Cardiac arrhythmias and conduction disturbances
Pamela Reynolds
Introduction
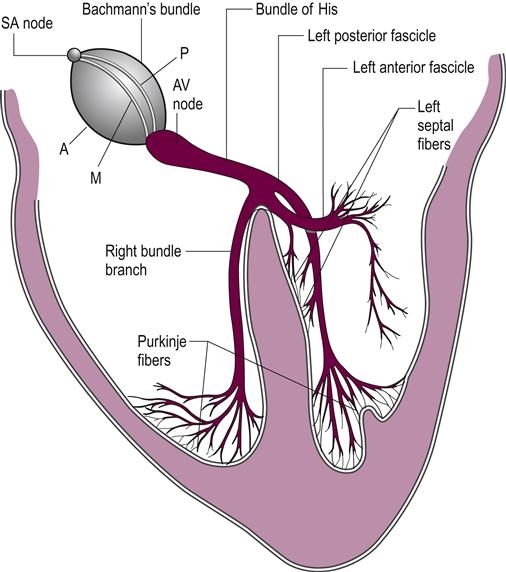
Cardiac rhythm originates from and is controlled by specific areas within the heart itself. These areas are called intrinsic pacemakers and are responsible for the propagation of electrical impulses that generally travel from the right atrium to the apex of the heart, and activate both atria and ventricles in the process. Although these impulses can pass from cardiac muscle cell to adjacent cardiac muscle cell, there is a preferential tract that they follow along specialized conducting tissue situated within the myocardium that minimizes conduction time. This pathway is detailed in Figure 41.1.
The primary intrinsic pacemaker is the sinoatrial (SA) node, situated at the junction of the superior vena cava and the right atrium. Electrical impulses travel from the SA node through the atria to the atrioventricular (AV) node, which sits on the right side of the interatrial septum. The rate of SA node discharge is controlled by the autonomic nervous system. Sympathetic stimulation increases the firing rate whereas parasympathetic activity (vagal stimulation) lowers the rate (Weiderhold, 1988; Mammen et al., 2004; Hillegass, 2011).
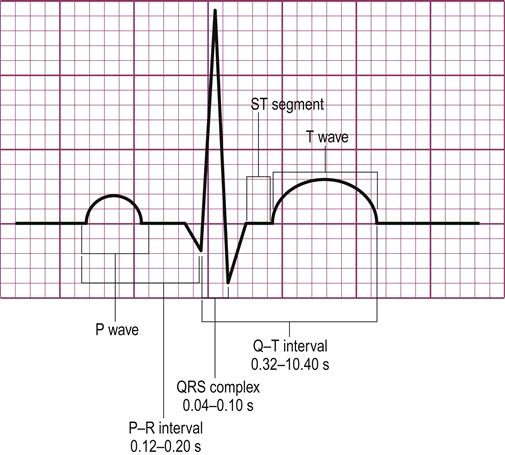
The depolarization of the atria corresponds to the P wave on the electrocardiogram (ECG). The impulse conduction is slowed as it traverses the AV node, allowing time for atrial contraction to be completed before ventricular contraction. This slowing or delay corresponds to the P–R interval on the ECG. After passing through the AV node, the impulse passes into the bundle of His, down the interventricular septum and then divides into the right and left bundle branches that supply impulses to the right and left ventricles respectively. The ventricular depolarization corresponds to the QRS complex on the ECG. The ST segment and T wave on the ECG are produced by ventricular repolarization. Specifically, the ST segment is the absolute refractory period in which no depolarization of the ventricles can occur. T-wave repolarization is also known as the relative refractory period. During this time, the ventricles can be stimulated to contract but the heart is still electrically unstable, and depolarization in this period can progress to ventricular tachycardia (Weiderhold, 1988).
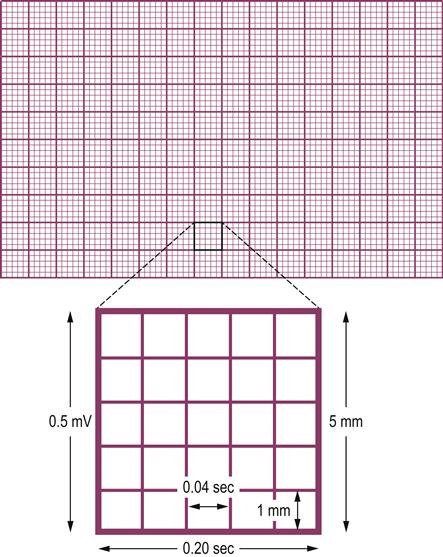
Each wave, segment and interval has certain normal characteristics, which are identified in Figure 41.2. Variances are usually indicative of different heart impairments. For instance, changes in the ST segment and T wave classically demonstrate some type of myocardial ischemia. Depression of the ST segment by more than 0.1 mm is generally indicative of ischemia and may also produce symptoms of angina. T-wave inversion is usually a sign of ischemia and/or an evolving myocardial infarction. Other abnormalities are discussed in the text that follows.
Many areas of the heart can depolarize spontaneously and rhythmically. The rate of ventricular contraction will be controlled by the area with the highest frequency of discharge. The SA node normally has the highest rate and therefore the ventricles will follow the rate set by the SA node. The normal cardiac cycle is termed normal sinus rhythm because it originates in the SA node and is conducted along the normal electrical pathway of the heart (Malone, 2006; Hillegass, 2011). Disturbances to cardiac rhythm and conduction are classified in several ways, for example: (i) heart rate; (ii) site of origin for the delay or block; (iii) whether rhythm is regular or irregular; (iv) mechanism of the arrhythmia; and (v) the ratio of atrial to ventricular depolarization (P waves–QRS complexes).
Basic rhythm disturbances and implications
Abnormal cardiac rhythms can arise in the atrial muscle, the junctional region between the atria and ventricles or in the ventricular muscle. These arrhythmias may be slow and sustained (bradycardias), occur as early single beats (extrasystoles or ectopic beats) or be sustained and fast (tachycardias). Rhythm disturbances may decrease cardiac output and potentially lead to orthostatic hypotension and possibly heart failure. If the ventricular rate is too fast, the volume of blood pumped with each contraction decreases. When the heart beats too slowly, the contractions are not adequate to supply the body’s demands. In the normal adult, heart rates between 40 and 160 beats per minute (bpm) are usually well tolerated, as physiological adaptations are able to maintain an adequate cardiac output and blood pressure. However, problems can arise in those with significant vascular disease if the heart rate drops below 50 bpm or goes above 120 bpm. These alterations to rate can cause tissue ischemia, with the heart being especially susceptible.
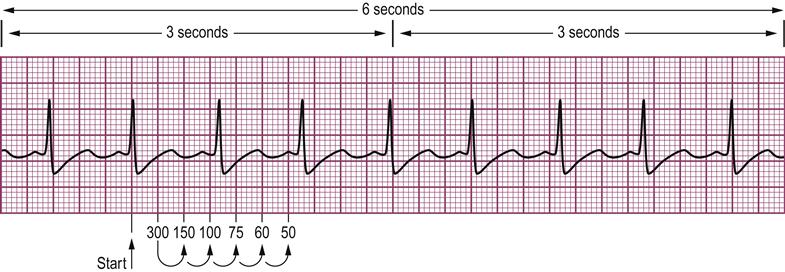
Heart rate can be determined from an ECG through several methods. The gridlines on the ECG paper indicate time on the horizontal axis and electrical voltage on the vertical axis. The paper is set up in millimeters. One millimeter on the horizontal axis equals 0.04 seconds and 0.1 mV on the vertical axis. Heavier dark lines section the ECG paper into 5 mm by 5 mm larger boxes representing 0.2 seconds horizontally and 0.5 mV vertically (Weiderhold, 1988; Hillegass, 2011) (Fig. 41.3). Heart rate can be calculated by counting the number of R waves in a 6-second strip and multiplying by 10. Another way to estimate the heart is to memorize these triplicates: ‘300, 150, 100’ and ‘75, 60, 50’. Then find an R wave that falls on one of the heavy black lines, count the number of large boxes to the next R wave, counting off heavy black lines with the triplicates between the two R waves (Weiderhold, 1988; Watchie, 2010; Hillegass, 2011) (Fig. 41.4).
Different areas of the heart are able to initiate the depolarization sequence if the SA node fails or, if conduction is blocked, another area will fire a depolarizing impulse and keep the heart beating. These secondary sites have lower depolarization frequencies than the SA node to avoid competition between pacing sites. As the heart is controlled by whichever site is discharging most frequently, the SA node with a rate of about 70 bpm is the primary site of impulse initiation. If the SA node fails, control will be assumed by a focus either in the atrial muscle or around the AV node (junctional region). Both of these have spontaneous depolarization frequencies of 40–60 bpm. If these fail, or conduction through the bundle of His is blocked, a ventricular focus will take over, with a rate of about 30–40 bpm (Weiderhold, 1988; Mammen et al., 2004). Therefore, the major mechanisms that cause bradyarrhythmias are either depression of SA node activity or blocks within the conducting system. In either situation, a supplementary pacemaker takes over to control the heart rate. If these supplementary pacemaker cells are located above the bifurcation of the bundle of His, the rate will be adequate enough to maintain cardiac output. Any bradyarrhythmia that causes hemodynamic compromise of the heart muscle requires urgent medical intervention.
Junctional impulses can arise from the AV node or above the bifurcation of the bundle of His. The impulse then spreads retrogradely or backwards through the atria and antegradely towards the ventricles. Depending on the site of origin and the conduction velocity of the impulse, and the refractory periods of the atria and ventricles, activation of the atria may occur before, during or after depolarization of the ventricle.
Any part of the heart can depolarize earlier than it should and, if it initiates a heartbeat, this is called an extrasystole or ectopic beat. Atrial ectopic beats cause abnormally shaped P waves on the ECG, whereas junctional ectopic beats may have no P wave or a P wave immediately before or after the QRS complex, depending on the site of the ectopic focus within the junctional region. The QRS complexes for atrial and junctional ectopic beats have the same configuration as in normal SA rhythm. Ectopic beats arising in the ventricles do not travel down the normal bundle branches. Therefore, they evoke abnormally shaped QRS complexes, frequently referred to as wide and bizarre, which are easily recognized on an ECG tracing.
Tachycardia refers to a clinical state in which the heart rate is over 100 bpm. Regardless of whether an ectopic focus is within the atria, the junctional (AV nodal) region or the ventricles, it can fire rapidly and repeatedly causing a sustained tachycardia. Bradycardia refers to a heart rate that is less than 60 bpm. Urgent treatment is needed if there is hemodynamic compromise of the cardiac muscle or rhythms develop that have the potential to become life-threatening (Malone, 2006; Collins & Dias, 2009; Watchie, 2010; Hillegass, 2011).
The following discussion of the most common types of rhythm disturbance will be categorized according to the anatomical site of the disturbance: supraventricular (atrial), junctional or ventricular. Each will then be divided into the type of arrhythmia: slow, fast or ectopic. Conduction blocks are discussed separately as a cause of bradycardia.
Atrial arrhythmias
Sinus arrhythmia
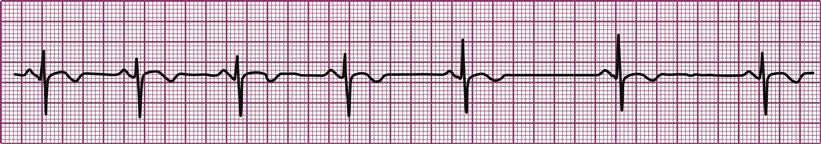
In sinus arrhythmia, the vagal nerves and changes in respiration can alter the rate of SA node discharge. The ECG is normal except for the variable lengths of the R–R intervals (Fig. 41.5). Variations are common, especially with changes in the rate of respiration. This rhythm is very prevalent in young people and tends to decline with aging. No treatment is required (Weiderhold, 1988; Mammen et al., 2004; Watchie, 2010; Hillegass, 2011).
Sinus bradycardia
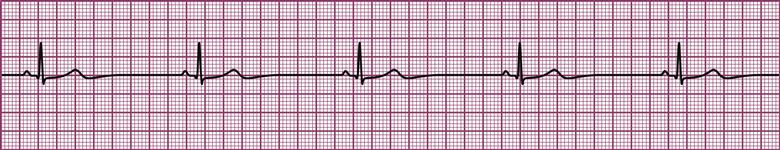
Sinus bradycardia is a regular sinus rhythm but with a SA node rate below 60 bpm (Fig. 41.6). The ECG has normal P waves and P–R intervals and a 1:1 conduction ratio between the atria and ventricles, but an atrial rate of less than 60 bpm. It represents a suppression of the SA node discharge rate, usually in response to normal physiology in athletes, during sleep and with stimulation of the vagus nerve. It may be drug-related, especially from the use of narcotics, beta blockers and calcium-channel blockers. Pathologies that may produce a bradycardia rhythm include acute myocardial infarction, increased intracranial pressure, hypersensitivity of the carotid sinus and hypothyroidism. If evidence of hemodynamic compromise is present, then treatment is needed. Drug treatment can be useful in the short term; however, in those with symptomatic recurrent or persistent bradycardia, internal cardiac pacing is indicated (Weiderhold, 1988; Mammen et al., 2004; Watchie, 2010; Hillegass, 2011).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree