Spondylolisthesis: Decompression, Partial Reduction, and Fusion
Harry L. Shufflebarger
Jahangir Asghar
INDICATIONS/CONTRAINDICATIONS
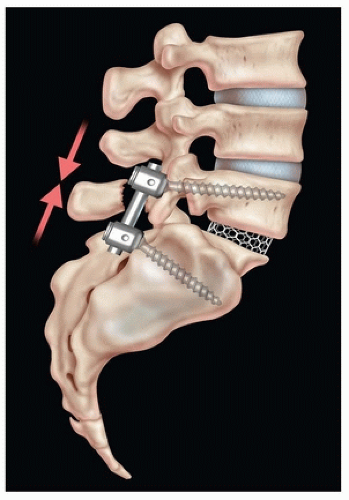
The procedure to be described is an instrumented spinal fusion with a structural interbody cage at the level of spondylolisthesis placed by the transforaminal lumbar interbody fusion method. Some degree of reduction of the spondylolisthesis is a usual accompaniment. This is the authors’ standard treatment for any degree of spondylolisthesis.
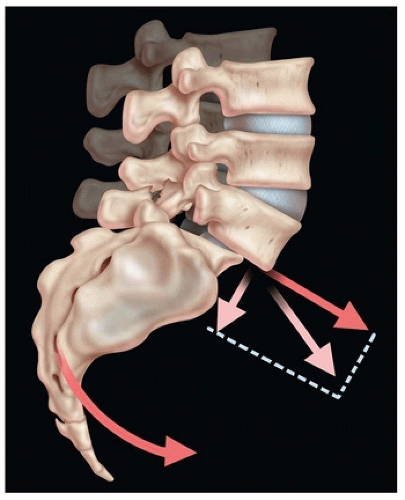
Indications for the procedure include failure of conservative treatment for spondylolisthesis, presence of any neurologic deficit, and any slip in excess of 50%. However, reduction of high dysplastic spondylolisthesis remains controversial, with a deserved bad reputation. Schoenecker et al. (1) describe the procedure as “extremely demanding and potentially dangerous.” Multiple other authors report catastrophic neurologic injury, nerve root deficits, nonunions, progressive slippage, and the need for revision surgery (2, 3, 4).
Fusion in situ is not without complications and problems. The deformity remains with in situ fusion, as well as the sagittal spinopelvic malalignment. This can only result in adjacent segment deformity and early degeneration. In addition, a 6% incidence of cauda equina syndrome has been reported with only fusion in situ. Additional problems with in situ fusion include progression of the deformity, pseudarthrosis, and failure to relieve symptoms (1, 2, 5).
Spondylolisthesis reduction and fusion, correcting the sagittal spinopelvic imbalance, are desirable for multiple reasons. The deformity is corrected. Arthrodesis should and usually does occur in excess of 95% of cases. Monosegmental fixation and fusion may be accomplished. With restoration of sagittal spinopelvic alignment and monosegmental fusion, adjacent segment deformity and degeneration should be minimal. Reduction can be accomplished with neurologic safety, particularly regarding the L5 root. It is the authors’ opinion that the described procedure, instrumented posterior spinal fusion with interbody structural cage with partial or complete reduction, is indicated in all patients with symptomatic spondylolisthesis.
With the exception of an infectious process, there are no contraindications to performing decompression, partial reduction, and fusion for spondylolisthesis.
PREOPERATIVE PLANNING
Complete history and physical examination, with particular attention to neurologic evaluation of the lower extremities, is necessary. Signs of cauda equina irritation, such as tight hamstrings, should be noted. Bowel and bladder competency should be noted.
Imaging studies for planning include erect anterior-posterior and lateral 36-inch radiographs including the occiput, femoral heads, and sacrum. These permit classification of the deformity and determination of the pelvic incidence, sacral slope, and pelvic tilt. These indices are helpful in determining the amount of lumbar lordosis to place in the distal lumbar spine.
A computed tomography (CT) scan is very useful in planning the procedure. This will define the type of defect (isthmic or elongated intact pars) and alert the surgeon to dysplastic changes at L5 or the sacrum (particularly spina bifida occulta). The orientation of the L5 pedicle is defined. The screw length for the sacrum and lumbar spine can be determined.
The anatomy of the sacrum, particularly the dome, is well defined. This is helpful in planning for sacral dome excision.
An MRI scan of the lumbar spine is also necessary. The L5-S1 disc is usually degenerated and deformed. Attention should be directed to the L4–L5 disc. Degenerative changes here may indicate the need to include lumbar 4 in the fusion.
SURGICAL PROCEDURE
This surgical technique of reduction and internal fixation of high dysplastic spondylolisthesis was developed by Professor Juergen Harms and has been reported by this author and by Professor Harms (6, 7). Multiple steps are necessary to successfully perform the procedure.
Monitoring of the L5 nerve root is recommended and easily performed throughout the procedure. Many surgeons have routinely employed the pedicle screw stimulation technique reported by Calancie et al. (8) The same technique can be applied to the L5 root during the various stages of spondylolisthesis reduction. The root should be first stimulated with its identification medial to the L5 pedicle (Fig. 51-1). The normal nerve root stimulation threshold is usually less than 2 mA. In this condition, the stimulation threshold is typically elevated, frequently in excess of 10 mA. With further exposure and decompression of the root, the stimulation threshold usually decreases. Repeated root stimulation throughout the procedure provides the surgeon with real-time evidence of conduction of the root and hence function. Assurance of postsurgical function is present with peripheral response to intraoperative stimulation. Should there be increase in stimulation threshold during the procedure, which means the nerve function is decreasing, the surgeon should alter the procedure and seek the cause of change.
The procedure is performed using the Jackson surgical table (OSI, Union City, CA). A lower lumbosacral skin incision is made, and exposure of L4 to the caudal sacrum is accomplished. This is carried to the tips of the transverse processes of L4 and L5 as well as the alae of the sacrum.
Review of the CT for spina bifida occulta can help avoid inadvertent damage to dura and nerve roots. Care should be exercised during exposure, as the sacrum is frequently dysplastic, and incidental durotomy may be avoided. With exposure complete, the loose posterior element of L5 is excised, in either one piece or piecemeal.
Review of the CT for spina bifida occulta can help avoid inadvertent damage to dura and nerve roots. Care should be exercised during exposure, as the sacrum is frequently dysplastic, and incidental durotomy may be avoided. With exposure complete, the loose posterior element of L5 is excised, in either one piece or piecemeal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree