Cardiac considerations in the older patient
Meryl Cohen
Introduction
Determination of health and wellness among young individuals is relative, varying from person to person. Similarly, the effects of an aging cardiovascular system vary among the elderly. Controversies exist in the literature regarding the application of a single model to the influence of aging on heart function. Structural changes that occur with aging are more consistent and more easily identifiable than are physiological changes. The latter findings are difficult to distinguish for several reasons, including the interrelatedness of dynamic variables contributing to myocardial performance, the pathophysiology and symptomatology of heart disease, and the concept of hypokinesis in American society, to which the older person is, to an extent, considered to be entitled (Lakatta, 1993; Susic, 1997). In addition, comparison of studies is limited because of measurement inconsistencies and varying definitions of ‘elderly’ and ‘heart disease’. Many of the pioneering studies of the 1950s and 1960s continue to be reproduced using new definitions of ‘old’ and paying more deliberate attention to the presence of heart disease in study populations. Recent studies have been more effective at teasing out consequences of aging that are independent of disease, fitness and environment (Kaye & Esler, 2008).
There is general consensus regarding the effects of aging on several factors that influence cardiac performance. These factors have been studied in older individuals who are healthy and in those with heart disease, both at rest and during various levels of exertion. This chapter presents these findings as a model of declining cardiac performance with increasing age. Comparison is made to the baseline ‘young’ model in an attempt at defining a ‘healthy older’ model. The unique influences of exercise and disease on this model are then discussed, with an emphasis on the clinical implications of these physiological changes.
Cardiovascular structure
Age-related changes in cardiovascular tissue can be found in cardiac contractile fibers, conducting tissue and valvular structure (Lakatta & Levy, 2003a). Although the actual number of myocytes decreases, the myocyte volume per nucleus increases in both ventricles. Commonly, the coronary microvasculature is unable to accommodate this increase in tissue volume, which raises the likelihood of myocardial ischemia. In addition there is an increase in nondistensible fibrous tissue and an accumulation of senile amyloid deposits (see Box. 6.1). The loss of pacemaker cells (sinoatrial node tissue) and the increase in fibrous tissue in conducting pathways combine to increase the risk of cardiac arrhythmias in the elderly.
Simultaneous age-related changes occur in coronary arteries and systemic vasculature. These changes tend to increase the stiffness of the vessel walls (see Table 6.1; Fig. 6.1) (Priebe, 2000). Typically, proximal portions of the arteries change first, and the left coronary artery changes before the right. Together, the locations of the changes and the increased vessel rigidity cause an increase in peripheral vascular resistance. The heart attempts to adapt to this increased afterload (see discussion below) with myocellular hypertrophy, which probably accounts for the increase in myocyte volume previously mentioned. Alterations found in endothelial cells lining the arterial lumen cause a decrease in laminar blood flow, possibly establishing sites for lipid deposition and further increase cardiac afterload. In addition, decreased nitric oxide release from the coronary endothelium further reduces vasodilator capacity in the older individual (Susic, 1997; Lakatta & Levy, 2003b).
Table 6.1
Age-related cardiovascular responses to exercise
| Response | Effects of Aging | After Exercise Training |
| Resting | ||
| Oxygen consumption | ↔ | ↔ |
| Heart rate | ↔ | ↔ |
| Stroke volume | ↔ | ↔ |
| Arteriovenous oxygen difference | ↑ | ? |
| Submaximal exercise | ||
| Oxygen consumption | ↔ | |
| Heart rate | ↔ | ↓ |
| Stroke volume | ↔ | ? |
| Arteriovenous oxygen difference | ↑ | ? |
| Maximal exercise | ||
| Oxygen consumption | ↓ | ↑ |
| Heart rate | ↓ | ↔ |
| Stroke volume | ↓ or ↑ | ↑ |
| Arteriovenous oxygen difference | ↓ or ↔ | ↑ or ↔ |
| Cardiac output | ↔ (?) or ↑ | ↔ |
↑=increased; ↓=decreased; ↔=no change; ?=insufficient data on elderly subjects.
Reprinted from Protas E 1993 Physiological change and adaptation to exercise in the older adult. In: Guccione A (ed) Foundation of Geriatric Physical Therapy, 2nd edn. Mosby-Year Book St Louis, MO, with permission from Elsevier.
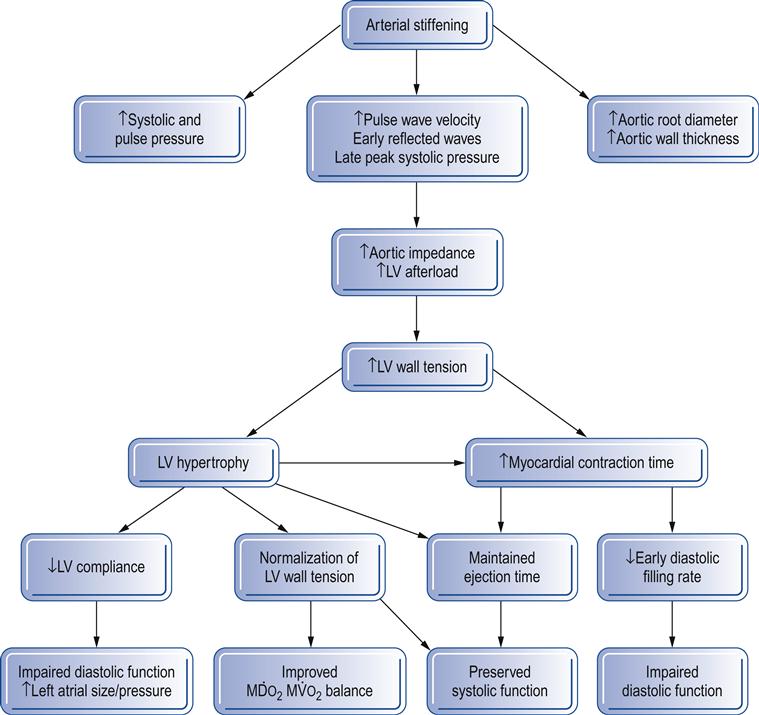
 , myocardial oxygen supply;
, myocardial oxygen supply;  , myocardial oxygen demand. (Reproduced with permission from Priebe, 2000. © The Board of Management and Trustees of the British Journal of Anaesthesia. Reproduced by permission of Oxford University Press/British Journal of Anaesthesia.)
, myocardial oxygen demand. (Reproduced with permission from Priebe, 2000. © The Board of Management and Trustees of the British Journal of Anaesthesia. Reproduced by permission of Oxford University Press/British Journal of Anaesthesia.)Recent advances in genetic and stem cell research have provided further insight into aging cardiac mitochondria and chromosome structure. Cardiac function, which relies heavily on ATP-generating properties of mitochondria, is negatively affected by the significant decline in mitochondria biogenesis and function seen with normal aging (Moslehi et al., 2012).
Cardiovascular physiology
The job of the heart is to pump blood rich with oxygen to body tissues. The ability of the heart to do this work efficiently is closely affected by three other systems: the lungs, the vasculature and the blood. Age- or disease-related changes occurring in these systems will directly affect cardiac function.
Cardiac output (CO), or the volume of blood pumped to body tissues each minute, depends on the frequency of cardiac contractions (heart rate) and the volume of blood ejected with each contraction (stroke volume). Heart rate (HR) can be influenced by many external factors; however, intrinsically, the HR depends on pacemaker tissue function and autonomic nervous system stimulation. In addition to the loss of pacemaker cells in older people, there is also a decreased sensitivity to beta-adrenergic stimulation (see Box 6.2). These two age-associated changes in HR control may or may not affect the resting HR, but they do typically decrease the maximal exercise HR (Fleg et al., 1994). CO is maintained in the older individual if the stroke volume (SV) is able to increase and compensate for any blunted HR response. This is the case if the individual remains physically fit, but usually the resting and submaximum CO tend to decrease with aging owing to a decrease in SV. This reduction in SV may be a result of alterations in a number of variables (see Box 6.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







