, physical therapy, antiinflammatory drug therapy, and corticosteroid injections.
Introduction
Proximal median (PMNE) and radial (RNE) nerve entrapment syndromes are not common. As such, there are no high-quality clinical or scientific studies regarding these conditions. However, these guidelines have been developed using the best available evidence-based studies with an emphasis is on accurate diagnosis and treatment that is curative or rehabilitative. These guidelines were developed originally by the Washington State Labor and Industries’ Industrial Insurance Medical Advisory Committee (IIMAC) and its subcommittee on Upper Extremity Entrapment Neuropathies. It focuses on work-related medical conditions. One of the subcommittee’s goals is to provide standards that ensure a uniformly high quality of care for injured workers in Washington State. The IIMAC unanimously approved these guidelines, which have been updated recently. The subcommittee that has approved of these guidelines is composed of a group of physicians of various medical specialties, including rehabilitation medicine, occupational medicine, orthopedic surgery, plastic surgery, neurosurgery, neurology, pain medicine, and electrodiagnostic medicine. The subcommittee based its recommendations on the weight of the best available clinical and scientific evidence from a systematic review of the literature.
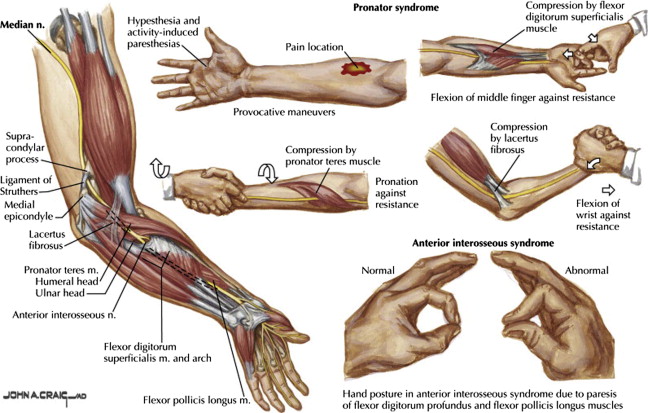
Objective confirmation of the diagnosis of PMNE/RNE is critical to making the correct diagnosis and directing appropriate treatment. Entrapment of the median nerve in the proximal forearm must be distinguished from more distal sites of entrapment, such as at the wrist (carpal tunnel) or at the anterior interosseous nerve branch (which supplies no cutaneous sensation). Proximal compression of the median nerve may occur near the antecubital fossa can occur as the nerve traverses any of the following anatomic structures: the ligament of Struthers/supracondylar process, the lacertus fibrosis (bicipital aponeurosis), the fascia of the pronator teres, or the fibrous arch formed by fascia of the flexor digitorum superficialis. The anatomy of PMNE is illustrated in Fig. 1 .
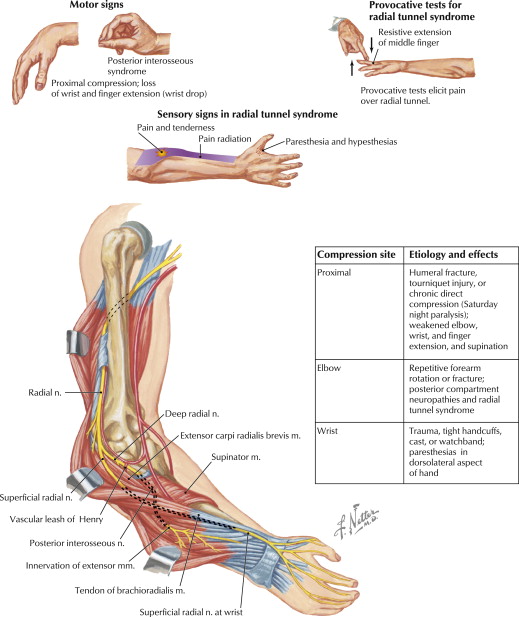
When it occurs in relation to work, RNE usually refers to 1 of 2 syndromes: radial tunnel syndrome or posterior interosseous nerve syndrome (PINS). Although RNE may occur from compression at any point along the course of the radial nerve owing to acute trauma (eg, humerus fracture, Saturday night palsy), space-occupying lesion (eg, lipoma, ganglion), or local edema or inflammation, this guideline focuses on radial tunnel syndrome and PINS, which are more typical for RNE arising from repetitive work activities. Radial tunnel syndrome and PINS have been described to occur at 1 of 5 potential sites. These sites, from proximal to distal, include the fibrous bands of the radiocapitellar joint, radial recurrent vessels (the leash of Henry), the tendinous edge of the extensor carpi radialis brevis, the arcade of Frohse, and the distal edge of the supinator. Most cases of RNE have been described at the arcade of Frohse. The anatomy of RNE is illustrated in Fig. 2 .
In general, both work relatedness and appropriate symptoms and signs must be present to accept PMNE on a claim. Electrodiagnostic (EDx) studies, including nerve conduction velocity studies (NCVs) and needle electromyography (EMG), should be scheduled immediately to corroborate the clinical diagnosis. Completion of EDx studies should always be accomplished before any surgery is considered.
Introduction
Proximal median (PMNE) and radial (RNE) nerve entrapment syndromes are not common. As such, there are no high-quality clinical or scientific studies regarding these conditions. However, these guidelines have been developed using the best available evidence-based studies with an emphasis is on accurate diagnosis and treatment that is curative or rehabilitative. These guidelines were developed originally by the Washington State Labor and Industries’ Industrial Insurance Medical Advisory Committee (IIMAC) and its subcommittee on Upper Extremity Entrapment Neuropathies. It focuses on work-related medical conditions. One of the subcommittee’s goals is to provide standards that ensure a uniformly high quality of care for injured workers in Washington State. The IIMAC unanimously approved these guidelines, which have been updated recently. The subcommittee that has approved of these guidelines is composed of a group of physicians of various medical specialties, including rehabilitation medicine, occupational medicine, orthopedic surgery, plastic surgery, neurosurgery, neurology, pain medicine, and electrodiagnostic medicine. The subcommittee based its recommendations on the weight of the best available clinical and scientific evidence from a systematic review of the literature.
Objective confirmation of the diagnosis of PMNE/RNE is critical to making the correct diagnosis and directing appropriate treatment. Entrapment of the median nerve in the proximal forearm must be distinguished from more distal sites of entrapment, such as at the wrist (carpal tunnel) or at the anterior interosseous nerve branch (which supplies no cutaneous sensation). Proximal compression of the median nerve may occur near the antecubital fossa can occur as the nerve traverses any of the following anatomic structures: the ligament of Struthers/supracondylar process, the lacertus fibrosis (bicipital aponeurosis), the fascia of the pronator teres, or the fibrous arch formed by fascia of the flexor digitorum superficialis. The anatomy of PMNE is illustrated in Fig. 1 .
When it occurs in relation to work, RNE usually refers to 1 of 2 syndromes: radial tunnel syndrome or posterior interosseous nerve syndrome (PINS). Although RNE may occur from compression at any point along the course of the radial nerve owing to acute trauma (eg, humerus fracture, Saturday night palsy), space-occupying lesion (eg, lipoma, ganglion), or local edema or inflammation, this guideline focuses on radial tunnel syndrome and PINS, which are more typical for RNE arising from repetitive work activities. Radial tunnel syndrome and PINS have been described to occur at 1 of 5 potential sites. These sites, from proximal to distal, include the fibrous bands of the radiocapitellar joint, radial recurrent vessels (the leash of Henry), the tendinous edge of the extensor carpi radialis brevis, the arcade of Frohse, and the distal edge of the supinator. Most cases of RNE have been described at the arcade of Frohse. The anatomy of RNE is illustrated in Fig. 2 .
In general, both work relatedness and appropriate symptoms and signs must be present to accept PMNE on a claim. Electrodiagnostic (EDx) studies, including nerve conduction velocity studies (NCVs) and needle electromyography (EMG), should be scheduled immediately to corroborate the clinical diagnosis. Completion of EDx studies should always be accomplished before any surgery is considered.
Case definition
For the purposes of this article, the case definition of confirmed PMNE/RNE included appropriate symptoms, objective physical findings (signs), and abnormal EDx studies. A provisional diagnosis may be made based on appropriate symptoms and objective signs alone, but confirmation of the diagnosis requires abnormal EDx studies. Nonoperative therapy may be considered for cases in which a provisional diagnosis has been made. Operative treatment should be undertaken only in cases where the diagnosis has been confirmed by abnormal EDx studies, because the potential benefits of surgery outweigh the risks.
Clinical findings
Proximal Median Nerve Entrapment
The primary symptom associated with PMNE is pain in the proximal volar area of the forearm. Many patients report an increase in pain severity with an increase in activity. Other symptoms may include weakness in the forearm and the hand (such as a decrease in grip strength), cramping in the hand (writer’s cramp), and paresthesia or numbness in the first 3 digits. Nocturnal symptoms are not as common for PMNE as they are for carpal tunnel syndrome. There is accompanying tenderness to palpation over pronator teres muscle. Inability to produce an “OK” sign may be noted.
Physical signs include tenderness in the forearm over the pronator teres muscle and along the median nerve distribution. Unlike median entrapment at the carpal tunnel, if weakness is present, it should involve muscles supplied by the median nerve both above and below the wrist. The Tinel sign (paresthesias radiating in a median nerve distribution with pressure or tapping over the median nerve in the forearm) may be present, but by itself is not specifically diagnostic of PMNE. A positive Phalen sign (paresthesias radiating in a median nerve distribution with sustained flexion of the wrist) or Tinel sign with tapping over the wrist more likely indicates carpal tunnel syndrome, rather than PMNE.
Three provocative tests have been described to help corroborate the site of compression for PMNE. These provocative tests do not replace the objective signs discussed elsewhere in this article. The sensitivity and specificity of these provocative tests have not been established. The tests are based on creating maximal tension on the anatomic sites that can contribute to PMNE:
- 1.
The pronator teres muscle is implicated if symptoms are reproduced upon resisted pronation of the forearm in neutral position with the elbow extended.
- 2.
The lacertus fibrosis (bicipital aponeurosis) is implicated if symptoms are reproduced upon resisted elbow flexion at 120° to 130° flexion with the forearm in maximal supination.
- 3.
The flexor digitorum superficialis is implicated if symptoms are reproduced upon resisted flexion of the proximal interphalangeal joint to the long finger (“middle finger flexion test”).
Symptoms associated with RNE may include weakness in radial innervated muscles and pain or aching over the proximal, lateral forearm. Patients may report an increase in pain severity with an increase with activity or during sleep. Loss of motor function is most common with PINS.
Signs on examination may include tenderness over the radial nerve distal to the lateral epicondyle. Tenderness on palpation is a useful objective finding, but alone cannot support the diagnosis of RNE. Motor findings include difficulty extending the thumb, fingers, or wrist. Motor testing should compare strength of radial innervated muscles to strength of the same muscles in the nonaffected limb as well as nonradial innervated muscles of the affected limb. Atrophy of affected muscles may be seen in chronic or severe cases.
Provocative tests have been described to help corroborate the diagnosis of RNE. These tests include pressure over the radial tunnel (“radial nerve compression test”), resisted supination with the elbow extended (“resisted supination test”), and resisted extension of the middle finger at the metacarpophalangeal joint (“middle finger test”). These tests are based on creating maximal tension on the anatomic sites that are involved in RNE. However, the sensitivity and specificity of these tests have not been established. Every effort should be made to confirm objectively the diagnosis of RNE before considering surgery. A differential diagnosis for RNE includes extensor tendinitis and lateral epicondylitis (which can coexist with RNE), neuralgic amyotrophy, brachial plexopathy, or cervical radiculopathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






