Closed, Percutaneous, Intramedullary, and Open Reduction of Radial Head and Neck Fractures
Roger Cornwall
DEFINITION
Radial neck fractures are extra-articular fractures of the radius proximal to the bicipital tuberosity.
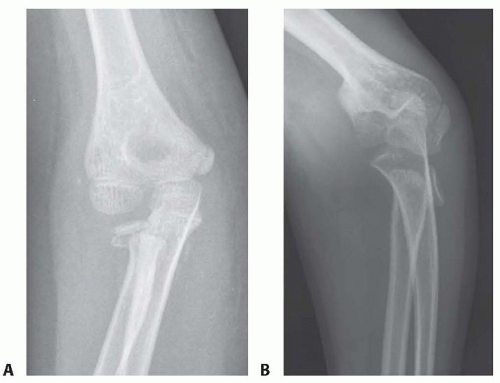
Radial neck fractures are most common in children 9 to 12 years old and represent 14% of elbow fractures in children.17 The physis is typically involved as a Salter-Harris I or II pattern (FIG 1), yet Salter-Harris III and IV patterns also occur. Alternatively, the fracture can be extraphyseal through the metaphysis.1,33
Intra-articular radial head fractures are less common elbow injuries in patients with open physes than in skeletally mature patients (7% vs. 52%).18
The Wilkins classification of radial head and neck fractures is based on the mechanism of injury and the pattern of the fracture, specifically whether there is physeal or articular involvement34:
Type I: valgus injury
A: physeal injury—Salter-Harris I or II
B: intra-articular—Salter-Harris III or IV
C: metaphyseal fracture
Type II: elbow dislocation
D: fracture occurred during reduction
E: fracture occurred during dislocation
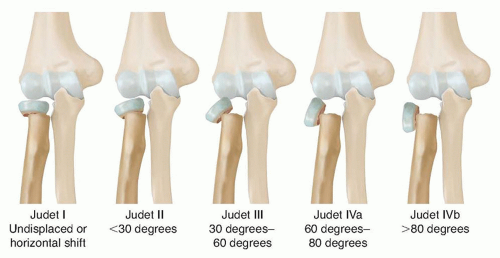
The O’Brien and Judet classifications of radial neck fractures are based on degree of angulation.
O’Brien classification22
Type I: less than 30 degrees
Type II: 30 to 60 degrees
Type III: more than 60 degrees
Type I: undisplaced
Type II: less than 30 degrees
Type III: 30 to 60 degrees
Type IVa: 60 to 80 degrees
Type IVb: more than 80 degrees
ANATOMY
The radial head articulates with the capitellum and the radial notch of the ulna. The radial neck is extra-articular and has a normal 15 degrees of angulation on anteroposterior (AP) and 5 degrees on lateral radiographic views. The radial head ossific nucleus appears at about 4 years of age.
Ossification of the proximal radial epiphysis (radial head) occurs by 4 years of age, at which time the radial head and neck have assumed their adult shape. The proximal radial physis closes at 14 years in girls and 17 years in boys.
The proximal radioulnar joint is stabilized by the annular ligament and the accessory collateral ligament.
There are no muscular attachments to the radial neck. The blood supply is derived from the adjacent periosteum.
The radial nerve gives rise to the superficial radial nerve and the posterior interosseous nerve at the level of the lateral condyle. The posterior interosseous nerve travels distally anterior to the radial head and neck, enters the arcade of Frohse 2.6 cm distal to the radial head (FIG 3), and submerges between the superficial and deep fibers of the supinator 6.7 cm distal to the radial head.5 The radial recurrent artery originates from the radial artery and travels toward the lateral epicondyle in the opposite direction along the path of the radial nerve on the anteromedial surface of the supinator.
PATHOGENESIS
The most common mechanism of radial neck fractures is a valgus and axial force to the elbow caused by a fall on an outstretched hand. This mechanism results in a lateral compression and a medial traction injury. The actual plane of maximal radial head angulation depends on the forearm position of supination or pronation at the time of impact.12
The other mechanism of injury is an elbow dislocation where the fracture occurs either during the dislocation (radial head anterior) or during the elbow reduction (radial head posterior).12
Associated injuries, such as medial collateral ligament rupture or occult elbow dislocation, occur in 30% to 50% of radial neck fractures.28
A posteriorly displaced radial neck fracture can occur during the spontaneous reduction of a posterior elbow dislocation.11
Alternatively, an unrecognized (undisplaced) radial neck fracture can be displaced posteriorly during the manipulative reduction of a posterior elbow dislocation. During the reduction maneuver, if the elbow is flexed, the distal humerus (lateral condyle) strikes the radial head, knocking it posteriorly off the metaphysis (FIG 4).
Chronic stress fractures of the radial head and neck can occur with repetitive valgus loading, such as overhead throwing.
NATURAL HISTORY
The prognosis for radial neck fractures depends on the energy of injury, the amount of displacement, and the presence of any associated injuries.
Most radial neck fractures are minimally displaced or undisplaced. These heal uneventfully.
The greater the degree of angulation or translation, the greater the disruption in the relationship of the radiocapitellar joint, which may be associated with a decrease in the range of pronation and supination.3
The upper limit of acceptable angulation (0 to 60 degrees) is unclear and may be age-dependent.24 Most believe that angulation less than 30 degrees is unlikely to cause a clinically (functionally) significant loss of motion.
Other reported consequences include avascular necrosis of the radial head, heterotopic ossification, radioulnar synostosis, and premature physeal closure, which may result in pain, crepitus, and valgus deformity and stiffness.3,13,24,26,27
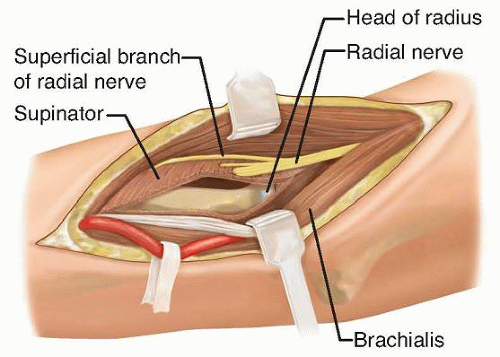
FIG 3 • The posterior interosseous nerve courses volarly to the radial head and neck and enters the arcade of Frohse about 2.6 cm distal to the articular surface of the radial head.
These outcomes may be associated with age, severity of displacement, presence of associated injuries, or delay in treatment.
Some of these might be a complication of the treatment (poor reduction, open treatment, or internal fixation) rather than the natural history.
PATIENT HISTORY AND PHYSICAL FINDINGS
Elucidating the mechanism of injury is important to truly understand the personality of the fracture, which can help in directing treatment. Higher energy mechanisms are more likely to be associated with concomitant injuries. Elbow dislocations that have reduced before presentation are not uncommon, so it is helpful to ask the patient and family whether a marked deformity was noted at the time of injury.
Carefully palpating each anatomic area in the elbow to find the points of maximal tenderness helps diagnose the fracture as well as additional injuries. Associated injuries include medial collateral ligament tears, medial epicondyle fractures, ulnar fractures, and supracondylar humerus fractures. A neurologic evaluation assesses distal radial, medial, and ulnar nerve motor and sensory function.
Assessing elbow stability and range of motion can help determine the need for treatment.
Valgus instability indicates a medial elbow injury in addition to an unstable radial neck fracture.
Blocks in forearm rotation, in particular pronation, are typically due to loss of congruity of the radioulnar joint and indicate a need for reduction.
Stability and range-of-motion assessment may necessitate either an intra-articular anesthetic injection or an examination under anesthesia.
IMAGING AND OTHER DIAGNOSTIC STUDIES
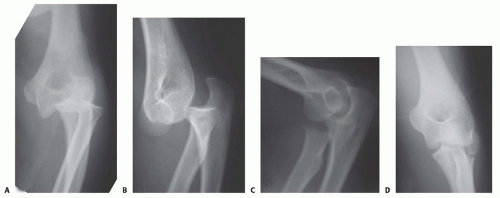
AP, lateral, and oblique radiographs often show radial neck fractures well (FIG 5A,B). However, the true extent of fracture angulation can be underestimated on plain radiographs, as orthogonal views may fail to capture the true plane of angulation.
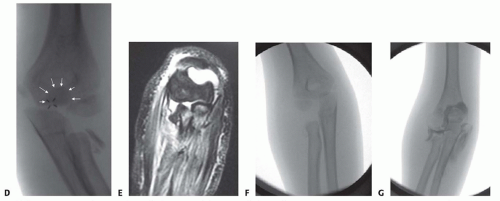
The clinician should carefully rule out associated injuries such as fractures of the olecranon (intra-articular) (FIG 5C,D), proximal ulna, medial epicondyle, or lateral condyle or elbow dislocation.
In posterior elbow dislocations, the clinician should carefully examine the radial neck for an occult fracture that is at risk for displacement during the reduction maneuver.
Radial neck fractures can occur before the ossification of the radial head, without clear evidence of fracture on plain radiographs.
Ultrasound, magnetic resonance imaging (MRI) (FIG 5E), and arthrography (FIG 5F,G) are useful for diagnosing and evaluating radial neck fractures in young patients with nonossified radial heads.
In the operating room, arthrography is useful in outlining the nonossified radial head when monitoring and verifying reduction.
DIFFERENTIAL DIAGNOSIS
The diagnosis of a radial neck fracture is usually easily made with appropriate imaging. However, the presence or absence of the following associated injuries should be ascertained:
Medial collateral ligament rupture
Medial epicondyle fracture
Olecranon fracture
Monteggia equivalent type IV fracture
NONOPERATIVE MANAGEMENT
Ultimately, the objective is to obtain and maintain a congruent joint with restored elbow range of motion in all planes. Most consider up to 30 degrees of angulation and 3 mm of translation as limits of an acceptable reduction.
Controversy exists regarding the exact numbers, however, with reported acceptable angulation ranging from 20 to 60 degrees.1,3,15,21,26,30,31,32,33,34
Two things partially account for the controversy:
The accuracy of the radiographic measurement is variable and depends on whether the radiographic beam is perpendicular to the true plane of the fracture.
Twenty-five degrees of fracture angulation can have variable effects on the congruity of the radioulnar joint, depending on the direction of angulation.
It is therefore important to base the decision of treatment on the functional effects of the angulation rather than a specific number. Any block of pronation or supination warrants a reduction of the fracture, no matter what the radiographic angulation is.
As remodeling potential decreases with advancing skeletal maturity, less residual angulation is acceptable (15 to 20 degrees).9,32
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree