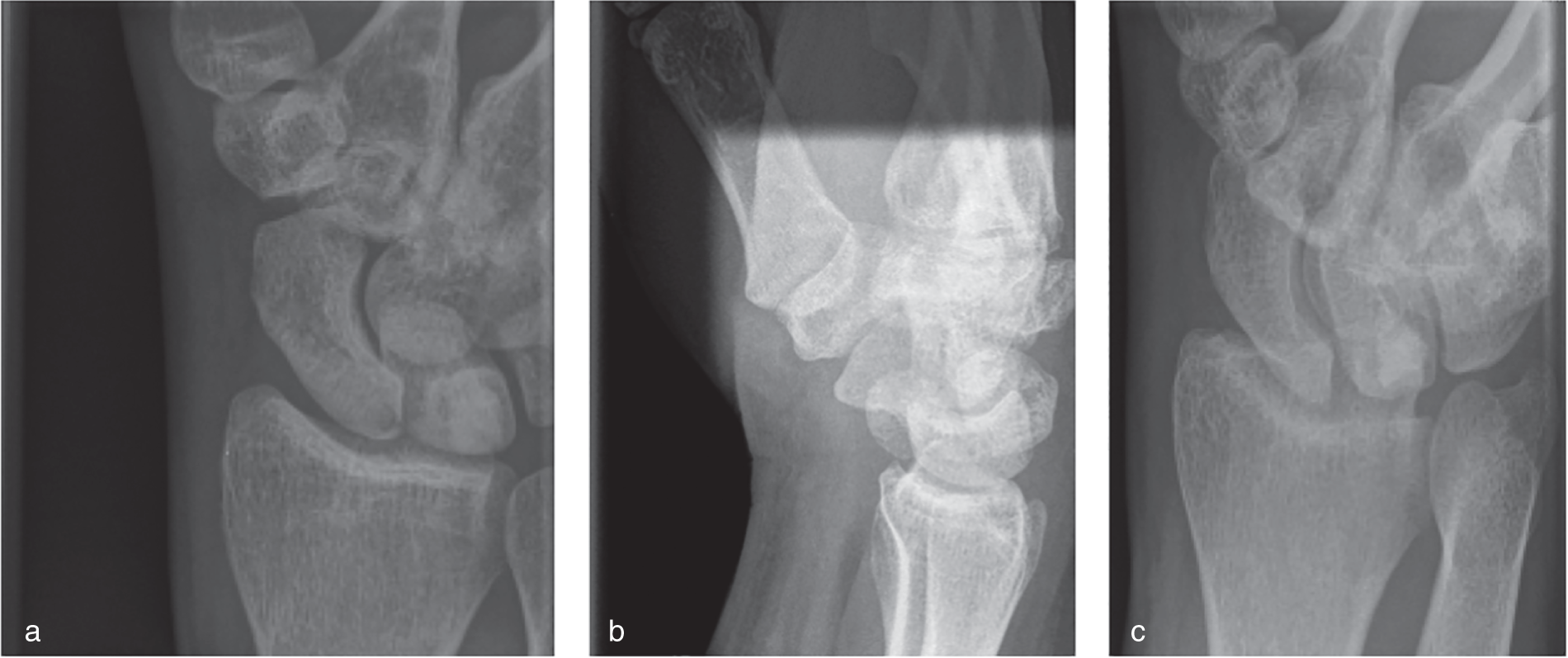
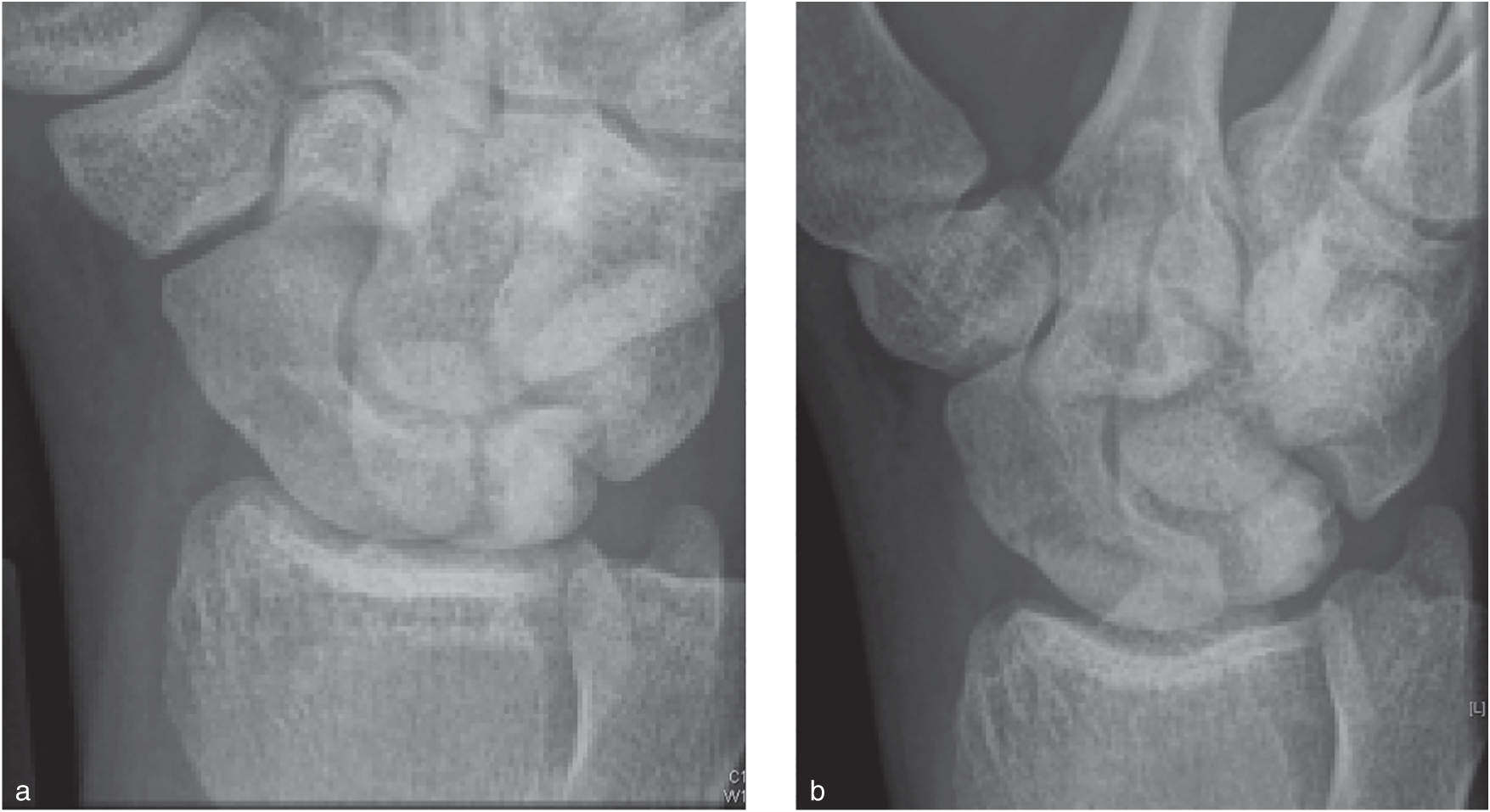
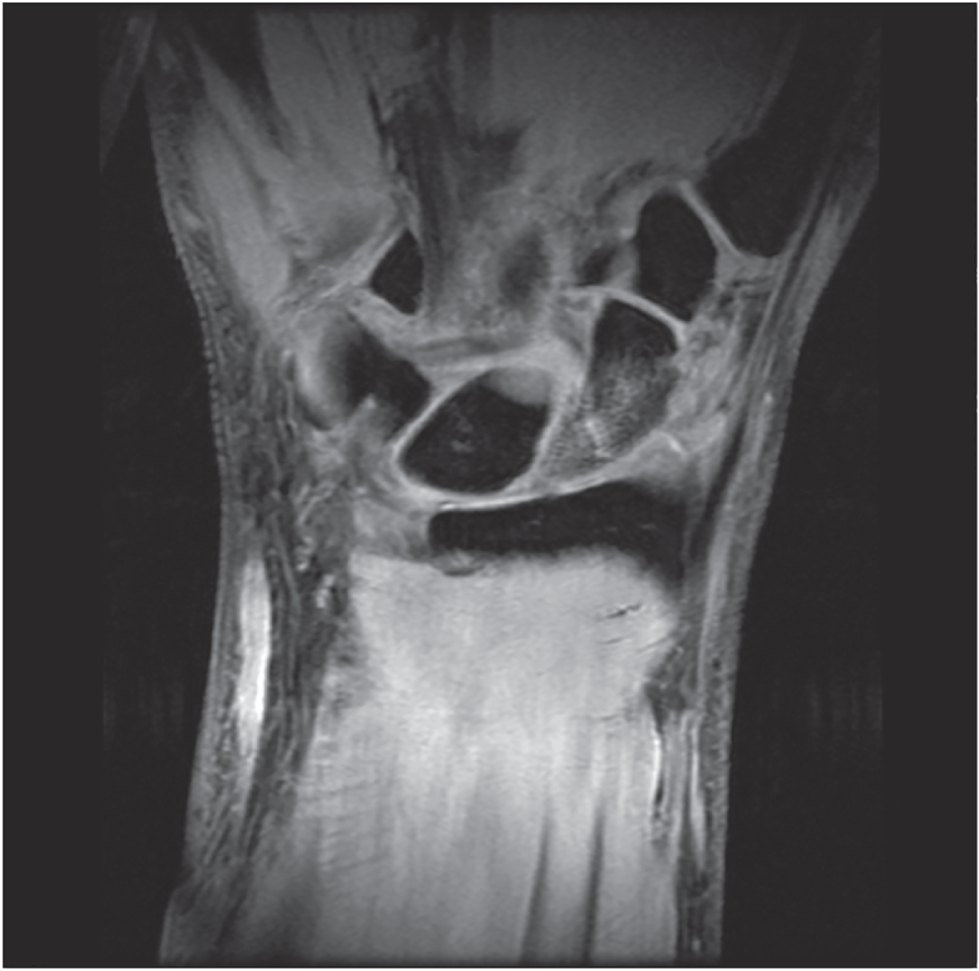
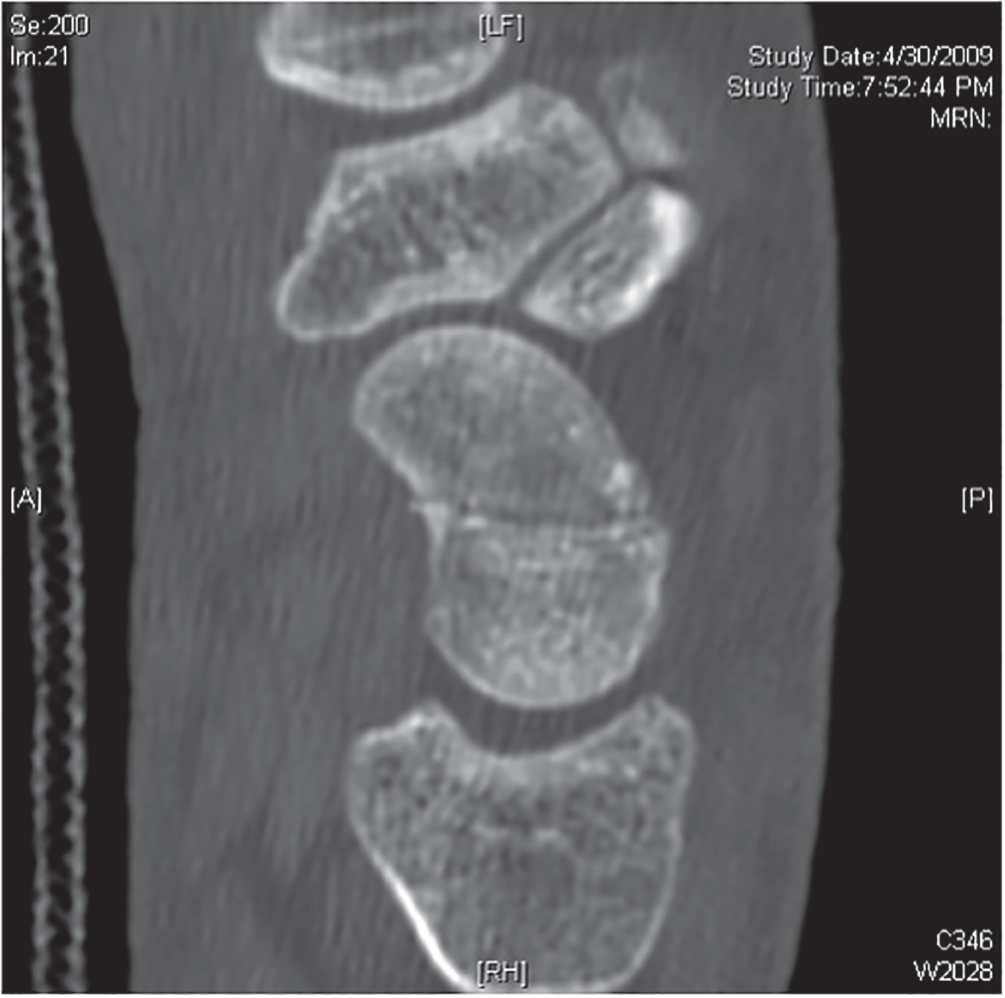
Bert Perey MD FRCSC1, Emanuelle Villemaire‐Côté MD FRCSC2 and Francesc A. Marcano‐Fernández MD PhD3 1University of British Columbia, BC, Canada 2Department of Orthopaedics, CHU de Québec‐Université Laval, Quebec, Canada 3Division of Orthopaedic Surgery, McMaster University, Hamilton, ON, Canada A missed scaphoid fracture can have adverse outcomes. It is generally accepted that a delay in diagnosis and treatment of scaphoid fractures can lead to nonunion or malunion resulting in symptomatic osteonecrosis, carpal collapse, or secondary osteoarthritis. This underlines the importance of an accurate and prompt diagnosis. Patients presenting with a clinically suspected scaphoid fracture, but negative initial radiographs, are treated with temporary cast immobilization for 10–14 days before a second set of radiographs is performed. The patient’s radiographs are initially negative. You are planning to immobilize the patient in a cast and reassess him in two weeks with repeat radiographs (Figure 89.2), but you are wondering if an immediate bone scan, computed tomography (CT) scan, or MRI would be more appropriate. Figure 89.1 PA in ulnar deviation (A), lateral (B), and scaphoid (C) view of the right scaphoid. Figure 89.2 Pronated oblique view of the same patient in Figure 89.1: (A) following the injury, there was a doubt about a waist fracture; (B) 10 days later, radiograph reveals more clearly the waist fracture. This search produced the following level I studies: a Cochrane meta‐analysis,1 one randomized controlled trial (RCT) comparing the suitability of two imaging techniques (conventional radiography vs a CT scan),2 two RCTs comparing the cost‐effectiveness of MRI versus conventional management,3,4 and two meta‐analyses of mostly prospective cohorts.5,6 Whenever possible, these level I studies will be used to answer the question. Studies with a lower level of evidence will be used to address the role of other imaging modalities that lack high‐quality evidence. The NPV of initial radiographs varies greatly between studies. One large prospective multicenter study of moderate quality showed a sensitivity of 93.7% (95% CI: 0.88–0.96) and a specificity of 100% (95% CI: 0.99–1.00) for patients with clinical suspicion and after five standardized projections.7 A collection of smaller studies shows a range of NPV between 50 and 93% with a mean of 82%.2,3,8–10 To compensate for this variation, patients with clinically suspected acute scaphoid fractures but negative initial x‐rays are typically treated with two weeks of cast immobilization followed by repeated examination and radiographic studies. A meta‐analysis by Yin et al. demonstrated that radiographs repeated in less than six weeks have a sensitivity of 91% (95% CI: 0.810–0.978) and a specificity of 99% (95% CI: 0.99–1.00).11 The latest Cochrane review reveals that bone scan is sensitive but not specific for diagnosing scaphoid fractures. Sensitivity and specificity of bone scan were 99% (95% CI: 0.69–1.00) and 86% (95% CI: 0.73–0.94).1 Moreover, it requires a delay of at least 72 hours following the injury to capture the osteoblastic activity of the fracture site5 and is also the most invasive test with the need for intravenous radioactive isotopes and a higher dose of radiation compared to CT scan.12 According to the latest Cochrane meta‐analysis, MRI has shown to have a sensitivity of 88% (95% CI: 0.64–0.97) and a specificity of 100% (95% CI: 0.38–1.00) (Figure 89.3).1 Previous meta‐analyses coincide with this high specificity value but grant higher values for sensitivity; 96% (95% CI: 0.91–0.99) and 97% (95% CI: 0.95–0.99).5,11 This decrease in sensitivity value observed in the latest Cochrane meta‐analysis is due to the selection of only high‐ and moderate‐quality studies for this calculation which omitted poor‐quality studies. Figure 89.3 Coronal Fat Sat T2 MRI confirming a suspected proximal pole fracture of the scaphoid. MRI also allows for the ability to detect associated soft tissue injuries. CT scan can also identify occult fractures (Figure 89.4) but is more useful in defining the fracture pattern and the angular deformity.13 According to the Cochrane review it has a sensitivity and specificity of 72% (95% CI: 0.36–0.92) and 99% (95% CI: 0.71–1.00), respectively. Similarly to the MRI findings, sensitivity is lower than the one from an earlier meta‐analysis which granted it a sensitivity between 93% (95% CI: 0.83–0.98) and 85% (95% CI: 0.73–0.94).5,11 This reduction in sensitivity is due to the same reasons as the MRI decrease. Figure 89.4 CT scan of the same patient in Figure 89.1
89
Carpal Fractures
Clinical scenario
Top three questions
Question 1: In patients with a suspected scaphoid fracture but negative findings on initial x‐rays, is magnetic resonance imaging (MRI) more sensitive and cost‐effective than temporary immobilization and repeated x‐rays after two weeks?
Rationale
Clinical comment
Available literature and quality of the evidence
Findings
Sensitivity and negative predictive value (NPV) of initial and repeated radiographs
Other diagnostic modalities and their utility in avoiding significant, unnecessary immobilization time
Bone scan
Magnetic resonance imaging
Computed tomography

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





