CHAPTER 49 Biomechanics and Assessment of the Painful Shoulder
INTRODUCTION
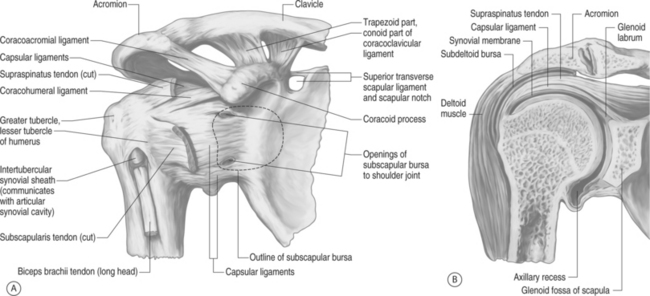
Spinal pain itself is complex in nature. To add another dimension to the diagnostic dilemma, the shoulder itself is among the most complex of all the body’s joints (Fig. 49.1). The shoulder is composed of four joints: the glenohumeral (GH), the acromioclavicular (AC), the sternoclavicular (SC), and the scapulothoracic (ST). It entails anywhere from 22 to 26 individual muscles and/or muscle slips, which are utilized for a combination of stability, power, and control of elevation and rotation. The shoulder is unique in that it is highly mobile, with an estimated 16 to 17 thousand positions in which the upper extremity may be placed, while necessarily exhibiting a concurrent lack of bony stability. The arm can move through approximately 180 degrees in elevation, 150 degrees of internal and external rotation, and flexion and extension or anterior and posterior rotation in the horizontal plane of approximately 170 degrees.1 The very interaction of the musculature both as agonist and antagonist must be coordinated for even the simplest motions in order for there to be an effective movement. An understanding of the anatomy and biomechanics of the shoulder is essential for clinicians who treat spinal disorders, as well as for other orthopedic practitioners.
ANATOMY
Sternoclavicular joint
Four ligaments and an intra-articular disc stabilize the sternoclavicular joint, which is mobile about all three axes (x, y, and z planes). The interclavicular ligament provides restraint to medial clavicular motion superiorly. It interconnects one medial clavicle to the other medial clavicle via its attachment to the sternum. However, this ligament may be absent or nonpalbable in 22% of individuals.2 The interclavicular ligament is taut when the arm is brought to the side. There are anterior and posterior capsular structures that prevent motion in the anterior and posterior planes; of the two, the anterior is the stronger restraint. The costoclavicular ligaments, which run obliquely and laterally from the first rib to the clavicle, provide for stabilization inferiorly. The posterior capsular structure is the strongest stabilizing force that resists downward motion, and the anterior structure resists superior motion of the medial clavicle.
Glenohumeral joint
The glenohumeral joint is what the layman and many in the healthcare field think of as the ‘shoulder joint.’ Although this joint is considered a ball (humerus) and socket (glenoid) joint, the socket covers only one-quarter of the humeral head.3–5 This ratio was initially calculated by the following simple formula, known as the glenohumeral index:
Maximum diameter of the glenoid:maximum diameter of humeral head
Saha recalculated the ratio to 0.6 in the transverse plane and 0.75 in the sagittal plane.6 Maki and Gruen further refined the ratio to 0.58 and 0.86 in a presentation to the Orthopedic Research Council in 1976.
Three different types of glenohumeral articulations have been identified, and in each case the humeral head is classified as being smaller, equal to, or larger than the radius of curvature of the glenoid.6,7 This difference is believed to impact a variety of shoulder instability patterns. A smaller glenoid surface diameter is necessarily a smaller effective contact surface for the humeral head and is thus a more unstable configuration.6,8,9 In the coronal plane, the articular surface of the glenoid comprises an arc of approximately 75 degrees, whereas the articular surface of the humeral head is roughly 120 degrees, or one-third of a sphere.
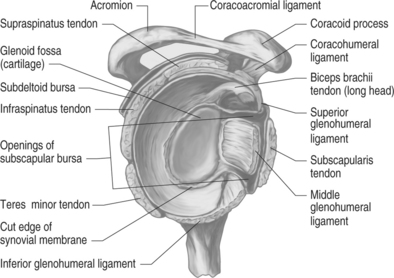
The glenoid labrum increases coverage about the humeral head by nearly 100%, and doubles the depth.10 The glenoid labrum is composed of dense fibrous connective tissue, and serves not only to increase the surface area and depth of the glenoid, but also to increase the structure’s load-bearing ability.11 The labrum is a structure which appears to be fibrocartilagenous in structure when examined superiorly but, as one approaches the inferior surface, is almost capsular in appearance. There are wide variations in labral anatomy among individuals, and there is no correlation between labral depth and glenoid size. Two aspects of labral anatomy that are fairly consistent are that the most stable, largest portion is the anterior and inferior area, and that the labrum itself acts to physically double the depth of the socket for the humeral head.
The glenohumeral joint allows for three distinctly different types of motion: spinning, sliding, and rolling. Spinning is when the contact point on the glenoid remains the same, but the contact point of the humeral head is changing. Sliding occurs when the contact point on the glenoid is changing, but that of the humerus remains the same. This generally occurs in unstable joints, and in extremes of motion in normal joints. The third type of motion, rolling, is when the contact points on both the glenoid and humeral head change.12
Anatomically, the proximal humerus is separated into four parts: the articular surface, the greater tuberosity, the lesser tuberosity, and the diaphyseal shaft. In relation to the shaft, there is a 45-degree medial angulation to the humeral head, and a 30-degree retroversion relative to the transcondylar axis of the distal humerus. The intertubercular groove lies between the greater and lesser tuberosities, and it is here that the tendon of the long head of the biceps lays.13 This tendon is held in place not only by the coracohumeral ligament, but also by the transverse humeral ligament. During shoulder abduction, the humeral head slides on this tendon. If the biceps tendon should rupture, anterior translation of the humeral head is subsequently increased.14
Utilizing an elegant approach, Johnson noted in 1937 that in order for the upper limb to maximally elevate, the humerus must externally rotate.15 Initially, research pointed to a physical obstruction caused by the coracoacromial arch to the greater tuberosity of the humeral head. By 1976, it was realized that this movement provides for loosening of the inferior ligaments of the glenohumeral joint while simultaneously allowing for optimal articulation with the glenoid.16 Thus, full arm elevation combined with external rotation is a position of greater stability than full elevation alone. This is due to a combination of relative laxity and stability of the three glenohumeral ligaments, intrinsic muscular forces, and negative intracapsular pressure.17
The ligamentous restraints of the glenohumeral joint are the inferior glenohumeral ligament (IGHL), the middle glenohumeral ligament (MGHL), and the superior glenohumeral ligament (SGHL) (Fig. 49.2). These glenohumeral ligaments, which insert onto the glenoid labrum and humeral neck, have often been described as ‘capsular thickenings.’15 This ‘capsular-ligamentous’ complex is the major static stabilizer of the shoulder, and although all of the ligaments are necessary for proper function, the IGHL is the most essential component of this complex. Studies have shown that the shoulder joint capsule possesses greater elasticity and twice the strength of that of similar structures within the elbow.19 The superior, middle, and inferior glenohumeral ligaments are considered the anterior glenohumeral ligaments.
The coracohumeral ligament, which runs laterally from the coracoid process to insert upon the superior–anterior aspect of the humeral head, is the most consistent of the ligaments of the shoulder capsule.20 In addition to providing an anterior stabilizing force to the biceps tendon, it also renders stability to the shoulder, particularly when the arm is in the dependent position.21
The superior glenohumeral ligament lies beneath the coracohumeral ligament, and has been found to contribute little to the stability of the glenohumeral joint. It also is a relatively constant structure, and arises from the tubercle of the glenoid, inserting upon the lesser tuberosity of the proximal humerus. The long head of the biceps tendon originates posteriorly to the SGHL. In concert with the superior tilt of the glenoid, the SGHL provides passive resistance to inferior subluxation and dislocation of the humerus.22
The middle glenohumeral ligament exists underneath the subscapularis muscle, and its presence is the most variable of the glenohumeral ligaments.20 Its origin is at the supraglenoid tubercle at the superior glenoid and anterior superior labrum, and inserts with the subscapularis muscle at the lesser tuberosity of the humerus. This ligament provides the majority of resistance to anterior humeral head displacement.20,23 It may measure up to 2 cm wide, and as much as 4 mm in thickness.24
The thickest of the glenohumeral ligaments is the inferior glenohumeral, which originates from most of the anterior glenoid labrum, and inserts on the inferior margin of the humeral head articular surface. The IGHL is the main static stabilizer in the abducted arm, and it reinforces the inferior capsule.25,26
A fundamental knowledge of the anatomy of the IGHL is instrumental in understanding the pathophysiology behind recurrent anterior humeral dislocation. When the humeral head dislocates in an anterior direction, the associated detached bone–labral complex essentially renders the IGHL an incompetent structure. The IGHL is composed of an anterior and posterior band with an axillary pouch in between.27 The anterior band serves as the major stabilizer of the glenohumeral joint when the arm is in abduction and external rotation.25 In this position, the anterior band appears to fan out, while the posterior band becomes cordlike. With the arm in internal rotation, the anterior band becomes cordlike, while the posterior band spreads into a fan shape to support the joint.
Codman’s paradox
While seated or standing, have the arm resting at the side with the medial epicondyle of a flexed elbow facing the midline of the trunk; take the arm to a position flexed forward to 90 degrees. Next, abduct the arm 90 degrees so that the epicondyle is then pointing perpendicular to the coronal plane. Then, bring the arm back to the side to its initial position. After performing these motions, the medial epicondyle is no longer facing medially towards the trunk, but is rather rotated away from the body in an ‘anterior’ position all without the humerus ever being actively axially rotated.15
Discussions have abounded surrounding this concept. It has been noted that the angular rotations involved with this movement do not add up to the concluding position, and that they are thus sequence dependent. The sequence of these complex rotations is what allows this phenomenon to occur. In aerospace terminology, these rotations are called the ‘Eulerian angles’ of yaw, pitch, and roll.10
Scapulothoracic joint
The scapulothoracic joint can be thought of as the base that stabilizes the shoulder girdle. Jobe and Pink28 have likened it to a seal balancing a ball on its nose. If that seal is able to stand still it can balance a ball for a lengthy time; however, if the seal is unable to obtain a stable position the ball will fall. This basic premise of strength at the base of the shoulder or core stabilization as referred to in spine rehabilitation is quite similar and will be discussed later. As noted above, the only bony attachment site of the scapula to the axial skeleton is at the acromioclavicular joint. Therefore, it is the muscular attachments, the scapulothoracic muscles, that are referred to as the scapular stabilizers. It is these muscles that act to position the scapula to the proper orientation on the thoracic cage for a given shoulder motion. These muscles include the trapezius, levator scapulae, serratus anterior, pectoralis minor, and rhomboids (major and minor). Shoulder abnormalities can stem from weakness or tears of one or all of these muscles. Disorders may also result from neuropathic abnormalities such as entrapment of the suprascapular nerve or compression of the dorsal scapular or long thoracic nerve, resulting in neuropraxia, neurotmesis, or axonotmesis. Space-occupying masses such as cysts or tumors as well as arthritic spurs and bony deformity in the glenohumeral joint can also result in abnormalities of function of the scapular stabilizers and hence the scapulothoracic joint.
BIOMECHANICS
The relative motion between the scapulothoracic articulation and the glenohumeral joint during shoulder abduction is termed the scapulothoracic rhythm.17,29–31 Over the entire arc of abduction, the glenohumeral joint moves more than the scapulothoracic joint; however, this difference is large at the beginning of abduction, and minimal at the end range of motion. Glenohumeral motion is much greater than scapulothoracic motion for the first 30 degrees of abduction; this ratio has been reported as ranging from 4:1 to 7:1.16,32 Over the subsequent 30–180 degrees of shoulder abduction there is less asymmetry between glenohumeral motion and scapulothoracic motion, and the ratio is then closer to 5:4.
The arc of full arm elevation involves anterior rotation of the scapula by about 6 degrees, with subsequent posterior rotation of the scapula on the order of 16 degrees until the arm is at its final resting position. That is, 10 degrees posterior to it’s starting position.33 In addition to these movements, there is also a simultaneous forward tilt of the scapula by 20 degrees.10,34
The articulation of the humeral head with the glenoid portion of the scapula was found by Saha6 to be posteriorly oriented by an average of 7 degrees in relation to the body of the scapula. This apparently minor retroversion is thought to be an important element of the static restraint system. It has been clinically correlated that those individuals with less retroversion have a greater tendency towards recurrent anterior dislocation at the glenohumeral joint. While there is agreement that there is a wide array of the amount of retroversion within individuals, there is still no consensus with regards to the clinical relevance, or in research with regards to these variations and their part in instability of the joint.
Resting muscle tension appears to account for much of the stability about the shoulder girdle. The base of the shoulder girdle is the scapula, and three groups of muscles concordantly maintain its stability: the posterior, intrinsic, and extrinsic groups.35 The scapulohumeral stabilizers comprise the posterior group of muscles, consisting of the trapezius, levator scapulae, rhomboids, and serratus muscles. This group helps to provide a stable base of rotation for glenohumeral motion, and maintains the glenoid in a position of maximal congruency with the humeral head, thus maintaining the proper length–tension relationship of the glenohumeral musculature.36,37 The intrinsic groups of muscles are the glenohumeral stabilizers and include the rotator cuff musculature: the supraspinatus, infraspinatus, teres minor, and subscapularis. Dynamic stability about the shoulder is dependent upon muscular forces generated by these muscles and those surrounding the scapulothoracic joint.38 The deltoid is the primary muscle of the extrinsic group, with biceps and triceps being secondary extrinsic muscles. These muscles comprise the primary positioners of the humerus and forearm.38
Inman and associates first described the concept of a ‘force couple’ in 1944.13 They described the dynamics of multiple forces passing across and through the shoulder during active motion to allow for any desired arm position. For example, their theory noted that if the deltoid were to pull the humerus superiorly, then the subscapularis, infraspinatus, and teres minor would act as a single functional unit to counteract any shearing forces that the deltoid placed upon the glenohumeral joint. This would then allow the humeral head to maintain itself in a congruent alignment to the glenoid by simultaneously depressing the humeral head and allowing the head to rotate about the glenoid.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree