CHAPTER 18 Chondrocyte Transplantation Techniques
Developing concepts and methods that can restore hyaline articular cartilage has been the goal of researchers and clinicians for centuries.1 In 1994, Brittberg and coworkers2 reported on the first successful use of autologous chondrocytes in human subjects with full-thickness articular cartilage lesions of the knee using a two-step implantation technique. Since its first description, chondrocyte transplantation has been performed in more than 15,000 patients worldwide and many research studies have clinically validated this surgical technique as a reliable method for biologic restoration of hyaline-like articular cartilage.3–13 Based on the evolution and better understanding of the treatment of articular cartilage defects and cell-based implantation techniques in recent years, this demanding surgical technique has undergone several technical modifications. These recent developments can help reduce patient morbidity and technique-specific complications. Chondrocyte implantation techniques continue to evolve using modern tissue engineering technologies.
PATIENT EVALUATION
Diagnostic Imaging
Plain radiographs, including weight-bearing anteroposterior (AP) and lateral views, Rosenberg and tunnel views, long-leg films, and Merchant views, can help identify osteochondral lesions, joint space narrowing, patellar maltracking, or lower extremity malalignment. Cartilage-sensitive magnetic resonance imaging (MRI) presents a sensitive, specific, and accurate tool for noninvasive diagnosis of articular cartilage injury.14,15 Images should be obtained in three planes; using fast spin-echo imaging with a repetition time (TR) of 3500 to 5000 msec and moderate echo time (TE) provides high contrast resolution among articular cartilage, subchondral bone, and joint fluid. Cartilage-sensitive MRI provides useful information about meniscal and ligamentous status, subchondral bone, lesion size, and depth Because of the pathologic changes in the surrounding cartilage, the final size of the defect intraoperatively is usually larger than the defect size measured on preoperative MRI. In addition to its use for preoperative diagnosis, cartilage-sensitive MRI can be helpful for postoperative evaluation of cartilage repair. Routine postoperative MRI is recommended to evaluate the cartilage repair tissue and detect potential complications, such as graft hypertrophy. If available, newer technologies, such as T2 mapping, delayed gadolinium-enhanced MRI of cartilage (dGEMRIC), and T1 rho relaxation mapping, can be used to obtain additional details about cartilage morphology pre- and postoperatively.15
TREATMENT
Indications and Contraindications
Chondrocyte implantation is indicated for symptomatic, high-grade chondral and osteochondral defects of the knee in active patients who are physiologically too young for arthroplasty. This technique can be successfully used as a first-line treatment of femoral condylar, trochlear, and patellar lesions larger than 2 cm2, or used as a revision technique for failed prior cartilage repair procedures.8,11–13 The technique can be successfully used for isolated, multiple, and kissing cartilage defects. Prerequisites for successful autologous chondrocyte transplantation include adequate range of motion, appropriate axial alignment or patellar tracking, ligamentous stability, and the ability to comply with the postoperative rehabilitation protocol. Adjuvant procedures may be indicated to correct coexisting knee pathology; these can be performed simultaneously with chondrocyte transplantation without negative effects of the complex procedures on the postoperative functional outcome and activity level.
Arthroscopic Technique
Autologous chondrocyte transplantation of the knee is carried out as a two-stage procedure.
Stage 1: Chondrocyte Harvest
Step 1. Arthroscopic Evaluation.
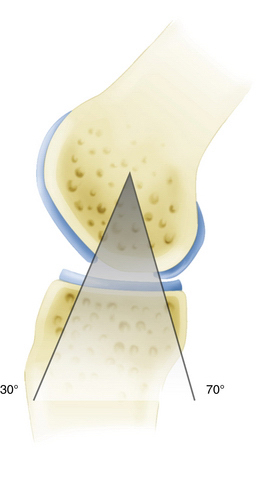
The first stage involves a thorough diagnostic arthroscopy. In addition to identification of the known articular cartilage defect, the meniscal and ligamentous status is evaluated and the entire articular cartilage is inspected to rule out any additional cartilage defects. Partial meniscectomy or meniscal repair can be performed at the time of this arthroscopy because it minimally affects the course after the initial arthroscopy and can decrease operative time during the second-stage procedure. However, surgical treatment of meniscal deficiency or ligamentous pathology should be performed simultaneously with autologous chondrocyte implantation to avoid repetitive operative joint trauma and prolonged rehabilitation. During the first-stage arthroscopy, the cartilage defect is identified and existing cartilage flaps are débrided back to a stable and healthy peripheral margin. Following thorough débridement, the size of the articular cartilage lesion is measured and its containment documented. The knee is taken through a full range of motion and the arc of motion during which the lesion articulates with the opposing joint surface is carefully recorded (Fig. 18-1). The opposing joint surface should always be carefully inspected for the presence of a kissing lesion or signs of low grade cartilage injury.