6
Clinical Reasoning and Problem Solving to Prevent Pitfalls in Hand Injuries
Donald Greg Pitts, Jason Willoughby and Ryan K. Morgan
Introduction and Clinical Reasoning
Stages of Wound Healing
The stages of wound healing are commonly placed into three basic categories: inflammatory, proliferation, and maturation (Fig. 6-1).1–4 Therapists should strive be competent in their understanding of the stages of wound healing and how each type of tissue heals at a different rates.1
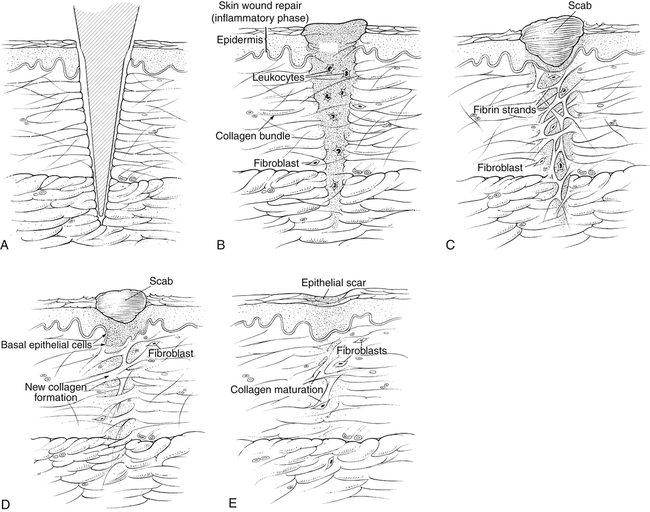
The therapist must place healing timelines on the patient’s pathology based upon classifying healing tissues into either loose or dense connective tissue categories (Fig. 6-2). Loose connective tissues include skin, blood vessels, and muscle.5–7 The normal healing rates for loose connective tissues in the inflammatory phase is between 1 to 3 days, the proliferation phase is between 3 to 10 days, and the maturation phase is from 11 to 21 days. Dense connective tissues include bone, joint capsule, ligament, tendon, and fascia.1,8,9 The approximate healing timeline for dense connective tissues in the inflammatory phase is from 1 to 4 weeks, the proliferation phase is from 4 to 8 weeks, and the maturation phase is from 8 to 12 weeks.
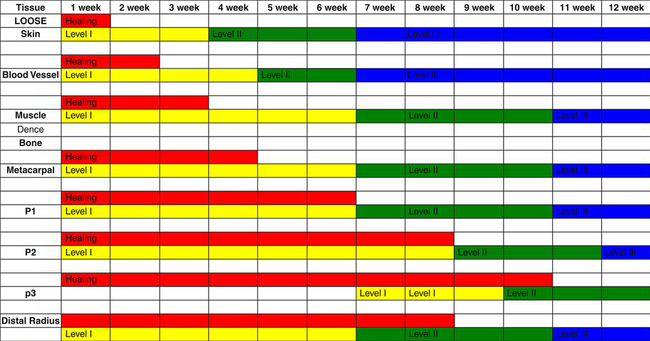
Fig. 6-3 is an example of a clinical-level system for communicating with therapists about therapeutic exercises for use throughout a common pathology of the hand and upper extremity.10
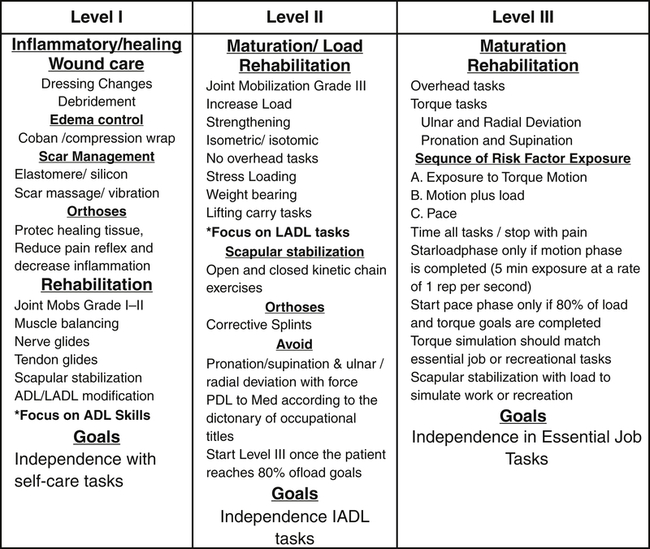
An explanation of the appropriate rehabilitation techniques for various phases of the wound-healing process.
Therapists should consider the occupational environments of the patient at home, work, and play. Clinical education programs provide patients with a clear understanding of tissue healing rates, pathophysiology of injuries, and the expected timelines of functional recovery. Occupational goals and wound healing education are reinforced daily. This promotes intrinsic buy-in throughout the rehabilitation processes, which is vital to facilitating therapist-patient relationships.4,11
Edema
Pathophysiology
According to Dr. Paul Brand, edema is scar in evolution, and if it is left untreated, it will result in adaptive shortening, adhesions, and joint contractures.12–15 Edema routinely occurs during acute inflammatory processes from infections, traumatic injury, or surgery. Edema can also be present from decreased mobility (immobility), systemic diseases, and local infections. Immobility is the primary reason for persisting or persistent dysfunctional edema of the hand from a traumatic injury or post-surgical procedure. Functional hand movement is one of the primary means of edema reduction. Hand movements increase pressure gradients on the arteriole and venous systems creating fluid shifts of pooled edema. This pressure promotes lymphatic flow and also assists the extremely insufficient venous outflow system of the hand.
Systemic edema can result from a non-functional lymphatic system or an autoimmune disease. Systemic edema can be extremely detrimental to hand function due to the prolonged stress on the musculoskeletal system, joints, and nerves.14–16 Prolonged stress may permanently derange the ligamentous structures that stabilize joints and tendon systems that produce functional dexterity 17
Infection
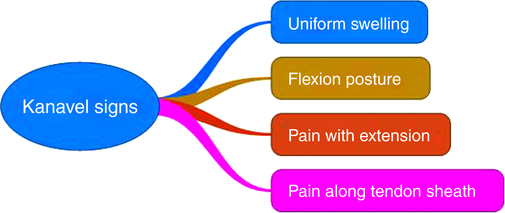
In 1904, Dr. Kanavel first described the identification and evaluation of infectious edema. He described the four cardinal signs of infection as symmetrical edema, flexed digital posture, pain with extension of digit, and pain with palpation along the tendon sheath (Fig. 6-4). The clinician should document the patient’s pain levels on a scale of 0 to 10 at rest and with ADL tasks and note the number of Kanavel signs present. This documentation will allow the therapist to evaluate progression or regression.
Evaluation
Edema may be on the dorsum of the patient’s hands due to the limited lymphatic drainage. Patients displaying persistent edema often develop the classic stiff hand posture. When the hand is subjected to pitting edema, the position of least resistance is often referred to as the loose pack position (Fig. 6-5).7,18 Edema diminishes the capacity for functional tendon excursions by a phenomenon known as fabric bias.15,18
The stiff hand (open pack) posture presents with the metacarpal joints in extension due to edema pooling in the dorsum of the hand and stress applied to the extrinsic extensor mechanism.15,19,20 The proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints are in a flexed posture with the edema stress creating a tenodesis effect on the extrinsic flexors fron the fabric bias stress on connective tissue.21
The stiff hand posture can be extremely problematic due to the open-pack non-stressed position of the collateral ligaments supporting the metacarpophalangeal (MP), PIP, and DIP joints.7 This may lead to insufficient glides of contractile tissues (tendon, muscle) and stress deprivation of non-contractile tissues (joint capsule, ligamentous structures).15,18,22
These pitfalls may result in joint contractures, tendon adhesions, and long-lasting pain reflexes inhibiting functional outcomes with ADLs and meaningful occupations. Therapists must evaluate the effects of the edema and adjust the patient’s treatment plans on a daily basis in order to diminish the chances of the stiff hand posture pitfalls.2,8
Physical Examination
When assessing the effects of edema on ligamentous structures of the hand, evaluators should place the MP joints in the maximum allowable flexed position and the PIP and DIP joints in maximum extension.14,15,18,22 Therapists should attempt to place the hand in the commonly referred safe position for long-term functional outcomes.
The standard edema evaluations for hand injuries are volumetric and active range of motion (AROM) (Fig. 6-6). According to Waylett-Rendall and Seibly, volumetric testing has been found to have a high level of inter-/intra-rater reliability and repeatability.23 Often volumetric devices are not feasible due to open wounds from injury or surgery. Therapists should consider AROM and passive range of motion (PROM) of the digits with the evaluations of fingertips to distal palmar crease (DPC) and palmar digital crease (PDC) (Fig. 6-7). These evaluations allow therapists a fast and reliable way to determine the negative impact edema has on functional movement.
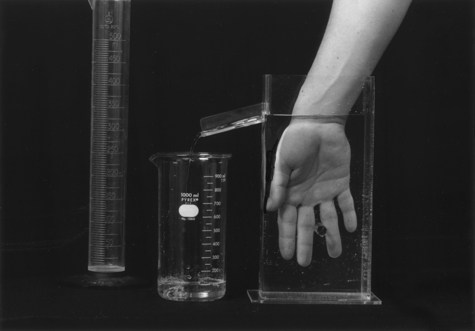
A volumeter is used to measure edema in the hand by comparing the amount of water displacement by the affected to the unaffected extremity. (From Fess EE, Gettle KS, et al: Hand and upper extremity splinting: principles & methods, 3e, St. Louis, 2005, Mosby, Inc.)

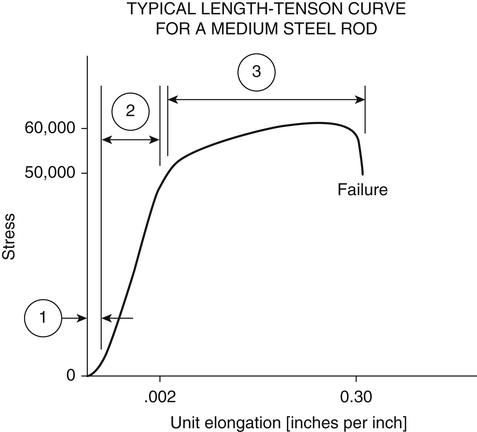
Dr. Brand describes a clinical evaluation of edema based upon the viscoelastic properties of loose and dense connective tissues. He describes the application of graded force to joints over a set time. He recommends recording torque range of motion (TQROM) obtained with a force gauge and plotted on a graph.12,24,25 The type of tissue and edema involved is based on the shape of the plotted TQROM timed stress strain curve (Fig. 6-8 and Fig. 6-9). A long shallow curve with a gradual peak at the end range will indicate a loose connective tissue problem (soft-end feel). This is demonstrated with an end range can be reached at a fast rate, the edema is fluid in nature and may respond to mobility and compression. A steep curve with an often painful hard end range reached at a slow sluggish rate indicates the edema is mature and protein-filled with great potential for stiffness.14,15,18
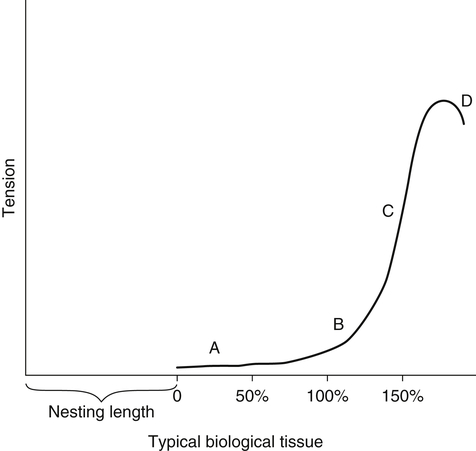
The diagram demonstrates a gradual stress strain curve with a slow slope to peak, which is characteristic of loose connective tissue with a soft-end feel of resistance.
Scarring
Scar tissue can alter tendon glide and change joint function (see Fig. 6-10).26–28 If the scar is not stressed appropriately in the early phase (inflammatory) of rehabilitation process, non-functional adhesions and joint contracture can result limiting function.14,15, 29,30 Scar tissue will respond to gentle graded stresses at the early stages of the rehab process. Stress application to a mature scar will take longer and be less predictive to realize effective change. Rehabilitation programs with aggressive stress can keep the tissue in an inflamed state longer or create an inflammatory state in mature tissue thus creating excessive scar tissue.
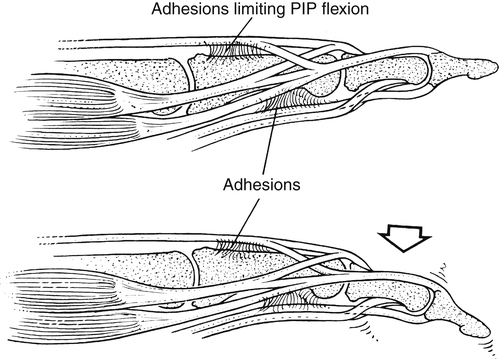
This picture demonstrates how adhesions form surrounding a proximal interphalangeal (PIP) restricting gliding structures of both extensor and flexor mechanisms. (From Fess EE, Gettle KS, et al: Hand and upper extremity splinting: principles & methods, ed 3, St. Louis, 2005, Mosby, Inc.)
The evaluating therapists must understand that the position of the proximal joints directly impacts length-tension relationship of the extrinsic muscles affecting joint positions.22 As an example, if positioning the MP joint in extension limits flexion of PIP but if MP flexion yields increase in PIP flexion, this indicates intrinsic tightness. If movement of a distal joint is not altered by proximal joint position, then adhesions in the joint structures is probable. 14,15
Dr. Brand pioneered the evaluation techniques necessary to implement a treatment plan to target specific altered tissue types with the application of progressive stress (Fig. 6-11). The controlled application of stress plotted on a stress strain curve can clearly identify the maturation of the scar, tissue type, and rehabilitation approach needed to avoid a pitfall.14,15 If the curve plotted is long with a gradual slope and a soft-end feel, then the problem is mechanical stiffness. If the curve plotted is shallow with a steep slope and a hard-end feel, then the problem is biological stiffness.31–35
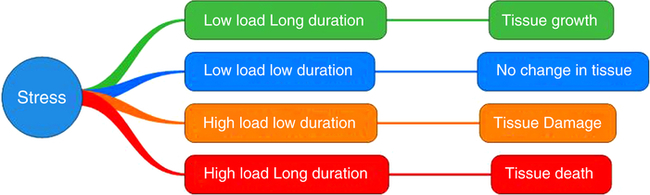
Therapists often use the concept of low load long duration (green) to facilitate a change in tissue length and tissue growth. The use of low load low duration will result in no change in tissue growth or length (blue). The use of high load low duration can result in tissue damage (yellow). If the stress is too aggressive and or long duration, this can lead to tissue death (red). (From Pitts G, Willoughby J: Rehabilitation of wrist and hand injuries. In Andrews J, Harrelson G, Wilk K: Physical rehabilitation of the injured athlete, ed 4, Philadelphia, 2012, Saunders.)
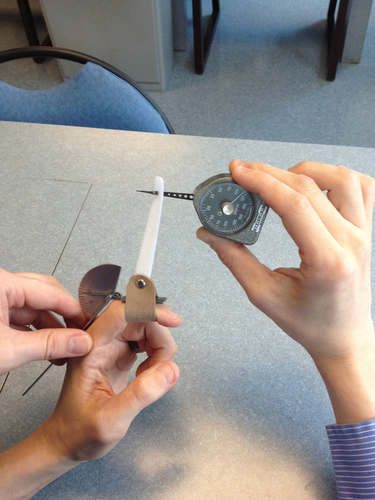
Stress application measured with a Haldex gauge and a goniometer allows therapists to plot changes in joint motion with the application of progressive measured force (Fig. 6-12). The data plotted will allow the treating therapist to determine if the lack of functional motion is due to loose or dense connective tissue. This allows proper selection and type of force when fabricating dynamic and static progressive orthoses (Fig. 6-13).10,18

Force application is effective in addressing joint stiffness and controlled safe tissue elongation.
Scar tissue can have direct negative impact on tendons with attempted functional movement. These types of pitfalls include gliding structures through scar, scar in gliding structures, and nerve glide through scar. Examples of gliding structures through scar include flexor and extensor tendon adhesions. Examples of scar in gliding structures include de Quervain tenovaginitis and trigger finger tendonitis .15,36
Examples of nervous tissue gliding through scar include digital nerve repairs, carpal tunnel syndrome, and cubital tunnel syndrome. This simple classification of scars when applied can assist therapists in the selection of proper treatment approaches to avoid functional impairments that limit social roles.37
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree