Derotation of the Scoliotic Spine
Stefan Parent
INTRODUCTION
Adolescent idiopathic scoliosis (AIS) is the most common form of spinal deformities, and its surgical treatment has evolved over the years from a simple spine arthrodesis to a more complex surgical procedure involving the use of instrumentation and better corrective strategies. The challenge in this procedure has shifted from the perioperative morbidity of the procedure to the long-term evaluation of radiographic and quality of life outcomes. The single most important objective remains the prevention of long-term progression of the scoliotic deformity and prevention of long-term sequelae. Additionally, obtaining a well-balanced pain-free spine has been set as a standard criterion for success. Great strides have been made in the last 20 years to better correct the spinal deformity, and great strides have been made to better correct the different aspects of the trunk deformity and not rely solely on the correction of the spinal deformity to achieve improvement in trunk shape. This chapter focuses on the different steps involved in correcting the spinal deformity including the torsional aspects of the deformity. Although different variations of these corrective techniques exist, the technique described herein is commonly referred to as direct vertebral derotation (DVD).
INDICATION/CONTRAINDICATIONS
The main objective of surgical correction of AIS is to improve spinal balance and alignment and to prevent further progression. The indication for surgery is usually based on a curve magnitude greater than 45 to 50 degrees, the clinical deformity, skeletal maturity, and the risk of progression. The Cobb angle cutoff is based on the long-term risk of progression into adulthood for thoracolumbar or lumbar curves greater than or equal to 45 degrees and thoracic curves greater than 50 degrees.
Contraindications are usually reserved for patients not healthy enough to undergo the surgery and patient preference.
PREOPERATIVE PLANNING
An excellent way to better appreciate the 3D spinal deformity is through the use of 3D reconstructions based on two orthogonal views of the spine acquired in the standing position. The system used at our institution to obtain 3D reconstruction is the EOS system, which provides two orthogonal views at a fraction of the radiation dose of other common radiologic systems. The 3D reconstructions obtained have a precision of 1 mm compared to CT scan reconstruction at 1/1,000th of the dose and provide information in the standing position for a given patient. These 3D reconstructions give access to views of the spine that are not easily accessible or even possible using standard radiographs. One can therefore better appreciate the hypokyphosis seen in scoliotic deformities as well as abrupt changes in the sagittal profile of different scoliotic segments of the deformed spine.
SURGICAL PROCEDURE
For a posterior correction and spinal fusion, the patient is placed in the prone position either on a Jackson Table (our preferred method) or on a Relton-Hall frame. Careful positioning is vital to prevent any pressure ulcers, skin problems, or increased pressure on the eyes. Furthermore, a significant portion of the correction can be achieved just by positioning the patient on the operating table. For example, thoracic kyphosis can be improved just by positioning the thoracic pad appropriately, which in turn will help restoring kyphosis later in the surgery. The abdomen contents should be free of pressure reducing the risk of bleeding.
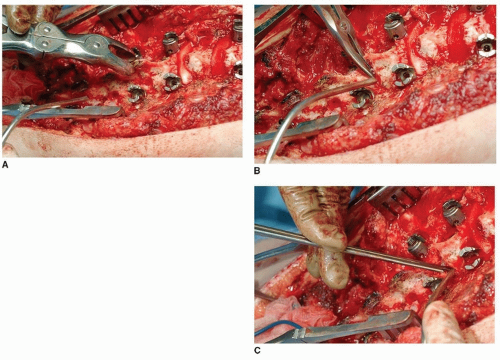
An incision is then performed midline along the spine. Subperiosteal elevation of spinal musculature is then performed and wide exposure of the spine achieved. Thoracic and lumbar pedicle screws are then carefully positioned to insure good vertebral attachment to help perform the spine derotation. Wide posterior release (in the form of Ponte osteotomies) will often provide greater spine flexibility and improve sagittal correction (Fig. 49-1A-C). Vertebral implants’ position is verified using standard radiographs (our preferred method), fluoroscopy, or intraoperative portable CT scan. This insures good visualization of implant placement prior to correction of the spinal deformity. Once the implants have all been securely positioned, correction of the deformity will aim at correcting the sagittal, coronal, and axial deformity (3D correction). The correction can be further divided into a global, regional, and local correction. Each of the steps described hereafter will have a specific goal in correcting some aspect of the deformity. We prefer to use uniplanar screws that allow for some adjustment in the sagittal plane but retain good derotation properties in the axial plane.
Global Correction
There are three main corrective maneuvers to improve the global spinal alignment in AIS. The first method, and probably the most common maneuver, is the rod derotation maneuver introduced by Cotrel and Dubousset. This method is achieved by attaching the rod to the vertebral implants by inserting the rod at about 90 degrees from its final position, loosely securing the rod to the spine,
and then derotating the rod 90 degrees to reach its final position in the coronal plane. This technique of bringing the rod to the spine and then derotating the rod provides good correction in the coronal and sagittal plane in a very synchronized fashion. The rod may be bent with asymmetric amounts of kyphosis with the left rod having more kyphosis than the right to aid in derotation of a typical right thoracic curve. For a right thoracic curve or a double major curve, the left rod would be used as the corrective rod. Other authors have suggested using the right rod as the corrective rod, but we tend to use the right rod first, only if there is significant kyphosis in the thoracic spine.
and then derotating the rod 90 degrees to reach its final position in the coronal plane. This technique of bringing the rod to the spine and then derotating the rod provides good correction in the coronal and sagittal plane in a very synchronized fashion. The rod may be bent with asymmetric amounts of kyphosis with the left rod having more kyphosis than the right to aid in derotation of a typical right thoracic curve. For a right thoracic curve or a double major curve, the left rod would be used as the corrective rod. Other authors have suggested using the right rod as the corrective rod, but we tend to use the right rod first, only if there is significant kyphosis in the thoracic spine.
Spine translation is another method commonly used to correct the global deformity. In this case, the rod is rigidly fixed in its final position, and the spine is progressively translated to the rod. This technique was initially described by Luque and used sublaminar wires. Nowadays, reduction screws or pedicle screws with reduction tools can be used to correct the spine progressively. This method often requires several rounds of progressively reducing the spine but has the advantage of a progressive reduction. The other challenge is that the method usually needs a form of multiaxial pedicle screw to permit screw and rod attachment.
The third method is rod cantilever. This technique is most commonly used in thoracolumbar or lumbar curves. The rod is usually attached to one end of the construct and progressively levered in the other adjacent levels. This can also be accompanied by rod derotation once the rod is fully seated inside the screws.
Regional Correction
The sagittal profile of the thoracic spine is predominantly in hypokyphosis or relative lordosis. This has led several surgeons to address the sagittal plane deformity with interventions aimed at restoring a more normal sagittal profile. These range from performing anterior releases to shorten the anterior column, posterior wide release to allow spine elongation, and differential rod bending to increase the thoracic kyphosis while correcting the thoracic rotational deformity. Differential rod bend can help restore kyphosis regionally. We typically overbend the concave rod (left rod for a typical right thoracic curve) and use a slightly underbent rod on the convexity (Fig. 49-2).
DVD is the general term for derotating the spine when using pedicle screws, which capture all three columns of the spine. DVD can be used with en bloc or segmental derotation techniques. With en bloc techniques, the apical two to three vertebrae are linked and rotated as a unit. With the segmental techniques, each vertebra is individually rotated against the adjacent vertebrae.
Segmental derotation is our method of choice to correct the mechanical torsion of the spine. This technique aims at correcting the intervertebral rotation at each level by stabilizing the adjacent segment and derotating the selected vertebral level. The amount of derotation necessary is less at each level when compared to the important derotation applied in the en bloc technique, but when each level is added, the total amount of derotation is similar. The technique can be done with only one screw per level but is typically done with two screws per level to divide the loads applied at the bone/screw interface. Again, several authors have proposed several ways of linking vertebral attachments (usually pedicle screws) at a single level to insure synchronized derotation of the vertebral segment. We typically use some form of screw extension attached to the pedicle screw that allows axial correction of the deformity without necessarily attaching the two screws at one level together.
For a typical right thoracic curve, a left overbent rod would first be attached to the pedicle screws on the left and then derotated 90 degrees (Fig. 49-3A, B). The segmental derotation technique would then be started distally at the last instrumented vertebra and by attaching screw extension or posts to the uniplanar pedicle screws. This would be typically done with the concave rod in place and the convex rod attached to the distal screw but left proud proximally. The sagittal position of the rods
is fixed at that time (Fig. 49-4A, B). We sometimes add 10 degrees of initial rod rotation on the concave side to hypercorrect the scoliotic segment. The derotation posts are then attached to the adjacent instrumented vertebral level. Once the posts securely attached, the distal segment is maintained rigidly in place and locked in place on the rod by the assistant or the surgeon. The surgeon can then derotate the adjacent segment, and the screws can then be secured to the rod by the assistant (Fig. 49-5A, B). This can then be repeated segmentally at each level to correct the mechanical torsion or intervertebral rotation at every level (Fig. 49-6A, B



is fixed at that time (Fig. 49-4A, B). We sometimes add 10 degrees of initial rod rotation on the concave side to hypercorrect the scoliotic segment. The derotation posts are then attached to the adjacent instrumented vertebral level. Once the posts securely attached, the distal segment is maintained rigidly in place and locked in place on the rod by the assistant or the surgeon. The surgeon can then derotate the adjacent segment, and the screws can then be secured to the rod by the assistant (Fig. 49-5A, B). This can then be repeated segmentally at each level to correct the mechanical torsion or intervertebral rotation at every level (Fig. 49-6A, B
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree