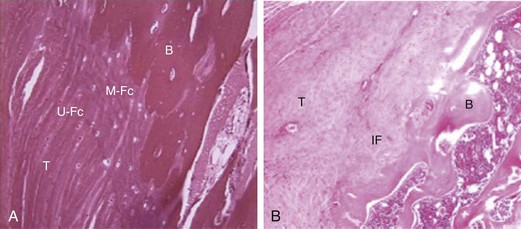
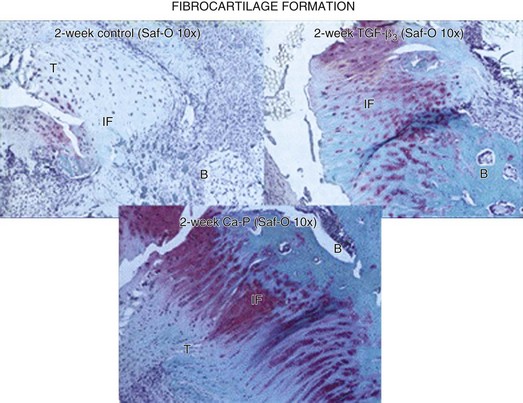
Chapter 37 Rotator cuff pathologies are among the most common causes of shoulder pain. The incidence of rotator cuff tears is known to increase with age, particularly over the age of 50 years. Torn rotator cuff tendons are associated with increased pain and poorer shoulder function. A significant proportion of torn rotator cuff tendons retear after surgical repairs, and failure rates of 30% to 70% are frequently reported. The biologic milieu that precedes and follows rotator cuff tears has been shown to contribute to rotator cuff tear pathogenesis. The increasing health burden of rotator cuff tears has encouraged investigation into biologic adjuncts that may be used to augment surgical repairs of rotator cuff tendons with the aim of ultimately reducing high failure rates. It is hoped that biologic adjuncts will encourage regeneration of functional tendon tissue rather than mechanically inferior scar tissue that usually forms at the healing rotator cuff enthesis (Fig. 37-1).1 Modulating Cytokines and Growth Factors Matrix metalloproteinases (MMPs) and their inhibitors (tissue inhibitors of matrix metalloproteinases [TIMPs]) control the balance between synthesis and degradation of the ECM. The most important regulators of the ECM include MMPs 1, 2, 3, 9, and 10 as well as TIMPs 2, 3, and 4. Manipulation of MMP-related pathways are proposed to encourage tendon regeneration. Tetracyclines inhibit collagenase via an interleukin (IL)-1β–mediated release of MMP-3. One such example, doxycycline, was reported to improve the histology and mechanics of rotator cuff tendon healing in a rat model.2 Recapitulating embryonic tendon differentiation may help to replicate the scarless healing process that is seen in the embryo. TGF-β3 plays a role in wound healing and embryonic tendon development, and therefore a number of studies have investigated the effects of localized TGF-β3 delivery to healing tendon sites.3,4 TGF-β3 delivery resulted in improved collagen I expression, vascularity, cellularity and cell proliferation. Improvements in histology and mechanical properties were also noted (Fig. 37-2). Effects of some growth factors may be temporally mediated and depend on the phase of healing during which they are delivered. For example, fibroblast growth factor 2 (FGF-2) delivered both with and without scaffolds was found to improve the histology and biomechanical properties of healing supraspinatus tears in rats at early rather than later time points.5,6 Another cytokine that is thought to be detrimental to rotator cuff healing is the proinflammatory mediator tumor necrosis factor α (TNF-α), and its effects appear to be affected by timing. A study of the effects of TNF-α blockade found an early improvement in mechanical properties only at 2 and 4 weeks, but the improvement was no longer present at 8 weeks.7 Ultimately, the effectiveness of cytokine- or growth factor–mediated enhancement of rotator cuff healing may be determined by a number of factors related to delivery, such as concentration, timing of delivery, and delivery modality. One interesting approach taken was to coat sutures with platelet-derived growth factor (PDGF-BB), and although it improved the histology of the rotator cuff, there was no effect on mechanical properties.8 Biologic and synthetic scaffolds are increasingly used as a delivery vehicle for growth factors, to ensure localized delivery and retention. Targeted delivery can be achieved by seeding transduced cells that express desired factors to the site of the rotator cuff repair. Another approach to ensure higher levels of growth factor and cytokine delivery is to use concentrated autologous platelets as a delivery vehicle in the form of platelet-rich plasma (PRP), which is classified as an autologous blood product rather than a drug (Fig. 37-3). Few randomized controlled trials have studied PRP application to rotator cuff repairs, and these studies have failed to demonstrate an improvement in healing after PRP treatment, which calls into question the efficacy of PRP use for rotator cuff tears. Two randomized controlled trials looking at the effects of platelet-rich fibrin matrix in 88 and 79 patients found there was no significant difference in clinical outcomes or healing rates compared with primary closures alone.9,10 However, a smaller randomized controlled trial in 20 patients reported a significant increase in blood flow in the PRP group, but this did not translate to improved clinical scores.11 Questions remain about the ideal concentration system, cellular content, platelet count, and timing of delivery.
Biologics in Rotator Cuff Repair
Drug Treatments That Improve Healing
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Biologics in Rotator Cuff Repair