Capsulodesis for Treatment of Scapholunate Instability
Angel Ferreres
Marc García-Elías
Andrew Chin
DEFINITION
Scapholunate dissociation (SLD) is the rupture of the anatomic linkage between the scaphoid and lunate and its subsequent progressive dysfunction, with or without carpal malalignment.
Classical radiographic signs occur only when there is permanent carpal malalignment. This is preceded by complete scapholunate disruption together with failure of the secondary scaphoid stabilizers, namely the scaphotrapeziotrapezoid (STT) ligament, the scaphocapitate (SC) ligament, and the radioscaphocapitate (RSC) ligament.
However, in many cases, only partial tears or ligament sprains occur and do not produce positive radiologic signs. These injuries are often seen only arthroscopically.
Dorsal capsulodesis of the radioscaphoid joint was first described by Blatt.2 Now it is one of the most commonly used techniques in the treatment of carpal instability. This procedure involves the creation of a dorsal capsular flap.
ANATOMY
Scapholunate ligaments are divided into three fibrous structures:
Dorsal ligament
Volar ligament
Thin proximal membrane
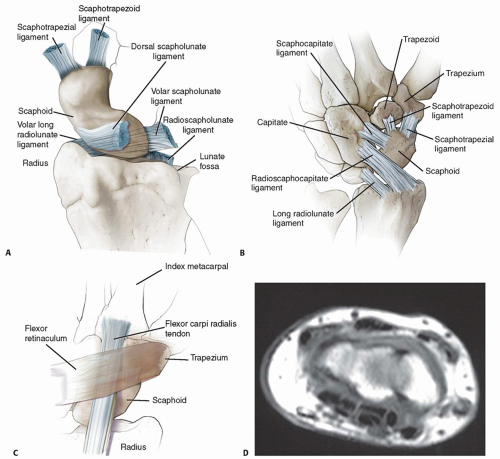
Anatomically, the dorsal scapholunate ligament is the thickest and shortest of the fibrous structures, measuring 2 to 3 mm thick and 2 to 5 mm long. Biomechanically, it is the strongest and most resistant to failure under load.1 The radioscapholunate (Testut) ligament is only a path for vascularization and innervation of the scaphoid and lunate (FIG 1A).
Scaphoid position and relationship with lunate and distal carpal row is maintained by the scapholunate ligaments and by the secondary stabilizers (STT, SC, and RSC ligaments), which prevent excessive scaphoid flexion. These are collectively the secondary stabilizers (FIG 1B).
The flexor carpi radialis (FCR) tendon is closely related to the STT joint and acts as a crucial dynamic stabilizer of the scaphoid, preventing it from rotating into excessive flexion and pronation during grip (FIG 1C).
PATHOGENESIS
Injury to the scapholunate ligaments occurs when the wrist is hyperextended, ulnarly deviated, and supinated during a fall on an outstretched hand. Because of the osseous configuration and disposition of the bones of the proximal carpal row, when the hand hits the floor, the tubercle of the scaphoid is pushed dorsally and extended. The lunate is held in position by the volar radiolunate (RL) ligaments and resists the tendency to extension transmitted by the scaphoid. The impact of the hand on the floor also pushes the pisiform against the triquetrum and because of the configuration of the joint between the triquetrum and the hamate, the former turns into flexion. If forces exceed the ligaments’ resistance, they will rupture.
The sequence of failure of the ligaments is from palmar to dorsal. The first to tear is the volar scapholunate ligament, the weaker of the two scapholunate ligaments, followed by the dorsal scapholunate ligament.5
The participation of the dorsal intercarpal ligament (DICL) in scapholunate instability has been recently supported by the studies of Mitsuyasu et al.13
NATURAL HISTORY
Most SLDs present as the initial stage of a progressive carpal destabilization. The mechanism of injury produces a spectrum of injuries, ranging from mild scapholunate sprains to complete perilunar dislocations, all being different stages of the same progressive perilunar destabilization process as described by Mayfield et al.11
If only the palmar scapholunate ligament and the proximal membrane are disrupted, minor kinematic alterations result in predynamic instability. There is no gross carpal malalignment, but because there is an increased motion between the scaphoid and lunate causing shear stress, these injuries may be sufficient to promote painful synovial inflammation.
Complete disruption of the scapholunate ligament complex leads to substantial alteration in kinematic and force transmission parameters (demonstrated in cadaver specimens) but not necessarily static carpal malalignment.13,17 Dynamic instability may be the result. The scaphoid is unconstrained at the proximal end, resulting in increased RL motion and correspondingly decreased radioscaphoid motion. This is accentuated in a loaded wrist.
When the secondary stabilizers start to attenuate after repeated use of the wrist, carpal malalignment develops, eventually resulting in static instability. Initially, the scaphoid is still reducible, but over time, it becomes permanently flexed and pronated (see Imaging and Other Diagnostic Studies).
If the alteration in the motion of the scaphoid persists, the cartilage degenerates and arthrosis develops. This pattern of degeneration is known as scapholunate advanced collapse (SLAC).
Once arthrosis is present, surgical techniques directed at replacing or reconstructing the injured ligaments are no longer options.
SLD is a progressive entity. Therefore, reconstruction is advocated as soon as it is diagnosed.
PATIENT HISTORY AND PHYSICAL FINDINGS
Almost always, patients present after a fall on their outstretched hand. The patient complains of dorsal hand and wrist pain when loading the affected wrist, such as when standing up from a chair.
Predynamic and dynamic stages of SLD are often missed or overlooked. The injury usually is the result of isolated trauma, which the patient does not clearly remember, or is masked by other more severe or obvious injuries (eg, fractured scaphoid and distal radius). A high index of suspicion is required.
Weakness of grip strength, occasional swelling over the dorsoradial wrist, point tenderness over the scapholunate interval (more pronounced with gripping), and radial-sided wrist pain after excessive or heavy use are common but subtle physical examination findings.
The examiner should palpate the scapholunate interval dorsally (1 cm distal to the tubercle of Lister) with the wrist in 30 to 50 degrees of flexion.
On palpation of the anatomic snuffbox and palmar scaphoid tubercle, tenderness may also be present, suggesting ligament involvement, synovitis, or an occult ganglion.
Provocative tests such as the Watson scaphoid shift test and resisted finger extension test reinforce the possibility of the diagnosis.
Watson scaphoid shift test: The scaphoid flexes as the wrist goes from ulnar to radial deviation. The examiner’s thumb prevents the scaphoid from flexing and if the scapholunate ligament is torn or incompetent, the proximal pole subluxates dorsally out of the scaphoid fossa, causing pain. When the thumb pressure is released, there may be a snap, signifying
spontaneous reduction of the scaphoid back into the scaphoid fossa. This test is not highly specific and may signify synovitis, an occult ganglia, or radioscaphoid impingement.
Sharp pain on the resisted finger extension test has low specificity but high sensitivity.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographs
Posteroanterior (PA) view
Elbow flexed at 90 degrees, neutral pronosupination, and the middle finger aligned with the forearm axis. The palm of the hand is in full contact on the film case.
Scapholunate gap greater than 3 mm or wider than the contralateral normal side and a cortical “ring” sign suggest SLD.
Decreased space between the radius and the scaphoid signifies cartilage loss and arthrosis.
Anteroposterior (AP) view
Forearm is in maximal supination.
This projection puts the scapholunate interval aligned with the beam of the ray.
Lateral view
Elbow at 90 degrees of flexion, middle finger aligned with the forearm, and wrist at 0 degree of extension or flexion
This projection allows measurement of the scapholunate angle. An angle greater than 60 degrees indicates disruption of the scapholunate ligaments and often corresponds with widening on the PA and AP views.
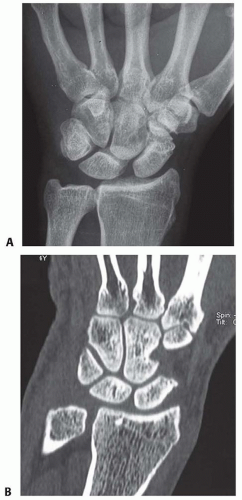
Clenched fist AP view demonstrates a widened scapholunate gap compared to the normal side (FIG 2A).
Cineradiography reveals abnormal movements between the scaphoid and lunate and an increase in the scapholunate gap as the wrist moves from radial to ulnar deviation.
Arthrography is not specific and may be positive in conditions such as degenerative perforations of the scapholunate membrane and osteochondral defects.
Magnetic resonance imaging (MRI) does not provide much additional information. Minor, degenerative perforation of the scapholunate membrane may result in a positive test.
Scapholunate ligaments can be seen clearly only on transverse cuts that pass through the two horns of the lunate (see FIG 1D).
MRI plays an important role in excluding other differential diagnoses.
Computed tomography scans do not give additional information except for providing a more accurate measurement of the parameters involved in the diagnosis of static SLD (eg, scapholunate distance and angle; FIG 2B).
It is useful in looking for other osseous anomalies of the wrist (eg, impacted fracture of the radius, scaphoid fracture).
Arthroscopy is the gold standard for diagnosing and staging SLD. It allows grading of the instability (Geissler classification) and therefore determination of the degree of injury to the ligament complex.5
It is also useful in assessing the condition of the cartilage and in locating concomitant carpal injuries that might negatively affect the outcome of a capsulodesis (Table 1).
DIFFERENTIAL DIAGNOSIS
Occult ganglia
Synovitis
Scaphoid fracture, nonunion, and avascular necrosis
Radiocarpal arthrosis
Radioscaphoid impingement
Table 1 Arthroscopic (Geissler) Grading of Interosseous Ligament Tears | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
NONOPERATIVE MANAGEMENT
Initial conservative management aims at resting the injured limb and decreasing edema. Adequate immobilization with casting or splinting is advocated.
This immobilization is frequently therapeutic for patients with predynamic SLD.
Elevation of the limb and active finger motion minimize edema.
Anti-inflammatory medications can be given for pain relief.
Physiotherapy may have a role if Geissler grade 1 instability is diagnosed by arthroscopy. As the ligaments have not lost their integrity, a period of short immobilization (2 weeks), followed by proprioception reeducation of the FCR, as dynamic stabilizer of the scaphoid, is suggested.
Nonoperative treatment is seldom indicated when a significant disruption is diagnosed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree