Carpal Tunnel Release: Endoscopic, Open, and Revision
Marco Rizzo
DEFINITION
Carpal tunnel syndrome (CTS) is a compressive neuropathy of the median nerve at the wrist.
CTS is the most common nerve compression condition in the upper extremity.
Carpal tunnel release (CTR) is one of the most commonly performed procedures in the United States.
Early stages of CTS are reversible with treatment.
Later or more severe stages of CTS may not be (fully) reversible.
ANATOMY
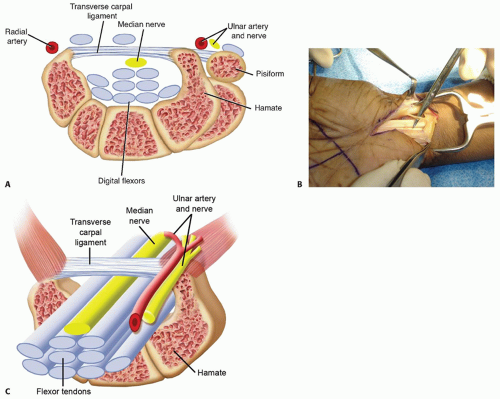
The carpal tunnel or carpal canal is a space bounded by the carpal bones dorsally, the trapezium and scaphoid radially, the hook of the hamate ulnarly, and the transverse carpal ligament (TCL) palmarly (FIG 1A).
The contents of the carpal canal includes the median nerve and nine digital flexor tendons, along with their accompanying tenosynovium (FIG 1C).
Anatomic anomalies include the following:
A persistent median artery
Muscle anomalies
Median nerve branching anomalies (FIG 1B)
Extraneous masses or structures may be found within the carpal canal, including sarcoid and ganglion cysts.
Arthritis or bone spurs from the carpus can diminish the size of the carpal canal and established associations between basal thumb arthritis and CTS exist.3
PATHOGENESIS
NATURAL HISTORY
CTS may have a variable course. It can improve, remain stable, or become more severe.
Severity of compression, age, and patient comorbidities help predict natural history.
Patients with severe CTS have motor and sensory changes and may have muscle weakness and atrophy.11
Patients with extremely advanced CTS frequently have constant numbness, thenar weakness, and readily visible atrophy.
HISTORY AND PHYSICAL FINDINGS
Presenting symptoms can be variable: Some patients with mild CTS present with moderate to severe pain, numbness, and paresthesias, whereas other patients have minimal symptoms until their syndrome is severe.
Symptoms are based in part on severity of disease.
Mild disease
Intermittent numbness and tingling
Provocative symptoms when driving, holding objects, and nocturnal waking
Moderate disease
Numbness and tingling become constant
+/− provocative symptoms
Severe disease
Dense constant numbness
Frequent absence of provocative symptoms
Thenar muscle atrophy with weakness and loss of dexterity
Obtain a full medical history to identify for risk factors for CTS such as hypothyroidism and diabetes.
The surgeon must understand the patient’s occupational and recreational hand activities and any antecedent trauma that might contribute to symptoms.
It is helpful to inquire about activity(s) that trigger symptoms.
Obtain a sense of symptom progression and severity.
Questions should be asked about sensory and motor function, pain pattern, and nocturnal waking.
The physical examination includes evaluation of the neck and shoulder girdle; the supraclavicular, infraclavicular, and axillary area; the humerus and elbow; the forearm; and the wrist and hand.
It is important to generate a list of findings that may be responsible for the pain or paresthesias other than CTS.
In addition to the standard joint evaluation with range of motion and assessments of stability, it is important to palpate the course of the nerves and elicit the Tinel sign along the course of the paracervical, brachial plexus, median, ulnar, and radial nerves.
The Tinel sign is mild, moderate, or severe based on subjective findings of radicular pain in an anatomic distribution. In a patient with peripheral neuropathy, the mechanical external stimulus threshold for nerve depolarization-repolarization is lowered.
Phalen sign: Wrist flexion decreases the volume of the carpal canal and raises pressure in patients with CTS. The pattern of paresthesia is important.
Carpal tunnel compression test: This is generally considered one of the most sensitive and specific tests for CTS.
Two-point discrimination: In peripheral neuropathy, the ability to distinguish one or two points is often diminished.
Decreased range of motion, crepitus, and palmar wrist swelling can be indirect indications of tenosynovium in the carpal canal or intra-articular wrist pathology.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Anteroposterior (AP), lateral, and oblique radiographs are not mandatory in the workup if the wrist examination is completely normal. If there is any possibility of wrist pathology, these studies should be obtained.
Other imaging studies are generally not indicated in routine cases. However, in patients with recurrent CTS, magnetic resonance imaging (MRI) or ultrasound should be considered as a means to gain further information regarding a complete versus incomplete release of the TCL or evidence of median nerve compression, tenosynovitis, and scarring.1 Ultrasound has the advantage of providing a real time and dynamic analysis of the nerve and tendons in the carpal tunnel.10
Electrodiagnostics: Nerve conduction studies (NCS) and electromyography (EMG) are important. CTS can be graded based on NCS and EMG findings:
CTS mild: increased sensory or motor distal latency; may see decreased amplitude
CTS moderate: increased nerve conduction velocity
CTS severe: EMG shows signs of chronic denervation with positive fibrillations and sharp waves or unobtainable recordings from the electrodes to median innervated muscles.
Although some experts believe the absence of any of the earlier electrodiagnostic findings means that there is no CTS, others believe that false-negatives exist due to sensitivity issues with NCS and EMG.5
DIFFERENTIAL DIAGNOSIS
Cervical radiculitis
Cervical pathology, joint disease, disc disease, facet disease with foramina stenosis
Thoracic outlet syndrome
Brachial plexopathy
Syringomyelia, motor neuron disease, myelopathy
“Double crush syndrome”
Shoulder pain related to instability, intra-articular pathology, subacromial impingement
Acromioclavicular joint pathology
Medial epicondylitis
Lateral epicondylitis
Cubital tunnel syndrome
Radial tunnel syndrome
Pronator syndrome
Elbow pathology instability or contracture
Forearm or wrist tenosynovitis
Wrist tenosynovitis, extensor, flexor, or de Quervain tenosynovitis
Digital tenosynovitis (trigger finger)
Guyon canal syndrome
Hypothenar hammer syndrome
Wrist or carpal fracture
Intra-articular wrist pathology
NONOPERATIVE MANAGEMENT
Activity modification can be attempted, especially if the activity includes highly repetitive loading of the hand, wrist, and upper extremity.
Wrist splints can be introduced.
The physician can recommend or prescribe nonsteroidal anti-inflammatory drugs (NSAIDs).
Corticosteroid injection into the carpal canal can be considered (FIG 2).
Temporary relief from such an injection indicates that surgical decompression is likely to be successful.
Hand therapy can be considered.
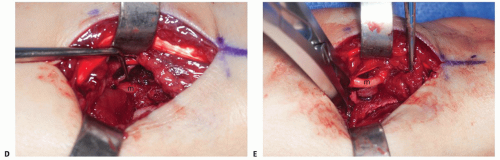
SURGICAL MANAGEMENT
The diagnosis of CTS is confirmed by either the presence of classic clinical symptoms and clinical signs or positive NCS or EMG studies.
If the NCS or EMG findings are negative, at least one trial of corticosteroid injection should be considered to evaluate the clinical response. In addition to having a potential therapeutic benefit, it likely has prognostic value for surgery.
It is important to confirm that a trial of conservative treatment has been undertaken without significant improvement or cure.
The surgeon should confirm that differential diagnoses have been considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree