Calcaneal Fractures/Talar Neck Fractures
Michael P. Clare
Roy W. Sanders
Fractures of the calcaneus and talus are among the most complex and challenging of fractures for the orthopaedic surgeon to effectively manage, in that both are three-dimensionally unique structures with highly specialized biomechanical function and a distinctly limited surrounding soft tissue envelope. Fractures of the calcaneus and talus are generally the result of high-energy trauma, such as a motor vehicle accident or a fall from a height, and as such, the severity of fracture displacement and the extent of soft tissue disruption are directly proportional to the amount of force and energy absorbed by the limb.
Fractures of the Calcaneus
Indications/Contraindications
General Considerations
Operative treatment is generally indicated for displaced intra-articular fractures involving the posterior facet as demonstrated on computed tomography (CT) scanning. Nonoperative treatment is best reserved for non- or minimally-displaced extra-articular calcaneal fractures, and truly non-displaced intra-articular fractures as determined on CT scan.
Comorbidities
While nicotine use/dependence is not a contraindication to operative treatment, all patients who are smokers are counseled at length as to the associated risks and encouraged to discontinue tobacco use. We consider heavy smoking (≥2 packs per day) as a relative contraindication to surgery. Specific contraindications for operative treatment include fractures in patients with insulin-dependent diabetes mellitus, severe peripheral vascular disease, or other major medical comorbidities precluding surgery, as well as fractures in elderly patients who are minimal (household) ambulators. Because many older patients are healthy and active well into their 70s, chronologic age itself is not necessarily a contraindication to surgical treatment.
Delayed Treatment by Necessity
Operative treatment may also be contraindicated if initial evaluation has been delayed beyond 3 or 4 weeks from the date of injury, or in certain situations in which injury severity prohibits early surgical intervention, including fractures associated with severe fracture blisters or prolonged edema; fractures with large open wounds; and fractures in patients with life-threatening injuries. Operative treatment following a prolonged delay (>4 weeks) from initial injury to definitive treatment is complicated by the fact that early consolidation of the fracture has occurred, making the fracture fragments increasingly difficult to separate to obtain an adequate reduction, and the articular cartilage may delaminate away from the underlying subchondral bone. In these instances, delayed treatment by necessity is used whereby the fracture is allowed to heal and is later managed as a calcaneal malunion following resolution of the prohibitive factors.
Preoperative Planning
In completing preparations for surgery, the surgeon should thoroughly review the plain radiographs and CT scans to gain a preliminary understanding as to the “personality” of the fracture pattern, which then allows for planning of patient position and surgical approach, as well as anticipation of specific technical steps in obtaining fracture reduction, and the necessary implants for definitive stabilization. While multiple surgical approaches have historically been described, the general consensus currently favors the extensile lateral approach for most displaced intra-articular calcaneal fractures. Percutaneous reduction techniques, such as the Essex-Lopresti maneuver, are particularly ideal for certain tongue-type fracture (Sanders type II-C) patterns.
Surgery is ideally completed within the first 3 weeks of injury before early fracture consolidation; however, surgery should not be attempted until the associated soft tissue swelling has sufficiently dissipated as demonstrated by a positive wrinkle test. The test involves assessment of the lateral calcaneal skin with passive dorsiflexion and eversion of the injured foot. A positive test is confirmed by the presence of skin wrinkling without residual pitting edema, such that surgical intervention may be safely undertaken (Fig. 33-1). A variety of modalities may used to decrease swelling in the affected extremity. We prefer initial elevation and immobilization in a bulky Jones dressing and supportive splint, with later conversion to an elastic compression stocking and fracture boot locked in neutral flexion as the acute swelling begins to dissipate in the ensuing few days.
Extensile Lateral Approach
Surgery
Patient Positioning/General Considerations
The procedure requires use of a radiolucent table and a standard C-arm. For isolated injuries, we prefer placing the patient in the lateral decubitus position on a beanbag. The lower extremities are positioned in a scissor configuration, whereby the operative (“up”) limb is flexed at the knee and angles toward the posterior, distal corner of the operating table, and the nonoperative (“down”) limb is extended at the knee and positioned away from the surgical field to facilitate intraoperative fluoroscopy. Protective padding is placed beneath the contralateral limb for protection of the peroneal nerve, and an operating “platform” is created with blankets and foam padding to elevate the operative limb (Fig. 33-2). The prone position may alternatively be used in the event of bilateral injuries.
The patient is given prophylactic preoperative antibiotics, and a pneumatic thigh tourniquet is used. The procedure should be completed within 120 to 130 minutes of tourniquet time, so as to minimize wound complications. If the procedure extends beyond that time, the tourniquet should be released and the remainder of the procedure performed without it. In allocating tourniquet time, the surgical approach should be completed within 20 minutes, allowing up to 60 minutes for fracture reduction, 20 minutes for implant placement, and 20 minutes for wound closure.
Technique
Anatomic Landmarks
Wound complications following surgical management of calcaneal fractures remain a major source of morbidity with these injuries. The soft tissues overlying the lateral hindfoot receive blood supply from a confluence of three arterial branches: the lateral calcaneal artery, the lateral malleolar artery, and the lateral tarsal artery. Borrelli and Lashgari determined that the majority of the full-thickness flap with an extensile lateral approach is supplied by the lateral calcaneal artery, typically a branch of the peroneal artery. At the level of lateral malleolus, the artery courses parallel to the Achilles tendon and lies approximately 11 to 15 mm anterior to the terminal Achilles tendon and its insertion. Thus, strict attention to detail with respect to placement of the incision and gentle handling of the soft tissues is of paramount importance.
Incision and Surgical Approach
The extensile lateral incision is then outlined on the skin with a marking pencil (Fig. 33-3). The incision begins approximately 2 cm proximal to the tip of the lateral malleolus, just lateral to the Achilles tendon extending toward the plantar foot. In this manner, the vertical limb of the incision will course posterior to the sural nerve and the lateral calcaneal
artery, thereby avoiding devascularization of the lateral calcaneal flap. The horizontal limb of the incision is drawn along the junction of the skin of the lateral foot and heel pad, the demarcation of which can be identified by compressing the heel. We prefer to substitute a gentle curve where these two lines intersect to form a right angle, primarily to avoid necrosis of the apical skin. The terminal portion of the horizontal limb includes a gentle curve anteriorly along the skin creases, extending over the calcaneocuboid articulation.
artery, thereby avoiding devascularization of the lateral calcaneal flap. The horizontal limb of the incision is drawn along the junction of the skin of the lateral foot and heel pad, the demarcation of which can be identified by compressing the heel. We prefer to substitute a gentle curve where these two lines intersect to form a right angle, primarily to avoid necrosis of the apical skin. The terminal portion of the horizontal limb includes a gentle curve anteriorly along the skin creases, extending over the calcaneocuboid articulation.
With a sterile bolster placed beneath the medial ankle, the incision begins at the proximal portion of the vertical limb, becoming full-thickness at the level of the calcaneal tuberosity; dissection is specifically taken from “skin to bone” at this level while avoiding any beveling of the skin. Scalpel pressure is again lessened beyond the apical curve, roughly at the midpoint of the horizontal limb, at which point a layered incision is again developed.
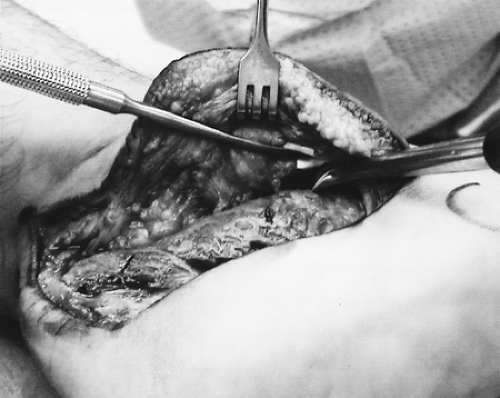
A full-thickness subperiosteal flap is then developed starting at the apex. Any use of retractors should be avoided until a sizeable flap has been raised, so as to avoid separation of the skin from the subcutaneous tissues and periosteum. The calcaneofibular ligament and inferior peroneal retinaculum are released sharply, thus exposing the peroneal tendons. Both tendons are identified and released from the peroneal tubercle through the cartilaginous pulley, and further gently mobilized distally with a periosteal elevator, thereby exposing the anterolateral calcaneus and calcaneocuboid joint. In this manner, the peroneal tendons and sural nerve are contained entirely within the sub-periosteal flap (Fig. 33-4).
Deep dissection continues anteriorly to the sinus tarsi and anterior process, and posteriorly to the superior-most portion of the calcaneal tuberosity for “window visualization” of the posterior facet, so as to prevent rotational malalignment of the posterior facet articular surface in the sagittal plane. Three 1.6-mm Kirschner wires are then placed for retraction of the subperiosteal flap using the “no touch” technique. In this technique, one wire is placed into the distal fibula as the peroneal tendons are slightly subluxed anteriorly; a second wire is placed in the talar neck; a third wire is placed in the cuboid as the peroneal tendons are levered away from the anterolateral surface of the calcaneus with a periosteal elevator. Thus, each Kirschner wire retracts its respective portion of the peroneal tendons and subperiosteal flap (Fig. 33-5). A small Bennett-type retractor may additionally be used at the distal margin of the sinus tarsi for further exposure of the anterolateral calcaneus.
Assessment of the Peroneal Tendons
Following fracture reduction, definitive stabilization, and final fluoroscopic images, the wound is copiously irrigated. As the previously placed Kirschner wires are manually removed, the peroneal tendons should easily reduce into the peroneal groove at the posterior border of the lateral malleolus. A Freer elevator is introduced into the tendon sheath, advanced proximally to the level of the lateral malleolus, and levered anteriorly to assess the stability of the peroneal tendon sheath and superior peroneal retinaculum. If the tendon sheath is detached from the lateral malleolus and therefore incompetent, the elevator will easily advance anterior to the lateral malleolus, indicating that a retinacular repair is required. A 3-cm incision is then made along the posterior margin of the lateral malleolus, exposing the tendon sheath and retinaculum. With the peroneal tendons held reduced in the peroneal groove, one to two suture anchors are
placed in the lateral malleolus to secure the detached tendon sheath and retinaculum. Tendon stability is then reassessed with a Freer elevator in the same manner.
placed in the lateral malleolus to secure the detached tendon sheath and retinaculum. Tendon stability is then reassessed with a Freer elevator in the same manner.
Closure Technique
A deep drain is placed exiting proximally in line with the vertical limb of the incision. Deep No. 0 absorbable sutures are then passed in interrupted, inverted fashion starting with the apex of the incision. Sutures are placed thereafter at the proximal and distal ends of the incision, and progressing toward the apex of the incision, while attempting to advance the flap toward the apex. The suture ends are temporarily clamped until all sutures have been passed (Fig. 33-6). The sutures are then hand tied in sequential fashion, starting at the ends proximally and distally, progressing toward the apex of the incision to minimize tension at the apex.
Allgöwer-Donati Suture
The skin layer is closed with 3-0 monofilament suture using the modified Allgöer-Donati technique, again starting at the ends and working toward the apex (Fig. 33-7




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree