Chapter 4 Clinical Assessment of the Elbow
Physical examination
General examination of the elbow
Inspection
Inspection requires appropriate exposure of the cervical spine, shoulder, elbow, wrist and hand. When assessing the skin, notable features include skin integrity, quality, pigmentation, scars or incisions, fistulas or sinuses, masses or ecchymosis. As an example, depigmentation may occur as a result of prior corticosteroid injections (Fig. 4.1).
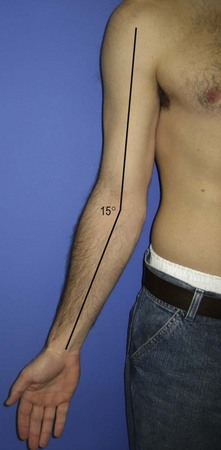
Assessment of the patient’s carrying angle (Fig. 4.2) is also important and should be compared to the contralateral elbow. It is measured with the arm adducted and externally rotated, the elbow extended, and the forearm supinated. The carrying angle is the angle formed by the long axis of both the arm and the forearm. Although there is with some dispute amongst authors as to whether differences exist between the sexes,1–3 the normal ranges for men and women are 10–15° of valgus. Some patients may demonstrate excessive cubitus valgus or cubitus varus as a result of previous trauma or disorders of physeal growth. Some overhead-throwing athletes have an increased physiological valgus carrying angle.4
Palpation
A systematic approach to palpation will ensure that no significant abnormality is missed. Table 4.1 provides a list of structures to include in the examination. On the lateral aspect of the elbow, the key anatomic landmarks to palpate are the lateral epicondyle, lateral collateral ligament, radial head, lateral soft spot (Fig. 4.3), crista supinatoris and the common extensors (Fig. 4.4).
Table 4.1 Structures to include during palpation of the elbow joint
| Lateral |
| Posterior |
| Medial |
| Anterior |
On the medial aspect of the elbow, the key structures are the medial epicondyle, the ulnar nerve (Fig. 4.5), the sublime tubercle and the flexor–pronator group. The latter is best visualized when placed under tension (Fig. 4.6).
Anteriorly, the coronoid (Fig. 4.7) is important to palpate, as is the distal biceps tendon (Fig. 4.8).
Motion
Determining the range of motion of the elbow is incomplete without an assessment of the range of motion of the cervical spine, shoulder and wrist. The use of a goniometer is helpful in collecting reproducible data that may be used for comparison in subsequent visits. The standard deviation of error for a single observer using a manual goniometer is 3.7° for any joint. With respect to the elbow, the standard deviation of measurement error varies with each motion. The following are the reported standard deviations of measurement error for elbow extension, flexion, pronation and supination, respectively: 2.7°, 4.9°, 5.3° and 4.0°. Given the imprecision of these measurements, Boone and Azen recommend that a single observer should perform repetitive measurements over successive encounters.5
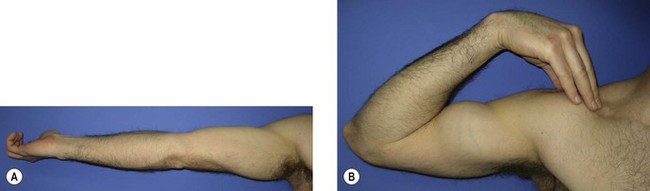
Documenting the range of motion with standardized methods is important to ensure consistency of information across clinic visits and providers. The American Academy of Orthopaedic Surgeons defined these standards in 1965.6 In 1979, Boone and Azen studied normal elbow range of motion in 109 normal subjects. In patients older than 19 years, the flexion–extension arc measured from 0° (full extension) to 140° (full flexion) (Fig. 4.9). Flexion was significantly greater (145°) in subjects younger than 19 years.5 Patients with some generalized ligamentous laxity may demonstrate hyperextension of the elbow, and this should be indicated with negative values (e.g. −10°). The functional arc of motion, allowing for most activities of daily living, is 30–130°.7
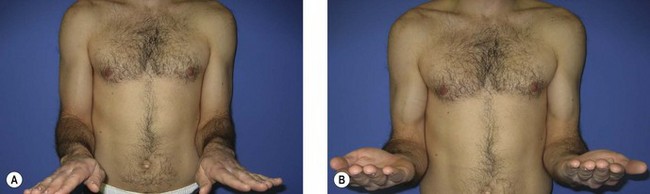
In a normal examination, most patients should achieve approximately 75° of pronation and 82° of supination (Fig. 4.10).5 Although it may appear that patients achieve 90° of rotation when observing the final hand position, as much as 15° of rotation is generated through the carpus and does not represent isolated forearm rotation. The functional arc of motion for forearm rotation is 50° of pronation to 50° of supination.7 It is important when pronation and supination are being measured that the patient’s elbow is flexed to 90° and at their side, since many patients will abduct or adduct the shoulder to compensate for loss of forearm rotation.
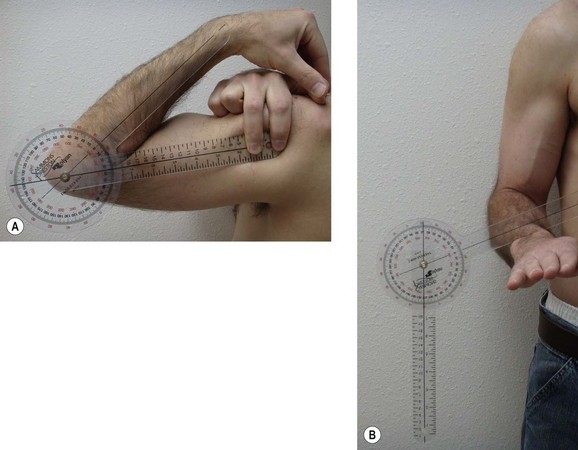
When using the goniometer to measure angles, consistent surface landmarks should be used to ensure that the arms of the goniometer are parallel to the humeral and ulna diaphyses. In muscular or overweight patients, it can be difficult to palpate the humeral shaft and it is better to use the anterolateral corner of the acromion as a reproducible landmark as it represents the approximate location of the humeral shaft. The hinge of the goniometer is placed at the rotational axis of the patient’s elbow, which is approximated by the lateral epicondyle. The distal arm of the goniometer is aligned with the subcutaneous border of the ulna. This is usually easy to see and palpate regardless of the patient’s body habitus. Flexion and extension should be measured with the forearm in supination (Fig. 4.11A). Measuring forearm pronation and supination should be done with the elbow at the patient’s side and in 90° of flexion. The goniometer arm should be placed parallel to the plane of the volar or dorsal aspect of the distal radioulnar joint and the other arm directed either downward with gravity (perpendicular to the floor) or upward (perpendicular to the ceiling) (Fig. 4.11B).
Neurological
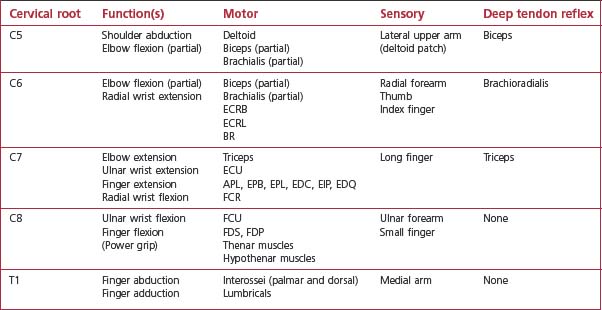
A complete neurological examination of the upper extremity should be conducted. This includes cervical roots C5–T1, the brachial plexus and the peripheral nerves. The accompanying tables are provided to guide in the examination of individual cervical roots (Table 4.2), as well as the individual peripheral nerves (Table 4.3).
An important part of the neurological examination is an assessment of strength. This is done with the patient’s elbow flexed 90° and the arm adducted at the side. Table 4.4 lists some common associations regarding elbow strength assessment.
Table 4.4 Strength assessment8
| Elbow strength assessment | Relative strength |
|---|---|
| Extension | 70% of flexion |
| Pronation | 85% of supination |
| Non-dominant arm | 90% of dominant arm |
Clinical assessment of specific elbow disorders
Epicondylosis
Lateral epicondylosis (tennis elbow)
Provocative manoeuvres include resisted wrist and long finger extension. Both of these will be more painful for the patient when the elbow is extended (Fig. 4.12). In addition, the examiner should check passive stretch of the ECRB by extending the elbow and passively flexing the patient’s wrist with the forearm in pronation. Each of these three manoeuvres should elicit pain over the ECRB origin and re-create the patient’s typical symptoms. Grip strength is a very useful objective test to evaluate response to treatment and recovery of function.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree