Closed Reduction, Casting, and Traction
PRINCIPLES OF CLOSED REDUCTION
Displaced fractures, including those that will undergo internal fixation, should be reduced to minimize soft tissue trauma and provide patient comfort.
Splints should respect the soft tissues.
Pad all bony prominences.
Allow for postinjury swelling.
Adequate analgesia and muscle relaxation are critical for success.
Fractures are reduced using axial traction and reversal of the mechanism of injury.
One should attempt to correct or restore length, rotation, and angulation.
Reduction maneuvers are often specific for a particular location.
One should try to immobilize the joint above and below the injury.
Three-point contact and stabilization are necessary to maintain most closed reductions.
COMMON SPLINTING TECHNIQUES
Splints may be prefabricated or custom made.
“Bulky” Jones (refers to padding)
Lower extremity splint, commonly applied for foot and ankle fractures and fractures about the knee, which uses fluffy cotton or abundant cast padding to help with postinjury swelling. The splint is applied using a posterior slab and a U-shaped slab applied from medial to lateral around the malleoli for ankle/tibia or a knee immobilizer for knee injuries. The extremity should be padded well proximal and distal to the injury.
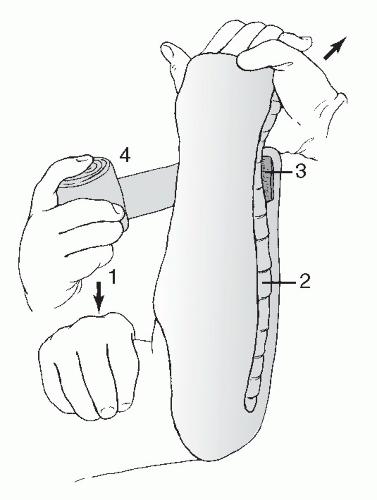
Sugar-tong splint
Upper extremity splint for distal forearm fractures that uses a U-shaped slab applied to the volar and dorsal aspects of the forearm, encircling the elbow (Fig. 1.1).
Coaptation splint
Upper extremity splint for humerus fractures that uses a U-shaped slab applied to the medial and lateral aspects of the arm, encircling the elbow and overlapping the shoulder.
Ulnar gutter splint
Volar/dorsal hand splint
Thumb spica splint
Posterior slab (ankle) with or without a U-shaped splint
Posterior slab (thigh)
Knee immobilizer
Cervical collar
Pelvic sheet/binder
Visit the University of Ottawa web site for general casting techniques and specifics on placing specific splints and casts: www.med.uottawa.ca/procedures/cast/
CASTING
The goal is semirigid immobilization with avoidance of pressure or skin complications.
Used with caution in the treatment of acute fractures owing to swelling and soft tissue complications.
Padding: This is placed from distal to proximal with a 50% overlap, a minimum of two layers, and extra padding for bony prominences (fibular head, malleoli, patella, condyles, and olecranon).
Plaster: Cold water will maximize the molding time. Hot water may lead to thermal injury of the skin. Room temperature water is preferred.
6-inch width for thigh
4- to 6-inch width for leg
4- to 6-inch width for arm
2- to 4-inch width for forearm
Fiberglass
This is more difficult to mold but more resistant to moisture and breakdown.
Generally, it is two to three times stronger for any given thickness.
Visit the University of Ottawa web site for general casting techniques and specifics on placing specific splints and casts: www.med.uottawa.ca/procedures/cast/
Below Knee Cast (Short Leg Cast)
This should support the metatarsal heads.
The ankle should be placed in neutral; apply with the knee in flexion.
Ensure freedom of the toes.
Build up the plantar surface for walking casts.
Fiberglass is preferred for durability.
Pad the fibula head and the plantar aspect of the foot.
Above Knee Cast (Long Leg Cast)
Apply below the knee first.
Maintain knee flexion at 5 to 20 degrees.
Mold the supracondylar femur for improved rotational stability.
Apply extra padding anterior to the patella.
Short and Long Arm Casts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree