Bernese Periacetabular Osteotomy
Travis H. Matheney
Michael B. Millis
DEFINITION
Hip dysplasia is the most common etiology of coxarthrosis, often leading to arthroplasty long before joint replacement can be considered a lifetime solution.3
Surgical realignment of the congruous dysplastic acetabulum can improve or eliminate symptoms for years, sometimes indefinitely, in a majority of appropriately selected patients, even in those with some degree of preoperative arthrosis.1, 3, 4, 6, 7, 8
Age limits for this procedure are adolescence (closed triradiate cartilage) to an indefinite upper age limit (limited by preoperative arthrosis and other considerations that might make arthroplasty a better choice).
ANATOMY
The acetabulum lies between the anterior and posterior columns of the pelvis.
The most common area of acetabular deficiency in developmental dysplasia of the hip (DDH) is anterior and lateral.
The Bernese periacetabular osteotomy (PAO) differs from the triple osteotomy primarily by maintaining the integrity of the posterior column of the pelvis.
The Bernese PAO uses up to five steps to divide the acetabular fragment from the remainder of the pelvis, allowing multiplanar reorientation.
Important bony landmarks include the following:
Iliopectineal eminence (which marks the medialmost extent of the acetabulum)
Infracotyloid groove (just distal to the acetabulum, where the obturator externus tendon lies; this is the site of the anterior ischial osteotomy)
Anterior superior iliac spine (ASIS)
Apex of the greater sciatic notch
Ischial spine
The posterior column is triangular and thickest just posterior to the acetabulum; it becomes much thinner closer to the sciatic notch. For this reason, the optimal plane for the posterior column is angled obliquely to the medial cortex and perpendicular to the lateral cortex of the ischium-posterior column.
PATHOGENESIS
Genetic and developmental causes exist for “developmental dysplasia.”
Neuromuscular: Charcot-Marie-Tooth disease and spastic diplegia
Posttraumatic: injuries to the triradiate cartilage and aggressive excision of the limbus in the infant hip
NATURAL HISTORY
There is a clear correlation between acetabular dysplasia and osteoarthrosis of the hip.
The more severe the acetabular dysplasia and any subluxation, the earlier the onset of symptoms from arthrosis.
Murphy et al5 found that every patient with a lateral center-edge angle less than 16 degrees developed osteoarthritis by age 65 years.
PATIENT HISTORY AND PHYSICAL FINDINGS
Key portions of the history include the following:
Personal or family history or treatment of DDH
History of other hip disorders, including Legg-Calvé-Perthes
Trauma
Skeletal dysplasias
History of cerebral palsy
Birth order and weight
Description of pain or mechanical symptoms, including location, duration, activity limitation, giving way, “clicking,” “catching,” and “popping”
Physical examination should include gait, limb length, assistive devices, and strength.
Specific hip tests include the following:
Trendelenburg test: demonstrates weakness in abductors
Anterior apprehension test: A positive result is a subjective noting of “apprehension” or instability by the patient.
Anterior impingement test (pain with passive hip flexion, adduction, and internal rotation): test of anterior labral pathology, not just a tear
Bicycle test for abductor fatigability
Range of motion (ROM): Dysplastic hips may demonstrate a relative increase in flexion due to anterior acetabular un-coverage. Decreased ROM with pain may indicate arthrosis.
IMAGING AND OTHER DIAGNOSTIC STUDIES
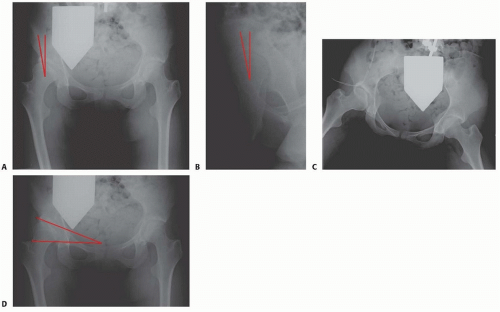
Radiography includes weight-bearing anteroposterior (AP) views of bilateral hips (FIG 1A), false profile of hips (FIG 1B), and AP views of the hips in maximal abduction and internal rotation (von Rosen view; FIG 1C). These studies allow assessment of lateral and anterior coverage of the femoral head as well as congruency of the hip joint. Additionally noted will be the presence of hinge abduction, which is a relative contraindication to PAO.
Radiographic parameters include the following:
Lateral center-edge angle of Wiberg measured from AP view of the hip (lower limits of normal about 25 degrees; see FIG 1A)
Anterior center-edge angle of Lequesne and de Seze (lower limits of normal 20 degrees measured on the false-profile view; see FIG 1B)
Tönnis acetabular roof angle measured on the AP view of the hip (upper limits of normal 10 to 15 degrees; FIG 1D)
Crossover sign (anterior wall shadow crossing posterior wall shadow on AP view of the pelvis)
Assessment of the line of Shenton for breaks indicative of femoral head subluxation
Computed tomography (CT) scan of both hips with three-dimensional reconstruction as well as with axial slices through the femoral condyles may be of assistance in preoperatively assessing the amount and direction of correction required as well as the potential need for proximal femoral osteotomy.
Magnetic resonance imaging (MRI) of involved hips with radial sequences centered at the femoral head allows assessment of articular and labral cartilage.
Delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) is a recently developed technique that assesses the mechanical damage to the articular cartilage. It has been demonstrated to be a better preoperative predictor than plain radiographs in determining outcome after PAO.2
NONOPERATIVE MANAGEMENT
Activity and job modification may be of benefit in delaying or mitigating arthritic symptoms.
Physical therapy may be of some benefit in increasing ROM and strength. To date, there are no data to suggest that a specific therapy regimen can affect the onset of arthritis in the dysplastic hip.
SURGICAL MANAGEMENT
Indication: symptomatic, congruous acetabular dysplasia (closed triradiate cartilage) with lateral and anterior center-edge angles 18 degrees or less
Contraindications: Tönnis osteoarthrosis grade 2 or more (subchondral cysts, significant joint space narrowing), severe limitation of motion secondary to arthrosis, active joint infection
Preoperative Planning
Radiographs and MRI are evaluated to assess the following:
Degree and character of dysplasia
Amount and direction of correction required to normalize the Tönnis acetabular roof angle (0 to 10 degrees), correct subluxation, and improve mechanical stability
Proximal femoral deformity may also require treatment at time of PAO.
Presence of acetabular articular or labral lesions (seen on MRI) should also be taken into consideration, as treatment either arthroscopically (before the osteotomy) or intraoperatively through limited arthrotomy may be required for best long-term results.
Isolated treatment of a labral lesion in the presence of acetabular dysplasia is contraindicated. Simultaneous acetabular realignment must be considered.
The torn acetabular labrum is usually associated with other structural abnormality within the hip (femoroacetabular impingement or DDH), which may also require correction for best results.9
Partial weight-bearing technique is taught preoperatively in preparation for postoperative mobilization.
For perioperative pain management, we recommended considering either epidural or lumbar plexus catheter placement preoperatively as well as multimodal perioperative analgesia. Catheters are removed the morning of postoperative day 1 or 2.
Positioning
The patient is positioned supine on a radiolucent table.
The operative extremity is prepared and draped free up to the costal margin; the surgeon should be certain to prepare and drape posteriorly to at least the posterior third of the ilium and medially to the umbilicus.
Approach
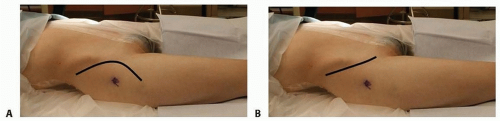
The standard longitudinal anterior Smith-Petersen incision and approach to the hip provides the appropriate access (FIG 2A).
As an alternative, an ilioinguinal (bikini) incision may be used followed by a similar deep approach (FIG 2B). This incision typically provides a better cosmetic result but can limit access for the anterior ischial osteotomy. Therefore, we recommend the standard anterior incision for larger and more muscular patients.
TECHNIQUES
▪ Superficial Dissection
The skin is incised into subcutaneous tissue.
The fascia over the external oblique and gluteus medius is identified and incised posterior to the ASIS, and the plane between the two muscles is developed to expose the periosteum over the iliac crest.
The periosteum is sharply divided over the iliac crest and subperiosteal dissection carried out over the inner table of the ilium. This space is packed with sponges for hemostasis.
Entry into the tensor fascia lata-sartorius interval is initially accomplished via the compartment of the proximal tensor fascia lata to avoid injury to the lateral femoral cutaneous nerve. The tensor fascia lata is bluntly elevated off the intermuscular septum and the compartment floor is identified proximally until the anterior ilium is palpated.
Once hemostasis is attained, the ASIS is predrilled with a 2.5-mm drill and the anterior 1- × 1- × 1-cm portion is osteotomized to facilitate the medial dissection and later repair.
Alternatively, the sartorius can be taken off with just a thin wafer of bone that will be sewn back in place at the end instead of with a screw.
Subperiosteal dissection is continued to the anterior inferior iliac spine (AIIS).