Chiari Medial Displacement Osteotomy of the Pelvis
Travis H. Matheney
Brian Snyder
DEFINITION
The Chiari osteotomy is primarily a “salvage” osteotomy for acetabular dysplasia in the painful, unstable hip.
It is generally reserved for hips where a congruous reduction is not possible because of arthrosis or femoral head asphericity that prevents use of one of the more standard rotational osteotomies.1, 4, 5
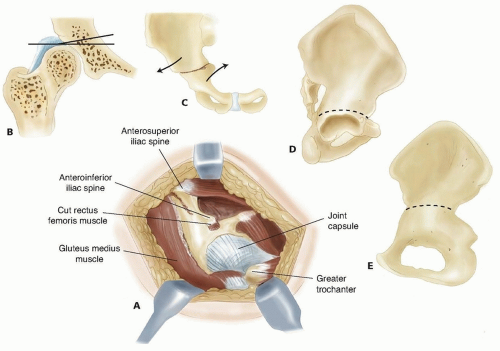
It is a single pericapsular osteotomy through the iliac (innominate) bone of the pelvis with medialization of the acetabulum and hip joint to improve posterior and lateral coverage. The ilium forms a shelf over the dysplastic, subluxated hip (FIG 1).
The goals are improved femoral head coverage, a stable articulation, and metaplastic transformation of the hip capsule to fibrocartilage to create a stable, pain-free hip.
Contraindications include severe arthrosis, age older than 45 years (relative, where arthroplasty may be a better option), and significant proximal migration of the femoral head (may prevent adequate coverage by thinner proximal ilium).5
ANATOMY
Developmental acetabular dysplasia most commonly involves deficiency of the anterior and anterolateral acetabulum.
In cases of spastic hip dysplasia, the lateral and posterolateral acetabulum is most often deficient.
The location of acetabular deficiency must be considered when planning the shape and orientation of the osteotomy and positioning of the iliac shelf over the hip joint.
Femoral head deformity may include coxa breva, coxa magna, or coxa plana.
In cases of trochanteric overgrowth, simultaneous advancement of the greater trochanter may provide improved abductor mechanics (although the risk of heterotopic ossification may be slightly increased).
This osteotomy may not provide adequate coverage in cases of high dislocation and in the pelvis in patients with advanced neurologic conditions (eg, myelomeningocele, where the ilium is very thin above the acetabulum). Therefore, careful
consideration of the available periacetabular bone stock should be made before considering the Chiari osteotomy.
The need for additional bone graft to supplement posterior, lateral, and (especially) anterior coverage is common.
This procedure does not require concentric reduction of the femoral head into the acetabulum.
It has the advantage of medializing the femoral head and decreasing the force across the hip joint by increasing the surface area of coverage.
Lateralizing the ilium to form a shelf causes obligatory shortening of the gluteal muscle length and abductor moment arm that weakens the muscle and contributes to postoperative Trendelenburg limp. However, advancing the greater trochanter can restore the resting length of the gluteus medius. Delp et al3 found that decreasing the obliquity of the supra-acetabular osteotomy may decrease the effect on the abductor lever arm.
PATHOGENESIS
The causes of advanced hip disease requiring salvage surgery are many and include late diagnosis of developmental dysplasia of the hip (DDH), spastic or neuromuscular hip dysplasia, failed prior hip procedures (reduction, periacetabular osteotomy), and acetabular trauma.
Femoral head conditions that can lead to incomplete or incongruous femoral head coverage include primary malformation, secondary avascular necrosis, slipped capital femoral epiphysis, epiphyseal-metaphyseal dysplasia, and secondary malformation from long-standing subluxation or impingement.
NATURAL HISTORY
Because this osteotomy is used as a salvage procedure for many hip diseases, it can be used to treat any of the several conditions that result in progressive, painful arthrosis and instability.
The threshold of acetabular dysplasia required to induce arthrosis is incompletely understood. However, when assessing lateral uncovering, Murphy et al6 found that a lateral center-edge angle less than 16 degrees on an anteroposterior (AP) view of the pelvis correlated with a significantly increased risk of requiring arthroplasty by age 65 years.
Spastic hip dysplasia can lead to progressive subluxation and painful dislocation in 30% to 50% of cases. It is more common in nonambulatory patients.
PATIENT HISTORY AND PHYSICAL FINDINGS
Key portions of the history include the following:
Personal or family history of or treatment for DDH
History of other hip disorders, including Legg-Calvé-Perthes disease
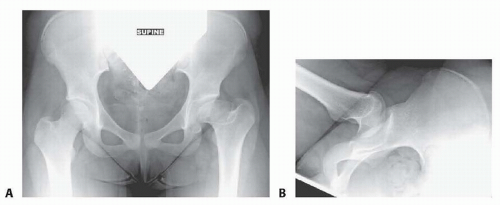
FIG 2 • A. AP radiograph of bilateral hips and pelvis of patient with right hip with Legg-Calvé-Perthes disease. B. Frog-leg lateral radiograph of left hip with Legg-Calvé-Perthes disease.
Trauma
Skeletal dysplasias
History of cerebral palsy
Birth order and weight
Description of pain and mechanical symptoms, including location, duration, activity limitation, giving way, clicking, catching, and popping
The physical examination should include gait, limb length, assistive devices, and strength.
Specific hip tests include the following:
Trendelenburg test: demonstrates weakness in abductors
Anterior apprehension test with extension and external rotation of the hip: A positive result is a subjective noting of “apprehension” or instability by the patient.
Gluteus medius and maximus strength
Anterior impingement test (pain with passive hip flexion, adduction, and internal rotation): test of anterior labral pathology, not just a tear
“Bicycle test” for abductor fatigability of the hip while lying in the contralateral decubitus position
Range of motion: It is important to test internal and external rotation at multiple degrees of flexion, as femoral head and acetabular deformities vary. This can often aid in determining where the pathologic articulation is located.
Galeazzi sign: demonstrates hip subluxation or dislocation
The Chiari osteotomy can increase abduction. It does not always significantly improve range of motion in other planes, and therefore preoperative flexion to 90 degrees, full (or near full) extension, and at least 10 to 20 degrees of adduction are requirements.
Gait is assessed preoperatively. It is important to discern whether any limp is antalgic, due to abductor weakness or instability. The Chiari osteotomy classically can improve antalgia and instability. However, the patient should understand that abductor weakness may not be improved.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiography should include weight-bearing AP views of bilateral hips, false profile of hips, and AP of hips in maximal abduction and internal rotation (FIG 2). These studies allow assessment of lateral and anterior coverage of the femoral head as well as congruency of the hip joint. Also noted will be the presence of hinge abduction.
Computed tomography (CT) scan with three-dimensional reconstruction may help in preoperatively assessing the amount and direction of acetabular deficiency.
Magnetic resonance imaging (MRI) of involved hips with radial sequences centered at the femoral head can also help with preoperative assessment of articular and labral cartilage.
DIFFERENTIAL DIAGNOSIS
DDH
Spastic hip dysplasia
Legg-Calvé-Perthes disease, avascular necrosis
Multiple or spondyloepiphyseal dysplasia
Posttraumatic hip or femoral dysplasia
NONOPERATIVE MANAGEMENT
The patient being considered for Chiari osteotomy usually presents with pain and arthrosis.
Activity and job modification and weight loss may be of benefit in delaying or mitigating the onset of arthritic symptoms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree