The incidence of osteoporotic fractures has been steadily rising along with the aging of the population. Surgical management of these fractures can be a challenge to orthopedic surgeons. Diminished bone mass and frequent comminution make fixation difficult. Advancements in implant design and fixation techniques have served to address these challenges and when properly applied, can improve overall outcome. The purpose of this review is to describe fixation challenges of common osteoporotic fractures and provide options for successful treatment.
Key points
- •
The incidence of osteoporotic fractures is steadily increasing.
- •
Diminished bone mass and frequent comminution make fixation of osteoporotic fractures difficult.
- •
Locked plating enhances fixation stability in osteoporotic bone.
- •
Adequate fixation of unstable intertrochanteric fractures requires fixation with intramedullary device.
Introduction
Osteoporosis is a common disorder of the elderly, affecting nearly 8 million women and 2 million men in the United States alone. Driven by an imbalance in bone turnover, osteoporosis is characterized by decreased bone mass and altered bone microstructural properties. An increase in osteoclast activity combined with a decrease in osteoblast activity leads to overall bone mineral loss. Metaphyseal skeletal regions with a high proportion of cancellous bone are affected most severely. A diagnosis of osteoporosis is often heralded by the occurrence of a fragility fracture; common sites include the distal radius, proximal femur, distal femur, and proximal humerus. Each year, an estimated 1.5 million US adults sustain a fracture after a low-energy injury, such as a fall from standing height. The associated morbidity, mortality, and medical costs are significant. The 1-year mortality of elderly hip fractures has been reported to be as high as 30%, and the overall cost of osteoporotic fracture medical treatment is an estimated $18 billion a year.
Effect of osteoporosis on fracture fixation
Bone failure, not implant failure, defines the challenge of osteoporotic fracture fixation. Disease-driven alterations in structural bone properties substantially weaken implant fixation in osteoporotic bone, particularly when nonlocking screws are used. Multiple biomechanical studies have demonstrated an association between bone density and screw fixation strength. As bone mass decreases, so does the holding power of a screw. Screw and implant cutout are common modes of failure in osteoporotic bone. This situation is magnified in metaphyseal bone where the trabecular network of cancellous bone is especially affected by osteoporotic changes. An additional factor complicating overall success of osteoporotic fracture fixation is an increased frequency of fracture comminution in the setting of decreased bone mass. Despite that healing potential is unaltered in osteoporotic bone, impaired fixation increases the risk of reduction loss, malunion, and nonunion. Given these challenges, implant modification and novel designs have been developed in an effort to improve fixation in osteoporotic bone.
Introduction
Osteoporosis is a common disorder of the elderly, affecting nearly 8 million women and 2 million men in the United States alone. Driven by an imbalance in bone turnover, osteoporosis is characterized by decreased bone mass and altered bone microstructural properties. An increase in osteoclast activity combined with a decrease in osteoblast activity leads to overall bone mineral loss. Metaphyseal skeletal regions with a high proportion of cancellous bone are affected most severely. A diagnosis of osteoporosis is often heralded by the occurrence of a fragility fracture; common sites include the distal radius, proximal femur, distal femur, and proximal humerus. Each year, an estimated 1.5 million US adults sustain a fracture after a low-energy injury, such as a fall from standing height. The associated morbidity, mortality, and medical costs are significant. The 1-year mortality of elderly hip fractures has been reported to be as high as 30%, and the overall cost of osteoporotic fracture medical treatment is an estimated $18 billion a year.
Effect of osteoporosis on fracture fixation
Bone failure, not implant failure, defines the challenge of osteoporotic fracture fixation. Disease-driven alterations in structural bone properties substantially weaken implant fixation in osteoporotic bone, particularly when nonlocking screws are used. Multiple biomechanical studies have demonstrated an association between bone density and screw fixation strength. As bone mass decreases, so does the holding power of a screw. Screw and implant cutout are common modes of failure in osteoporotic bone. This situation is magnified in metaphyseal bone where the trabecular network of cancellous bone is especially affected by osteoporotic changes. An additional factor complicating overall success of osteoporotic fracture fixation is an increased frequency of fracture comminution in the setting of decreased bone mass. Despite that healing potential is unaltered in osteoporotic bone, impaired fixation increases the risk of reduction loss, malunion, and nonunion. Given these challenges, implant modification and novel designs have been developed in an effort to improve fixation in osteoporotic bone.
Fixation: general considerations
Screws
Screws are one of the most common implant types used in fracture fixation. Whether used in isolation for interfragmentary fixation or in combination with a plate, conventional screw fixation is dependent on the force generated between screw threads and the bone. Two basic screw designs exist, cortical and cancellous. For both types, screw purchase is reliant on thread engagement in bone tissue and highly dependent bone mineral density. Cortical screws are characterized by smaller thread diameter, a smaller pitch, and a shallower thread and are designed for placement in more dense cortical bone. As a general rule, screw fixation should be placed in cortical bone whenever possible to optimize purchase. The cancellous screw is a simple modification of screw design created to address reduced fixation strength in less-dense metaphyseal or osteoporotic bone. An increase in screw thread diameter and pitch provide more surface area for bone purchase. Once bone mineral density falls below 0.4 g/cm 3 , however, changes in screw geometry can no longer improve fixation strength.
Augmentation
Bone augments, including polymethylmethacrylate and tricalcium phosphate bone cement, have been used to increase screw purchase in weaker osteoporotic bone. Cement can be injected into porous regions of metaphyseal bone and left to harden. The drying cement interdigitates with the bone trabeculae, increasing the overall material density and thereby improving subsequent screw purchase. More localized cement application is achieved by direct injection of cement into newly drilled screw holes. After filling with cement, screws are inserted into the holes but not tightened until the cement has hardened. Cement augmentation has been suggested to improve screw pullout strength in osteoporotic bone. The majority of biomechanical testing of cement augmentation, however, has involved pullout testing of screw strength rather than functional loading, the latter of which is more representative of a clinical setting. A disadvantage of polymethylmethacrylate is that it does not reabsorb and becomes permanent, making it difficult to remove if the need arises. In addition, the exothermic curing process of cement may induce thermonecrosis to adjacent bone and compromise fracture healing. For these reasons, the authors do not advocate routine use of polymethylmethacrylate augmentation. An advantage of alternative bone augments, such as tricalcium phosphate cement, is that it is resorbable and osteoconductive. The tricalcium phosphate cement provides a scaffold for bone progenitor cells and over time is remodeled to a patient’s native osteoporotic bone. With both cement types, care must be taken to avoid placement directly into the fracture site, because this may impair healing between fragments.
Screws coated with hydroxyapatite or bisphosphonates have also been designed as a means of improving implant fixation. Hydroxyapatite functions to improve initial screw purchase, whereas the bisphosphonate coating promotes the development of increased bone mass at the screw-bone interface. Both materials have been shown in biomechanical cadaver and animal studies to improve screw fixation; however, augmentation using bisphosphonate coating takes time for the beneficial effects to occur (approximately 2 weeks).
Traditional Plates
Traditional plate fixation achieves fracture stability through creation of preload and friction force between the plate and bone, and it is, therefore, classified as a load-bearing device. In managing osteoporotic fractures, several principles can help to achieve success. In general, bridge plating of osteoporotic fractures should be done with caution, because it relies solely on the implant for stability without intrinsic bone contact, but with long comminuted segments is acceptable and can be successful. With increasing fracture gap, the strain across the implant grows, predisposing the construct to failure. The best way unload strain on the plate construct is to achieve cortical contact at the fracture site and, in the setting of comminution, this may require shortening of the bone. Shortening alters anatomy, however, and predictably creates a malunion, so intentional fracture shortening should be done with careful consideration. Thoughtful screw position is critical to creation of a successful construct. The working length of the plate, defined as the distance between the closest screws on either side of the fracture, is the most important determinant of the axial and torsional stiffness. In order to optimize stiffness and bending rigidity, screws should be positioned as close to the fracture as possible, while avoiding comminution. Longer plates have been shown to significantly improve bending strength. As described in a study by Sanders and colleagues, 8-hole and 10-hole plates with screw placement near the fracture site demonstrated improved biomechanical properties compared with a 6-hole plate with screws placed in every hole. The ideal plate construct minimizes working length and maximizes plate length, whereas the addition of intervening screws does little to improve fixation strength. Finally, surgeons should not underestimate the utility of buttress/antiglide plate fixation of osteoporotic fractures. Successful fracture alignment and stability can be achieved, even in osteoporotic bone, with placement of an antiglide plate in areas subject to shear force, such as the lateral malleolus and the proximal tibia. A properly positioned antiglide plate inherently prevents fracture displacement and minimizes the reliance on screw fixation.
Locking Plates
Plate design has evolved over the past decade to address difficulties associated with osteoporotic fracture fixation. The development of locked plating revolutionized fracture fixation in weaker bone, by shifting the focus of fracture stability to the screw/plate interface rather than relying on friction generated by a screw compressing plate to bone. Locked plating offers angular stability, with each screw becoming a fixed-angle device within the plate. Angular stability serves to minimize screw displacement under bending loads, because locking prevents screw toggle within the plate. Also, failure of locking plates requires failure of the entire screw plate construct, which differs significantly from traditional plating, where failure can result from loosening or cutout of a single poorly fixed screw. The biomechanical benefits of locked plating are especially helpful in weaker metaphyseal bone and osteoporotic diaphyseal bone. Locked plating, however, has not demonstrated an advantage over traditional plating in diaphyseal bone.
Challenges of Locking Plates in Osteoporotic Bone
Recent data have shown that the stiffness achieved with locked plating may be too high for certain osteoporotic fractures, stimulating modifications of locked plating technique. The fixed-angle design of locked screws results in increased stress at the screw-bone interface because there is no load transfer between the plate and bone surface, as seen in traditional plating. The high stiffness of the plate construct, relative to the low stiffness of osteoporotic bone, generates a stress-riser effect, predisposing the construct to periprosthetic fracture, especially under bending loads. The incidence of secondary periprosthetic fracture after locked plating has been reported to be as high as 2.6%. Replacement of the outermost locked screws with traditional screws has been shown to improve bending strength by 40% without affecting the ability of the plate to withstand torsional or compressive loads.
The increased stiffness that characterizes locked plates has also been implicated in fracture nonunion. Fixed-angle stability makes locked plating an attractive option in the treatment of comminuted fractures. Fixation of comminuted fractures, however, especially those in periarticular regions, relies on micromotion between fracture fragments and secondary healing through callus formation. Rigid locked fixation may eliminate this micromotion and contribute to a high nonunion rate of up to 19% in fractures, such as the distal femur. Several methods have been described to decrease stiffness and enhance interfragmentary micromotion in locked plate constructs. The technique of far cortical locking reduces construct stiffness without compromising strength. The midshaft of far cortical locking screws is modified such that the screws lock into the far cortex and the plate but bypass the near cortex. The increased working length of the screw results in a reduction in stiffness and allows for parallel interfragmentary motion at the near cortex, which promotes callus formation and fracture healing. Furthermore, far cortical locking constructs display a biphasic stiffness behavior. Under smaller loads, stiffness of the construct is low, but stiffness gradually increases with progressively higher loads. At high loads, far cortical locking results in a construct that is 54% stronger in torsion, 21% stronger in bending, and 84% as strong under compression compared with standard locked plating. This technique can be applied to periarticular fractures, where far cortical locking screws are placed in the diaphyseal segment and standard locking screws are used in the metaphyseal and periarticular portions, which lack a far cortex. An alternative to far cortical locking is the use of near cortical slots. The use of slotted holes at the near cortex in place of standard holes functions similarly to the far cortical locking technique in that construct stiffness is reduced while overall fixation stability is maintained. The cost with these newer technologies is much greater than conventional implants, and similar stiffness effects may be obtained with cortical screw fixation in the diaphyseal segment.
An additional disadvantage of pure locked plating is the inability of the plate-screw construct to facilitate reduction. Although compression generated between a traditional screw and plate can be used to affect fracture reduction, the insertion of a fixed-angle screw does not reduce a fracture. When using pure locked plating construct, surgeons must reduce the fracture before fixation. The advent of hybrid plates combines the advantages of traditional and locked plating. Hybrid plates contain holes, which accommodate both traditional and locked screws. The sequence of fracture fixation with hybrid plates proceeds as follows: the bone is reduced to the plate using a traditional screw and then locking screws are placed to improve construct strength and protect the cortical screws. Despite initial concerns about construct stability, the addition of nonlocked screws results in minimal reduction in axial strength, improved torsional strength, and equivalent bending strength compared with fully locked plates. When using a hybrid technique in osteoporotic diaphyseal bone, a minimum of 3 bicortical locking screws should be inserted on either of the fracture to optimized torsional stiffness. Locking screws placed on either end of nonlocked screws has also been suggested as having a protected effect and minimizing construct fatigability.
Intramedullary Nails
Intramedullary nails (IMNs) are another common implant choice and the gold standard for diaphyseal fractures of the tibia and femur. IMNs are load-sharing devices and less susceptible to implant failure compared with plate fixation. The central location of the nail within the medullary canal distributes load equally across the construct, in contrast to plate fixation in which stress is eccentrically focused on the implant side of the cortex. Insertion of the nail proximal or distal to the fracture site allows for preservation of the surrounding soft tissue, periosteum, and fracture hematoma, further promoting healing. In treating osteoporotic patients, wide-diameter nails may be required to accommodate the expansion of the medullary canal seen in osteoporosis. Fracture fixation with an IMN generally allows for early weight bearing, a useful advantage in elderly patients where immobility is associated with increased morbidity.
Fracture fixation with an IMN requires placement of interlocking screws to achieve control of axial and rotational displacement. The weakness of IMN fixation, especially in osteoporotic bone, is the strength of interlocking screw fixation at the metaphysis. The same challenges of screw purchase in weak bone seen with plates arise here as well. Alternations to distal interlocks may be necessary to achieve adequate fixation in weaker bone. Placement of interlock screws in multiple planes has been shown to enhance fixation, as has cement augmentation or use of a washer. Other newer designs offer a blade-like device as an interlock and fixed-angle interlocking screws.
Osteoporotic fracture fixation is challenging and often requires different techniques and implants to maximize fixation. With the availability of locking screws and locking periarticular plates, screw augmentation with cement is not commonly used. In the diaphyseal segment of osteoporotic fractures, locking screws can improve fixation strength, whether used exclusively or in combination with cortical screws (hybrid fixation). For metaphyseal osteoporotic fractures, nails provide some advantages, but locking plates may facilitate reduction and provide more fixation points in the short end segment and should be considered strongly.
Proximal humerus
Introduction
Fractures of the proximal humerus are some of the most common types of fragility fractures. More than 184,000 emergency room visits in 2008 were for proximal humerus fractures and it is projected that, by 2030, 275,000 proximal humerus fractures will be seen in emergency departments each year. The fracture rates per 100,000 individuals increase exponentially as age increases and are particularly pronounced in women. Despite the increasing burden of proximal humerus fractures, most do not require operative treatment. Nondisplaced fractures represent up to 85% of all proximal humerus fractures, the majority of which can be successfully treated nonoperatively. At some centers, however, referrals increase the incidence of displaced 2-part, 3-part, and 4-part fractures and may compromise up to 53% of all proximal humerus fractures that are seen.
Despite the high percentage of nondisplaced and stable fractures, some patients with displaced and unstable fractures benefit from operative fixation to restore anatomy and allow early rehabilitation. Operative fixation of osteoporotic proximal humerus fracture is challenging and is related to the anatomy of the proximal humerus in osteoporotic patients, specifically the small tuberosity fragments, the poor bone quality, and the inability to place bicortical screws into the humeral head. The proximal humeral head, in particular the central portion, and humeral metaphysis are common areas of resorption during osteoporosis. The humeral head has even been described as similar to an eggshell or a grapefruit, which helps understand how the quality of bone, coupled with the inability to place bicortical fixation in the humeral head, limits a surgeon’s ability to obtain and maintain secure fixation. In addition to osteoporosis, avascular necrosis is another consideration when treating osteoporotic proximal humerus fractures and is a result of the traumatic and surgical insult to the tenuous blood supply to the humeral head. The posterior humeral circumflex artery tends to be the dominant arterial supply to the humeral head. This blood supply is damaged at the time of injury in approximately 80% patients; however, neovascularization is believed to occur with preservation of perfusion observed even in 3 and 4 part fractures. With proper surgical technique and careful attention to avoid unnecessary soft tissue stripping, avascular necrosis is a rare complication, with necrosis occurring in 2.3% to 3.1% of patients in 2 recent case series.
Surgical Techniques
Closed reduction and percutaneous pinning
Closed reduction and percutaneous pinning can be a viable surgical option; however, the indications for this technique are narrow. Fractures must not extend below the surgical neck, the fracture must be minimally comminuted, and the fracture must be able to be reduced and stabilized in a closed or minimally open fashion. The advantages of this procedure are that minimal soft tissue stripping may lead to less avascular necrosis and increased postoperative range of motion. Intermediate outcomes for patients treated with closed reduction and percutaneous pinning have revealed that osteonecrosis is a late occurrence, as far as 8 years after initial intervention. Overall, the need for revision surgery is not increased despite the increased incidence of late osteonecrosis.
Intramedullary nail
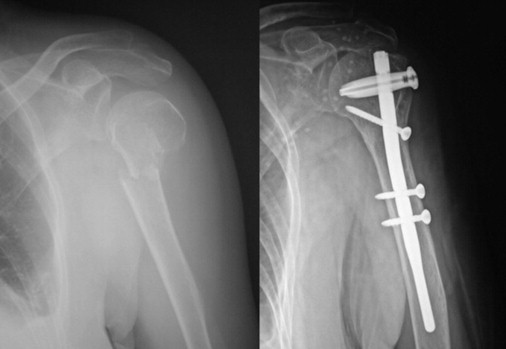
Recent development of specialized IMNs has led to an increased interest in using locked nails as an alternative to open reduction and internal fixation (ORIF) with locking plates. IMNs, in theory, involve less soft tissue stripping and offer the advantage of a load-sharing device. IMNs can be used to treat 2-part, 3-part, and 4-part fracture patterns but are best suited to 2-part fractures. Meticulous surgical technique must be used to preserve and repair the supraspinatus tendon and to avoid nail prominence. A recent randomized controlled trial demonstrated that at 3-year follow-up, outcomes between the IMN and locking plate groups were similar for American Shoulder and Elbow Surgeons score, pain, and supraspinatus strength. In this trial, the locked nail had significantly shorter operative times and less blood loss ( Fig. 1 ).
Locking plates
Specialized locking plates designed for the proximal humerus allow for ORIF of proximal humerus fractures. The specialized designs allow for multiple locking screws to be placed into the humeral head, which help decrease the risk of screw pullout and varus collapse. Certain plate designs also now incorporate holes for sutures, which can be used to augment repairs, particularly for tuberosity fragments and comminuted fracture patterns. Care must be taken to avoid superior placement of the plate, which causes impingement with shoulder abduction. Furthermore, there is a risk of screw penetration into the articular surface as the surgeon attempts to obtain good screw purchase in the dense subchondral bone. Restoration of the medial calcar and proper placement of an inferomedial oblique screw in the humeral head is thought to increase the likelihood of maintaining fracture reduction. Additionally, structural augmentation with either calcium phosphate cement or a fibular strut allograft may substantially reduce the risk of reduction loss and implant failure ( Fig. 2 ).
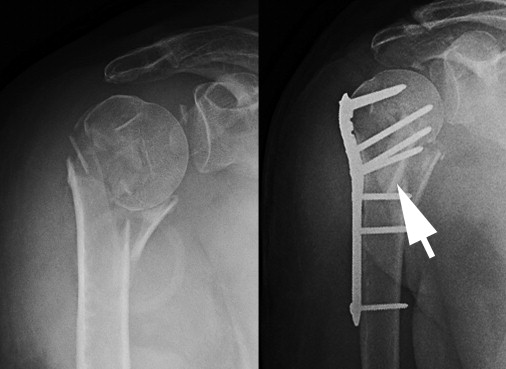
Shoulder arthroplasty
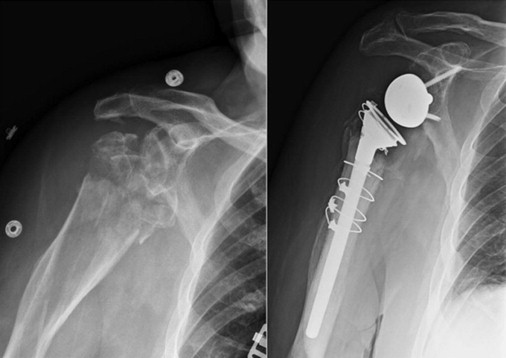
Shoulder arthroplasty was once recommended as the primary treatment of 3-part and 4-part fractures; however, this has fallen out of favor in a majority of these fracture patterns. As site-specific locking plates have been developed, the concern for avascular necrosis and nonunion has decreased. Furthermore, nonunion or malunion of tuberosity fragments have been shown to correlate with poor outcomes. For these reasons, shoulder arthroplasty has become a salvage procedure in most cases. Primary arthroplasty still may be the best surgical option in the face of multifragmentary head cleavage or early avascularity of the head fragments ( Fig. 3 ).
Clinical Outcomes and Complications
Patient outcomes after fixation of osteoporotic proximal humerus fractures are generally good but can vary with patient age and fracture pattern. Advanced age and more complicated fracture types are associated with worse outcomes. Patients should be counseled that their functional outcomes are likely to continue to improve over a long period of time and that their outcome is also greatly influenced by postinjury or postoperative rehabilitation.
Successful outcome can be achieved with multiple techniques. ORIF with a locked plating remains a reliable method for unstable 2-part, 3-part, and 4-part fractures. Postoperative Constant scores of an average of 70 can be achieved at 1 year. Complications include osteonecrosis, screw perforation of the humeral head, and loss of fixation. Locked IMN fixation is another option, best used in patients with 2-part fractures involving the surgical neck. Lower complication rates (4% vs 31%) have been reported with IMNs compared with locked plate fixation of similar fracture patterns.
Given the high frequency of poor quality bone, closed reduction and percutaneous pinning are not often used in the treatment of the majority of osteoporotic proximal humerus fractures. Finally, hemiarthroplasty is indicated in those fractures not amenable to fixation, such as fractures with significant comminution or with head splitting patterns. Hemiarthroplasty has been shown effective in alleviating pain, but unpredictable limitations in range of motion have been reported in some patients postoperatively, worsening patient-rated outcome. Tuberosity displacement or nonunion is a worrisome complication of shoulder hemiarthroplasty.
Humeral shaft
Introduction
Fractures of the humeral shaft have an incidence of 3% to 5%, account for more than 57,000 emergency department visits annually in the United States, and tend to occur in a bimodal age distribution. The first peak is in young men and the second peak in elderly female patients. Fractures occurring in patients older than 50 years of age account for 60% of the total humeral diaphyseal fractures observed and represent a true fragility fracture.
Most humeral shaft fractures can be treated nonoperatively. Functional bracing, first described by Sarmiento and colleagues, expect to have successful outcomes in 90% of cases. Furthermore, 98% of closed injuries and 94% of open injuries go on to clinical union with conservative treatment. Malunion (greater than 16° of angulation in any plane) occurs with greater frequency in nonoperatively treated fractures, resulting in combined varus and apex-anterior deformities in 13% and 19% of cases. Injury to the radial nerve at the time of humeral shaft fracture occurs in approximately 8% to 18% of patients with closed injury. This injury is most common in spiral and transverse fracture patterns. Full recovery of the radial nerve can be expected to occur in 70% of patients treated conservatively over 4 months and approaching 90% overall.
Despite the overall success of conservative management, operative stabilization is necessary in certain fracture and patient types. Gustilo type III injuries, often with gross instability and soft tissue stripping, require irrigation, débridement, and immediate stabilization through internal or external fixation. Patients with ipsilateral brachial plexopathies have been shown to develop nonunion in 45% of a case series of 21 patients. Fracture patterns with proximal extension may fail functional treatment up to 46% of the time and should be observed closely for potential early surgical intervention. Patients who are obese also may have soft tissues that tend to force their alignment into an unacceptable varus deformity and may require early operative intervention.
Surgical Techniques
Intramedullary nail
IMN of diaphyseal humerus fractures has had disappointing outcomes, even with the development of locked nails to control rotation. In theory, the advantage gained from using a load-sharing device with less soft tissue stripping has not borne out improved outcomes. A recent Cochrane review has shown that although functional outcomes are similar between IMN and ORIF methods, hardware removal is significantly more frequent in patients treated with IMN and is most often indicated for shoulder impingement. A randomized prospective study by Putti and colleagues similarly showed that although American Shoulder and Elbow Surgeons scores were similar between IMN and ORIF groups (45.2 and 45.1, respectively), complication rates were significantly higher in the IMN group (50% vs 17%). A meta-analysis comparing plate fixation with IMN demonstrated no difference in infection, nonunion, or radial nerve palsy but a higher incidence of symptomatic shoulder impingement and reoperation was observed with IMN fixation.
Open reduction and internal fixation
ORIF with plate and screw constructs is the mainstay of surgical intervention in humeral shaft fractures when operative intervention is indicated. There has been a substantial focus in the literature on proper fixation techniques for diaphyseal humerus fractures in osteoporotic bone models. As locked plating technology has been developed, the literature suggests that diaphyseal fracture of the humerus benefit greatly from increased stability of this technology. Initially demonstrated in bone substitute models and redemonstrated in biomechanical studies on matched cadaver constructs, locked or hybrid (mixed locked and unlocked) screw constructs are mechanically superior to unlocked constructs ( Fig. 4 ). The stiffness of purely locked constructs has been implicated in impaired fracture healing. With hybrid fixation, it is recommended that locked screws be placed on either end of the fracture to attain optimal strength ( Fig. 5 ). Furthermore, consideration should be given to the number of screws used in the construct. A recent study has suggested that a 4-screw construct, with 2 cortices above and 2 below the simulated fracture site, had superior resistance to catastrophic failure than a 6-screw construct. In this study it was theorized that the increased screw density created a stress riser, predisposing the 6-screw construct to fail at lighter loads.








