Calcaneal Lengthening Osteotomy
Vincent S. Mosca
INDICATIONS/CONTRAINDICATIONS
Flexible flatfoot is the “contour of a strong and stable foot… of little consequence as a cause of disability,” according to Harris and Beath in their landmark study on foot ailments in Canadian soldiers that was published in 1947. By way of contrast, they found that flexible flatfoot with a short tendo Achillis was often the cause of pain and disability.
The calcaneal lengthening osteotomy is indicated:
To correct the valgus/eversion deformity of the hindfoot in a flexible flatfoot with a short tendo Achillis when prolonged attempts at nonoperative management fail to relieve the pain under the head of the plantarflexed talus and/or in the sinus tarsi area
To correct the valgus/eversion deformity of the hindfoot in a symptomatic skewfoot with short tendo Achillis when prolonged attempts at nonoperative management fail to relieve the pain under the head of the plantarflexed talus and/or in the sinus tarsi area.
Management of the forefoot deformity varies between a flatfoot and a skewfoot. This statement highlights the fact that the calcaneal lengthening osteotomy does not correct flatfoot or skew-foot deformity. It corrects all components of valgus/eversion deformity of the hindfoot. There is frequently/usually a separate deformity of the forefoot that requires an additional procedure during the same operative session. And the heel-cord contracture that created the pain in the first place must be surgically addressed concurrently.
The calcaneal lengthening osteotomy is NOT indicated:
To change the shape of a pain-free flexible flatfoot
Surgery should not be performed in young children with flexible flatfeet who have nonlocalized, activity-related aching foot pain or nighttime pain in the lower extremities.
For incongruous signs or symptoms
In such situations, the flatfoot may be an incidental finding and not the cause of the symptoms.
For valgus deformity of the hindfoot in the iatrogenic flatfoot created by overcorrection of a clubfoot in which the calcaneus is laterally translated under the talus, the talonavicular joint is well aligned, and the thigh-foot angle is in neutral alignment
PREOPERATIVE PLANNING
Physical examination includes evaluation of the foot in weight bearing and non-weight bearing. In weight bearing, the surgeon should note the hindfoot’s valgus alignment, the depression of the longitudinal arch, and the outward rotation of the foot in relation to the flexion/extension plane of the knee as referenced from the alignment with the patella (Fig. 25-1).
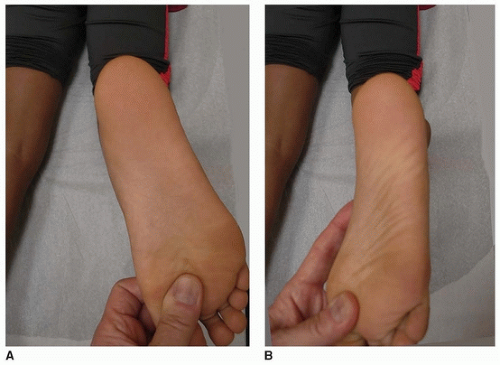
Flexibility of a flatfoot means flexibility of the subtalar joint. It is confirmed by observing the creation of the longitudinal arch and conversion of hindfoot valgus to varus with toe standing. Manipulation of
the subtalar joint is also performed with the child on the examination table. Inversion of the subtalar joint is a combination of plantar flexion (down), internal rotation (in), and supination of the calcaneus/acetabulum pedis under and around the talus. It is critical that the manipulation is performed with (1) the ankle joint in neutral dorsiflexion, (2) one hand cupping the calcaneus, (3) the other hand stabilizing and controlling the forefoot, and (4) the hand on the calcaneus acting as the motor that inverts (down and in) and everts (up and out) the calcaneus/acetabulum pedis/subtalar joint (Video 25-1).
the subtalar joint is also performed with the child on the examination table. Inversion of the subtalar joint is a combination of plantar flexion (down), internal rotation (in), and supination of the calcaneus/acetabulum pedis under and around the talus. It is critical that the manipulation is performed with (1) the ankle joint in neutral dorsiflexion, (2) one hand cupping the calcaneus, (3) the other hand stabilizing and controlling the forefoot, and (4) the hand on the calcaneus acting as the motor that inverts (down and in) and everts (up and out) the calcaneus/acetabulum pedis/subtalar joint (Video 25-1).
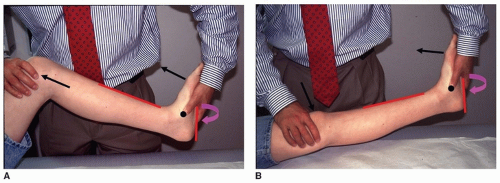
Video 25-1 Video showing the proper way to assess subtalar motion. See text. On the examining table, the Silfverskiöld test is performed to determine whether the equinus contracture is in the gastrocnemius alone or involves the entire triceps surae (Fig. 25-2, Video 25-2). The thigh-foot angle and the transmalleolar axis are assessed with the patient prone (Fig. 25-3). Most commonly, with eversion deformity of the hindfoot, the thigh-foot angle is abnormally positive (excessively turned out in relation to the thigh), whereas the transmalleolar axis (which specifically assesses tibial torsion) is normal. Further, the surgeon should determine whether the subtalar joint can be inverted to neutral. That said, the calcaneal lengthening osteotomy can correct rigid hindfoot valgus/eversion deformity even in a rigid deformity, as in a foot with a tarsal coalition, whether or not the coalition is resected.
Video 25-2 Video of the Silfverskiöld test. The subtalar joint is inverted to neutral with a thumb on the talonavicular joint to confirm that it is anatomically aligned or “locked.” With the TN joint
held anatomically aligned, the knee is flexed and extended while maintaining maximum dorsiflexion stress on the foot. True ankle dorsiflexion is then measured as the angle between the plantar-lateral border of the foot and the anterior tibial cortex. There are approximately 10 degrees of dorsiflexion with the knee flexed and 0 degrees with the knee extended. The subtalar joint is then allowed to evert to the normal resting valgus position of this flatfoot. The foot is again dorsiflexed with the knee both flexed and extended. There appears to be 30 degrees of dorsiflexion with the knee flexed and 20 degrees of dorsiflexion with the knee extended. That means that 20 degrees of this apparent ankle dorsiflexion is actually occurring in the subtalar joint as a component of eversion. One would anticipate the need for a gastrocnemius recession, and possibly an entire Achilles tendon lengthening, following correction of subtalar joint eversion with a calcaneal lengthening osteotomy.
held anatomically aligned, the knee is flexed and extended while maintaining maximum dorsiflexion stress on the foot. True ankle dorsiflexion is then measured as the angle between the plantar-lateral border of the foot and the anterior tibial cortex. There are approximately 10 degrees of dorsiflexion with the knee flexed and 0 degrees with the knee extended. The subtalar joint is then allowed to evert to the normal resting valgus position of this flatfoot. The foot is again dorsiflexed with the knee both flexed and extended. There appears to be 30 degrees of dorsiflexion with the knee flexed and 20 degrees of dorsiflexion with the knee extended. That means that 20 degrees of this apparent ankle dorsiflexion is actually occurring in the subtalar joint as a component of eversion. One would anticipate the need for a gastrocnemius recession, and possibly an entire Achilles tendon lengthening, following correction of subtalar joint eversion with a calcaneal lengthening osteotomy.
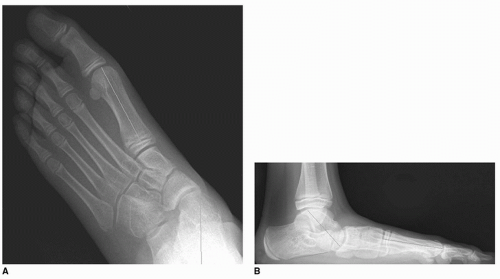
Radiographs must be taken with full weight bearing to correlate with the physical examination findings. Anteroposterior and lateral views are required (Fig. 25-4). Oblique and Harris axial views of the foot, or CT scan, can be added to assess the possible coexistence of a tarsal coalition. Anteroposterior, mortise, and lateral ankle radiographs are useful to determine whether any of the valgus deformity is in the tibiotalar joint.
The family should be informed of the risks and complications of allograft versus autograft for the required tricortical (bicortical) iliac crest bone graft. They should also be told of the possible need for a medial cuneiform, plantar-based closing wedge osteotomy. The need for this additional procedure can only be accurately determined intraoperatively following correction of the hindfoot deformity and lengthening of the heel cord.
Discussion about staged versus concurrent correction of bilateral deformities should include issues relating to the need for strict non-weight bearing on the operated foot/feet for 8 weeks. Most adolescents choose the correction of 1 foot at a time, with correction of the other foot 6 months later. This interval allows adequate rehabilitation for the operated foot to function comfortably in full weight bearing while non-weight bearing on the other foot.
SURGICAL PROCEDURE
Evans’ original report on the concept of lateral column lengthening was absolutely brilliant and correct. However, his description of the technique was terse, leading to treatment failure by most orthopedic surgeons who attempted to interpret his concept. What follows is my interpretation and
expansion on Evans’ concept that I originally reported in 1995 and reported in several subsequent publications since then. There are no shortcuts, and there should be no deviation from, or elimination of, steps. Attention to all of the details of the technique is critical for consistently good results. There are only two intraoperative decisions that need to be made: (a) whether rigid forefoot supination deformity exists and requires a medial cuneiform osteotomy for correction and (b) whether the heel-cord contracture is in the gastrocnemius alone or in the entire triceps surae.
expansion on Evans’ concept that I originally reported in 1995 and reported in several subsequent publications since then. There are no shortcuts, and there should be no deviation from, or elimination of, steps. Attention to all of the details of the technique is critical for consistently good results. There are only two intraoperative decisions that need to be made: (a) whether rigid forefoot supination deformity exists and requires a medial cuneiform osteotomy for correction and (b) whether the heel-cord contracture is in the gastrocnemius alone or in the entire triceps surae.
 FIGURE 25-5 Narrow Crego retractors (left), Joker elevators (center), and lamina spreader with smooth teeth (right). |
Special equipment includes a narrow sagittal saw, smooth Steinmann pins, straight osteotomes, a lamina spreader with smooth teeth, Joker elevators and narrow Crego retractors (Fig. 25-5), and a minifluoroscope:
The patient is placed supine with a folded towel under the ipsilateral buttock. A foam-cushioned ramp under the entire extremity can also be used. The lateral hindfoot must be visualized without difficulty.
If autograft is used, the patient is prepped and draped from the iliac crest to the toes, and a sterile tourniquet is used. If using allograft, only the lower extremity is prepped, and a nonsterile tourniquet is used.
A modified Ollier incision is made in a Langer skin line from the superficial peroneal nerve to the sural nerve (Fig. 25-6).
The soft tissues are elevated from the sinus tarsi, avoiding exposure of, or injury to, the capsule of the calcaneocuboid joint.
The peroneus longus and the peroneus brevis are released from their tendon sheaths on the lateral surface of the calcaneus (Fig. 25-7A). The intervening tendon sheaths are resected, as is the peroneal tubercle if it is large.
The peroneus brevis tendon is Z-lengthened. The peroneus longus tendon must not be lengthened. The aponeurosis of the abductor digiti minimi is divided at a point approximately 2 cm proximal to the calcaneocuboid joint (Fig. 25-7B).
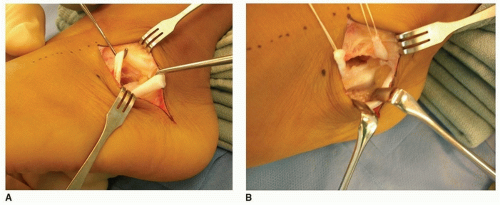
The interval between the anterior and middle facets of the subtalar joint is identified with a Freer elevator (Fig. 25-8). It is inserted into the sinus tarsi, perpendicular to the lateral cortex of the calcaneus at the level of the isthmus (Fig. 25-8A).
The isthmus is the lowest point of the dorsal-lateral cortex of the calcaneus in the sinus tarsi at the junction of the beak of the calcaneus and the posterior facet. It is the anatomic site that creates the radiographic “critical angle of Gissane.”

FIGURE 25-8 Finding the interval between the anterior and middle facets of the subtalar joint. A.Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree