Chapter 10 Condylar Fractures in Children
Introduction
The age of occurrence depends on the anatomical location. The average age for lateral condylar injuries is around 6 years.1,2 The less common medial condylar injuries occur in the age range 8–12 years.2,3 T-condylar fractures are more common in adolescents but occur in children in the age range 5–12 years (average 8.8 years).4 Fractures involving the entire distal humeral physis may be misdiagnosed as lateral condylar fractures. They should be suspected in a child below 1 year of age but can occur from birth to 6 years.5–7 They have an association with child abuse.
Epicondylar fractures are often associated with dislocations of the elbow and have a peak incidence in the 6- to 12-years age group.8–11
Lateral condylar fractures
Background/aetiology
Fractures of the lateral condyle in children represent 15% of all paediatric elbow fractures and are the second most common childhood elbow injury after supracondylar fractures (70%).12
These fractures constitute 75% of distal humeral physeal fractures.12 It is noted that fractures that exit in the trochlear notch will lead to an element of elbow instability with subluxation of the radius and ulna with the lateral condylar fragment.
Dislocation in association with a lateral condylar fracture has been reported by Rasool.13 He described 14 cases with a posteromedial dislocation and lateral condylar fracture, five of which also had a fracture of the medial epicondyle. He stressed the importance of looking for a lateral condylar fracture in children with a dislocation of the elbow.
Classification
Anatomical location
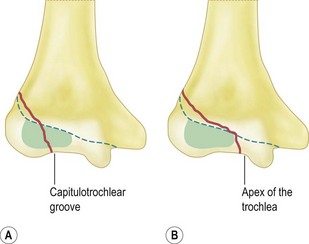
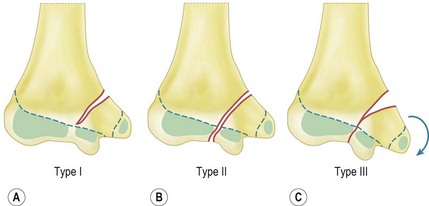
Milch15 described type I and II lateral condylar fractures (Fig. 10.1). In both types, the fracture line begins at the posterolateral aspect of the lateral condyle in the metaphysis:
Staging
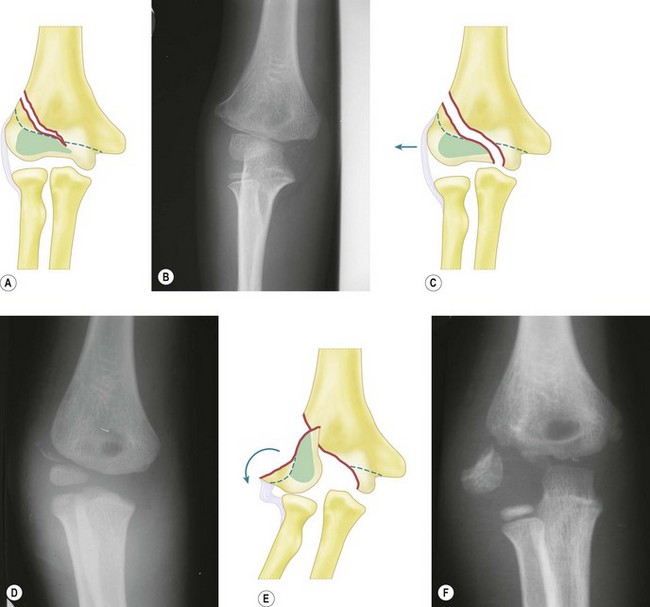
Jakob et al16 described three stages of displacement (Fig. 10.2):
Badelon et al17 modified this classification into four stages. In stage I the fracture line is seen on only one X-ray view and displaced less than 2 mm. In stage II the fracture line is seen on both the anteroposterior (AP) and lateral views but remains displaced less than 2 mm. Stages III and IV are the equivalent of Jakob stage II and stage III, respectively. The addition of the extra stage was to distinguish which fractures were unstable and more likely to displace and thus identify which should be fixed. They determined that stage I could be treated conservatively by plaster immobilization but stages II, III and IV required open reduction and internal fixation.
We use the thee-stage classification of Jakob et al in this text.
Mechanism of injury
Two mechanisms of injury are proposed:
Presentation, investigation and treatment options
Clinical features
In stage I displacement there may be no or minimal swelling and only local tenderness over the lateral condyle, this sign being key to the diagnosis. This can be confirmed by eliciting pain when passively flexing the wrist. In an undisplaced fracture not appreciated on X-ray, the presence of lateral ecchymosis may be the only clinical sign and should alert the clinician to the possible presence of this fracture.19 In addition, swelling is localized to the lateral side of the elbow only.
Investigations
Radiographs
The metaphyseal fragment is often small and minimally displaced, with displacement best appreciated on the lateral view. Badelon et al17 found that if the fracture could only be appreciated on one view then it was stable, but if seen on both views there was more likelihood that the articular hinge was disrupted, making the fracture unstable. The relationship of the proximal ulna and radius to the humerus must be studied since lateral subluxation of the distal radius and ulna imply a Milch II fracture with disruption of the articular hinge.
Finnbogason et al20 reviewed 112 undisplaced and minimally displaced fractures and classified them as stable fractures, fractures with an undefinable risk and high-risk fractures. Stable fractures had no gap or a minimal gap that did not extend all the way to the epiphyseal cartilage (65 cases, none of which had lateral displacement). Fractures with an undefinable risk showed the fracture line extending all the way to the epiphyseal cartilage (displacement occurred in 6 (17%) of 35 fractures). High-risk fractures had a fracture gap that was almost as equally separated laterally and medially. Five (42%) of 12 of these fractures displaced.
Oblique radiographs may improve the diagnosis and Song et al21 found that the internal oblique view was significantly more accurate in demonstrating the fracture gap and fracture pattern than the AP and lateral views. They concluded that classifications should be based on the greatest displacement seen on at least three views, namely AP, lateral and internal oblique.
Arthrogram (Fig. 10.3)
Arthrograms have been shown to increase the accuracy of diagnosis. Yates and Sullivan22 showed that the initial diagnosis on plain radiographs was altered in 7 of 36 (19%) children with elbow injuries.
CT scan
Chapman et al23 showed that multi-detector computed tomography, which can be done in children without using sedation, was highly reproducible in characterizing lateral condylar fractures and frequently demonstrated disruption of the articular surface. It may lead to a change in treatment for children with fracture displacement near the threshold of 2 mm.
MRI
Kamegaya et al24 performed MRI on 12 patients with fractures of less than 2 mm displacement as seen on plain radiographs. Fractures that passed through the articular surface into the joint were deemed unstable. One of five fractures that had 1 mm displacement was found to be unstable and four of seven with 2 mm displacement were found to be unstable. This study suggests that MRI is a useful and accurate method of assessing fracture stability and enables the identification of fractures that would be better treated by pin fixation rather than cast immobilization.
Ultrasound
Ultrasound has been reported to be useful in determining the type of fracture and monitoring for late displacement.25
Treatment
Plaster immobilization
Immobilization is appropriate for 30–40% of lateral condylar fractures.17,26 Badelon et al17 stated that in cases where the fracture is seen in only one view and displaced less than 2 mm (i.e. stable fracture) immobilization is adequate. Speed and Macey27 showed uniformly good results using this method and had no abnormalities of growth or premature fusion. Some authors have recommended placing the forearm in supination to decrease the muscle pull of the extensors and reduce the risk of displacement on the distal fragment.
Late displacement is the concern with simple immobilization. Beaty and Kassar28 had two cases of late displacement out of 24 stage I fractures. Their criteria for plaster immobilization was displacement of less than 2 mm on three X-ray views (AP, lateral and internal oblique).
Closed reduction and pinning for stage II
Mintzer et al29 reported good results after percutaneous pin fixation in 12 fractures with displacement of less than 2 mm. Joint congruity was checked with an arthrogram.
Open reduction and internal fixation
This is the most widely recommended treatment for stage II and stage III fractures because of the propensity for late displacement and the potential for late complications. The key is to have accurate reduction; Hardacre et al1 showed poor results when the reduction was inadequate.
With open reduction, care must be taken to avoid dissection at the posterior aspect of the fragment as this is the site of the fragment’s blood supply. The reduction must be adequate and this is done by direct visualization. Mohan et al30 reported the use of a posterolateral approach that is more cosmetic and provides excellent exposure with minimal dissection. They had no complications in 20 patients.
Methods of fixation
Most authors recommend smooth pins as these do not affect the growth plate. At least two K-wires should be used and can be inserted parallel or crossed. If there is an adequate metaphyseal fragment then one wire can be passed through this fragment. Pins can be buried under the skin or left protruding. There is controversy as to how long the pins need to be left in situ and, although some authors recommend 6 weeks, it has been shown that 3 weeks is sufficient.31
Although smooth pins are preferred Sharma et al32 used partially threaded cancellous screws.
Outcome
Badelon et al17 and Speed and Macey27 reported excellent results in patients with undisplaced fractures.
Bast et al33 reported union rates of 98% following non-operative treatment for undisplaced or minimally displaced fractures.
Ippolito et al34 evaluated 49 individuals at a follow-up of 18–45 years. Twenty fractures with displacement of 2–10 mm without tilting had been treated non-operatively and 36 with displacement and tilting had been treated surgically. All patients had a good result.
Treatment
Stage I fractures
These are treated in an above-elbow backslab with the forearm in pronation and the elbow flexed to 90°. The pronation creates a compressive force on the lateral condyle.35 A check X-ray is performed in the backslab at 1 week and the backslab left on for a total of 3 weeks. Active mobilization is then undertaken without physiotherapy.
Stage II and III fractures
Stage II and III fractures require open reduction and internal fixation. The proximal limb of the Kocher J incision is used and the fracture exposed by opening the fascia between brachioradialis and ECRL. The reduction may be difficult to hold but is assisted with the use of small fragment reduction forceps. It is checked by direct visualization of the anterior aspect of the joint. This is exposed by cutting the synovial attachment to the distal fragment. K-wires (1.6 mm) crossing at the lateral edge of the metaphysis are angulated from each other by approximately 60° (Fig. 10.4). The wires are left protruding through the skin and the end is bent to a right angle. A backslab is applied for 3 weeks with the elbow flexed at 90° and the forearm in neutral rotation. The plaster and wires are removed in the outpatient clinic without anaesthesia.
Complications
Lateral spur formation/lateral condylar overgrowth with cubitus varus
This is seen in 40–50% of patients with loss of carrying angle.27,36,37 De Jager and Hoffman26 reviewed 60 patients following lateral condylar fractures and found an average of 4 mm of lateral condylar overgrowth and an average of 3° loss of the carrying angle. It occurs in those treated operatively or non-operatively and can lead to clinical cubitus varus depending on the pre-morbid carrying angle. It is rarely of cosmetic or functional significance. It is important, however, to warn parents that this deformity may occur.
Delayed union
Delayed union (failure of union within 12 weeks) may occur even when the fracture has been adequately reduced. Reasons include poor vascular supply to the fragment38 or synovial fluid passing between the fracture fragments.1 The fragments remain reduced and eventually unite.
Non-union
Non-union is defined as no union by 12 weeks.38 It occurs with stage II or III fractures that are untreated, present late or are inadequately reduced.
The management of non-unions is controversial. Jakob et al16 and Dhillon et al39 reported that patients who were treated after 3 weeks had the same results as patients who had no treatment at all. Complications included loss of motion, delayed union and non-union, deformity and avascular necrosis.
Other authors have reported success with operative treatment prior to closure of the growth plate.1,38,40 Shimada et al41 reported good results at an average of 11 years follow-up. The average time between injury and surgery was 5 years (5 months to 10 years). One poor result was due to avascular necrosis.
The main concern with late surgery is the risk of avascular necrosis. Speed and Macey27 reported a high incidence of ‘epiphyseal changes’ in patients treated with late surgery. Yang et al,42 however, reported low rates of avascular necrosis and good results by approaching the non-union through an olecranon osteotomy, thus not disrupting the soft tissue attachment to the fragment.
Some patients who are seen years after their fracture (Fig. 10.5) may never have sought treatment at the time of the injury. They present with cubitus valgus. In addition, tardy ulnar nerve palsy may be noted, although this does not normally occur until an average of 22 years after the injury.43 When present, motor loss is usually followed by sensory changes. Papandrea and Waters44 recommended that late presentations were treated by a two-stage procedure. The first stage involved fixation and bone grafting of the non-union with anterior transposition of the ulnar nerve. At a later stage an osteotomy was advised. Milch15 described a transverse osteotomy and, more recently, Tien et al45 has advocated a dome osteotomy with fixation of the non-union through a posterior approach. This is thought to be associated with a reduced rate of complication.
Avascular necrosis
This can involve either the entire lateral condyle or result in a fishtail deformity.
Entire lateral condyle
This is usually iatrogenic and results from disturbance of the extra-osseous blood supply to the fragment. The blood enters via vessels that pierce the condyle in the posterior non-articular area.46 It may occur at the time of surgery for an acute fracture where there has been overzealous stripping of the soft tissue, but is more common in late surgery or surgery for non-unions. Some authors have advocated a transolecranon approach to avoid damaging the blood supply when treating non-unions.42
Fishtail deformity
The so-called fishtail deformity occurs with damage to the intra-osseous end arteries that supply the lateral part of the medial crista of the trochlea. It may also occur in undisplaced supracondylar fractures, medial condylar fractures, fractures of the entire distal humeral physis46 and from persistence of a gap between the lateral and medial ossification centres.47–49
Personal view
Non-union
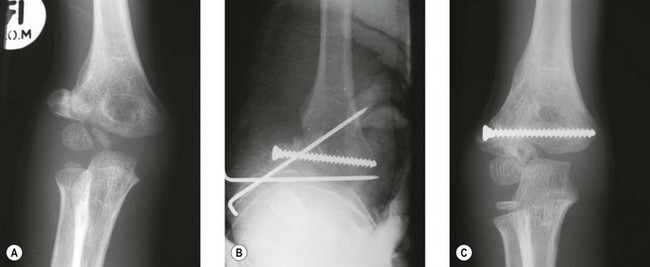
In stage II, the fragment has moved upwards and is tilted laterally and forward. The fragment is mobilized, reduced and held with an oblique K-wire passing through the epiphysis (left out the skin) and with a horizontal 3.5 mm cancellous screw (preferably partially threaded) through the metaphyseal fragment to provide compression (Fig. 10.6). The K-wire is removed at 3 weeks and the elbow mobilized actively. Physiotherapy is not usually necessary.
In stage III, the fragment is rotated. It is mobilized and reduced into a position that allows a functional reduction, i.e. the reduction that yields the best range of movement intraoperatively.40 In addition, in stage III, bone graft may be required. The postoperative management is the same as for stage II.
Medial condylar fractures
Introduction
These fractures are rare and account for less than 1% of fractures of the distal humerus.12 However, as they are intra-articular fractures they require accurate reduction to avoid later complications.
Background/aetiology
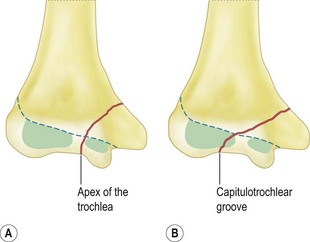
Infants may sustain this injury but more commonly they occur in the age range of 8–14 years.50 The fracture line extends from the metaphysis of the medial condyle and exits between the ossification centres of the lateral and medial condyle (apex of the trochlea) or through the lateral condylar epiphysis (capitulotrochlear groove). The fragment includes the medial epicondyle and the attached flexor muscles. These muscles cause the fragment to rotate so that the articular surface of the fragment faces posteriorly and laterally.
In younger children there is an association with child abuse,51,52 but the fracture also occurs with greenstick fractures of the olecranon and true posterolateral dislocations of the elbow.51,53
Classification
Salter–Harris14
This fracture is most likely a Salter–Harris II injury since untreated fractures result in non-union with cubitus varus rather than physeal arrest, which is more likely to occur with a Salter–Harris IV injury.54 However, the paucity of reported cases has meant that this has yet to be conclusively determined.
Anatomical location
Displacement of the fracture
This has been divided into three types by Kilfoyle55 (Fig. 10.8):
Mechanism of Injury
Two mechanisms of injury have been described. With a fall on the point of the flexed elbow, the semilunar notch of the olecranon impacts against the trochlear notch and initiates the fracture.52,56–58 The second mechanism involves a fall onto the outstretched arm, resulting in an avulsion injury secondary to valgus strain.3,59
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree