Basic Science of the Knee
Donald H. Johnson MD, FRCS
Paul Johnson MD
Ali Alsuwaidi MD, FRCSI, FRCSC
The knee joint is considered to be three separate compartments, the patellofemoral, the medial, and the lateral compartments.
The knee has no inherent bony stability, but depends upon the ligaments to provide stability.
The patellofemoral joint consists of the patella, the trochlea, and the stabilizing quadriceps mechanism.
The condyles of the femur articulate with the condyles of the tibia but are asymmetrical and appear to have no inherent stability.
The anterior cruciate ligament (ACL) is a two-bundle ligament with a small isometric attachment to the tibia and femur. The tension in the two bundles varies with knee flexion; the anteriomedial is tight in flexion and the posterolateral tight in extension.
The posterior cruciate ligament (PCL) is also a two-bundle ligament with a small central isometric point on the femur.
The pes anserinus muscles (sartorius, gracilis, and semimembranous muscles) are flexors and internal rotators of the knee, which act as dynamic stabilizers.
The medial and lateral meniscus are concentric lamellae that serve to deepen the contact of the tibia and provide stability to the femur.
Articular cartilage is a thin layer of specialized connective tissue lining the articulations of diarthrodial joints.
Age, mobilization, pregnancy and the post-partum state, and medications all are factors affecting the biomechanical properties of tendons and ligaments.
The function of the articular cartilage is significant as the knee joint reaction force at the tibiofemoral joint is about three times body weight in walking. The joint reaction forces are absorbed by the menisci along with the articular cartilage in the normal biomechanics of the knee.
Soft tissue can be divided into dense, loose, and adipose subtypes depending on the histological appearance.
Soft-tissue healing is a structured process that takes place over a specific period of time in a very coordinated way. Different tissues have different repair capacities for a variety of environmental and genetic factors.
In the multi-ligament injury, reconstruction of the ACL may impart stability to the injured medial collateral ligament (MCL) and allow it to heal in a satisfactory manner without the need for primary repair.
This description of anatomy of the knee will be presented with an emphasis on the practical surgical approach to each structure. The knee joint is considered to be three separate compartments, the patellofemoral, the medial, and the lateral compartments. The knee has no inherent bony stability, but depends upon the ligaments to provide stability.
Bone
The Patellofemoral Joint
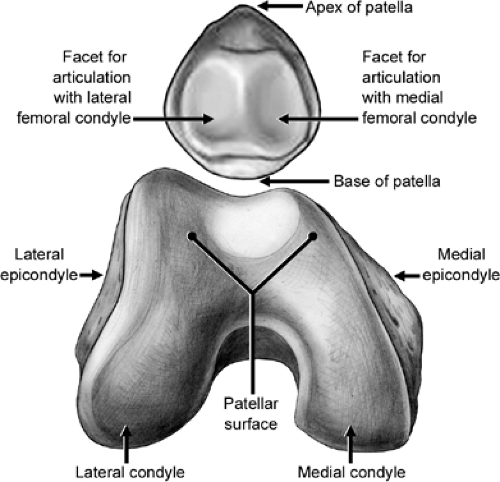
The patellofemoral joint consists of the patella, the trochlea, and the stabilizing quadriceps mechanism (Fig 33-1). In the normal situation, the trochlea provides stability to the patella, but with dysplasia of the lateral facet of the trochlea, and muscular imbalance, lateral instability of the patella occurs. The patella has seven facets, the three lateral: superior, medial,
and inferior, the three medial: superior, medial, and inferior. The medial odd facet has no articulation with the trochlea. The degree of contact between the patella and trochlea varies with knee flexion. The distal portion of the patella articulates in extension, and with increasing flexion the patella is drawn into the trochlea groove. In full flexion, the proximal patella articulates with the femur.
and inferior, the three medial: superior, medial, and inferior. The medial odd facet has no articulation with the trochlea. The degree of contact between the patella and trochlea varies with knee flexion. The distal portion of the patella articulates in extension, and with increasing flexion the patella is drawn into the trochlea groove. In full flexion, the proximal patella articulates with the femur.
The patellar tendon joins the patella to the anterior tibia, and is of variable length, but averages about 5 cm. The ratio of length of the patella tendon to the length of the patella determines the position of the patella in the femoral groove. An excessively long tendon results in patella alta, with the patella lying above the trochlea in extension.
The quadriceps tendon attaches to the superior aspect of the patella. The medial patella femoral ligament stabilizes the patella on the medial side. This ligament attaches to the femur at the epicondyle, and to the patella just above the midportion. The lateral retinaculum has several thickened bands, forming the lateral stabilizing structures.
The Tibiofemoral Joint
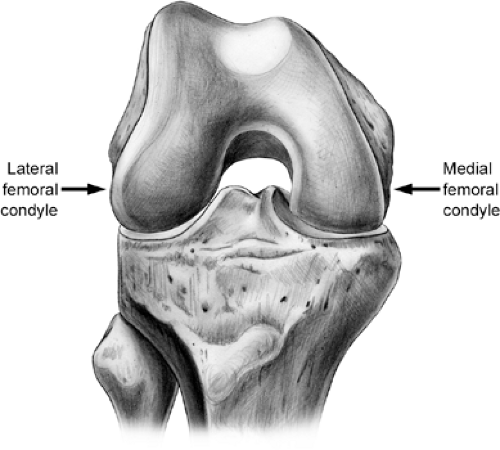
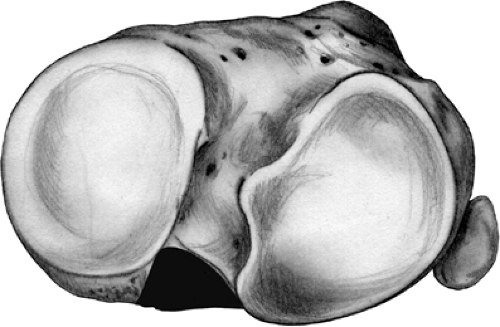
The condyles of the femur articulate with the condyles of the tibia, but are asymmetrical and appear to have no inherent stability (Fig 33-2). The larger medial femoral condyle is round, and the lateral condyle is longer, and wider at contact with the tibia. The medial tibial plateau is flat, but the lateral tibial plateau is convex. Both tibial plateaus have a posterior inclination of 10 degrees. The meniscus provides increased stability by deepening the concavity of the tibia. The intercondylar notch of the femur is occupied by the anterior and posterior cruciate ligaments (PCLs). On full flexion of the knee there is a posterior translation of the tibial on the femur through a combination of gliding and rolling of the femur.
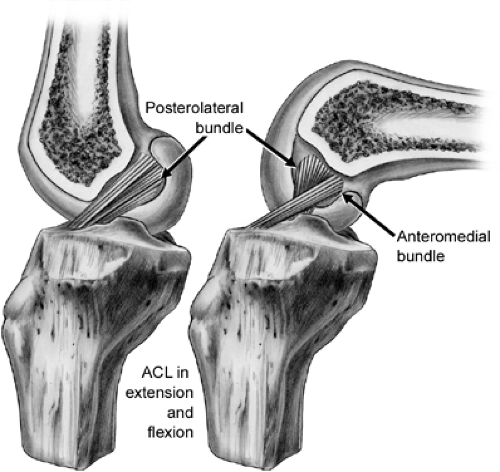
The Anterior Cruciate Ligament
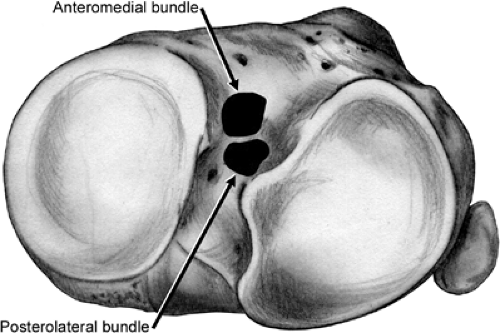
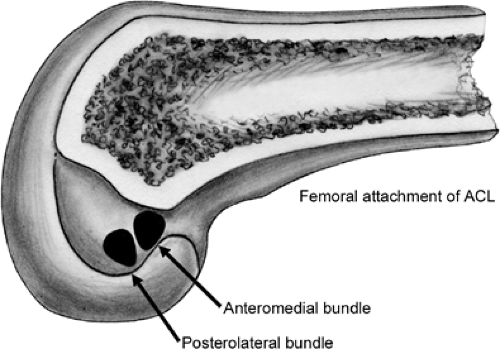
The anterior cruciate ligament (ACL) is a two-bundle ligament with a small isometric attachment to the tibia and femur (Fig 33-3). The cross sectional area of the ACL is approximately 35 mm2 and the average length is 25 mm. The tension in the two bundles varies with knee flexion; the anteromedial is tight in flexion and the posterolateral tight in extension. The tibial insertion is an oval attachment between the two spines of the tibia (Fig 33-4). The insertion sites are larger in cross sectional area than the midportion of the ligament. The insertion site on the femur is also oval in the posterior aspect of the medial wall of the lateral femoral condyle at the 1 to 3 o’clock position in the left knee, and 9 to 11 o’clock position in the right knee (Fig 33-5).
The Posterior Cruciate Ligament
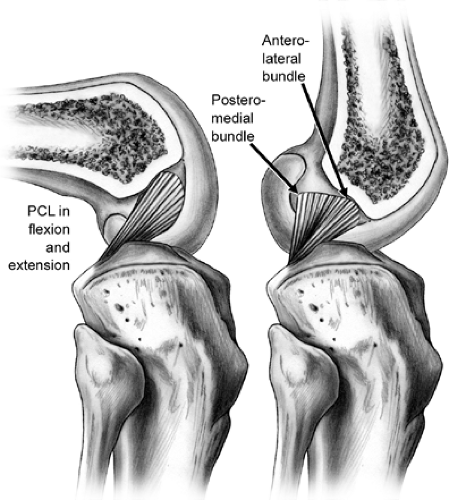
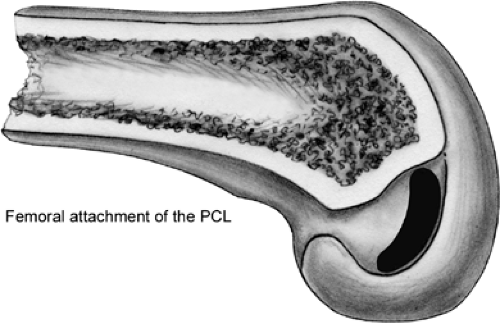
The PCL is also a two-bundle ligament with a small central isometric point on the femur (Fig 33-6). The PCL has an average intra-articular length of 4 cm, and the cross sectional
area is smaller in the middle compared to the femoral attachment site. The two bundles vary in tension with knee flexion, the anterolateral is tight in flexion and the posteromedial is tight in extension. The PCL insertion on the femur is a board insertion from the top of the intercondylar notch at the edge of the articular surface extending approximately 3 cm inferior (Fig 33-7). The insertion of the PCL on the tibia is slightly lateral, and 1 to 2 cm below the joint line (Fig 33-8).
area is smaller in the middle compared to the femoral attachment site. The two bundles vary in tension with knee flexion, the anterolateral is tight in flexion and the posteromedial is tight in extension. The PCL insertion on the femur is a board insertion from the top of the intercondylar notch at the edge of the articular surface extending approximately 3 cm inferior (Fig 33-7). The insertion of the PCL on the tibia is slightly lateral, and 1 to 2 cm below the joint line (Fig 33-8).
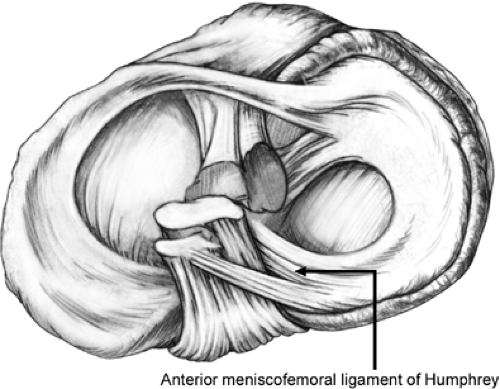
The Meniscal Femoral Ligaments
The meniscofemoral ligaments are present in most knees, but their true function is unknown. The meniscofemoral ligaments comprise up to one third the cross sectional area of the total PCL volume. The anterior meniscofemoral ligament of Humphrey crosses obliquely the distal aspect of the PCL when the knee is flexed (Fig 33-9).
The ligament of Humphrey attaches to the femur in front of the PCL, and is superficial when viewed in the flexed knee. It is attached to the femur immediately adjacent to the articular cartilage, in the 2 to 3 o’clock position, in a right knee. The distal attachment is to the posterior horn of the lateral meniscus. When the PCL is viewed arthroscopically, the anterior meniscofemoral ligament may be
identified by the oblique orientation of its fibers, in contrast to the vertical orientation of the PCL fibers.
identified by the oblique orientation of its fibers, in contrast to the vertical orientation of the PCL fibers.
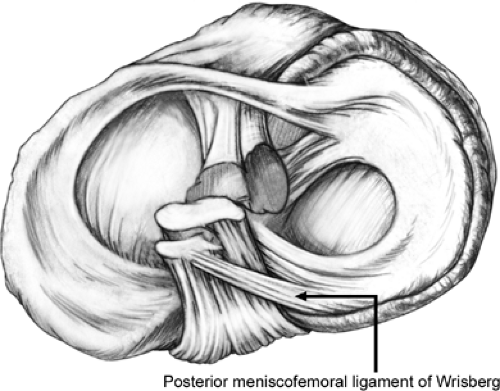
The posterior meniscofemoral ligament of Wrisberg runs from the medial side wall of the femoral notch to the posterior horn of the lateral meniscus (Fig 33-10). The femoral attachment is proximal to the posteromedial fibers of the PCL, and so, it is superficial to the PCL when viewed from the posterior aspect. It is on the posterior/superior aspect of the surface of the PCL. In order to make a positive identification of the posterior meniscofemoral ligament, it should be noted that it attaches directly to the posterior horn of the lateral meniscus, whereas the oblique posterior fibers of the PCL pass down to the posterior rim of the tibial plateau. The two meniscofemoral ligaments form a sling around the PCL.
The Medial Collateral Ligament
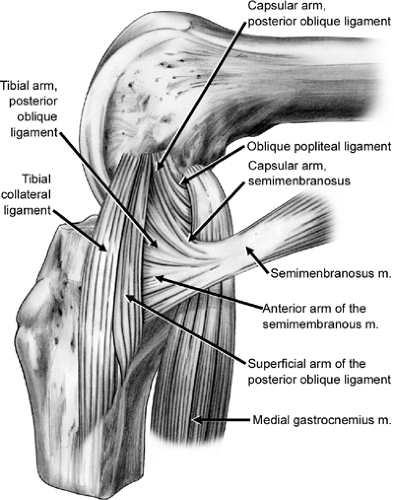
The medial supporting structures of the knee are divided into static and dynamic stabilizers. The pes anserinus muscles (sartorius, gracilis, and semimembranosus muscles) are flexors and internal rotators of the knee, which act as dynamic stabilizers. The semimembranosus is a stabilizer of the posteromedial corner, having insertions which provide capsular reinforcement along tibial and popliteal insertion. In addition, the vastus medialis obliquitous attaches to the adductor tubercle, and is associated with the tibial attachment of the MCL.
The static stabilizer is the capsuloligamentous complex. The MCL is a broad ligament (10 to 12 cm in length) that attaches to the medial femoral epicondyle and to the medial aspect of the tibia under the pes anserinus muscles, 4 cm below the joint line. The anterior fibers of the ligament tighten during knee flexion. The capsular tissue is reinforced by the vastus medialis anteriorly. In its middle one third of the capsule consists of meniscofemoral, meniscocapsular, and meniscotibial portions that lie under the deep MCL. Hughston and Eilers (1) have described the posterior portion of the capsule as the posterior oblique ligament (POL). This complex, which is tense in extension and loose in flexion, forms a sling around the posterior aspect of the medial femoral condyle and becomes confluent with the posterior capsule of the knee (Fig 33-11).
The Posterolateal Corner
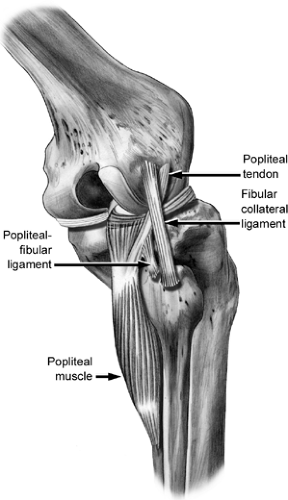
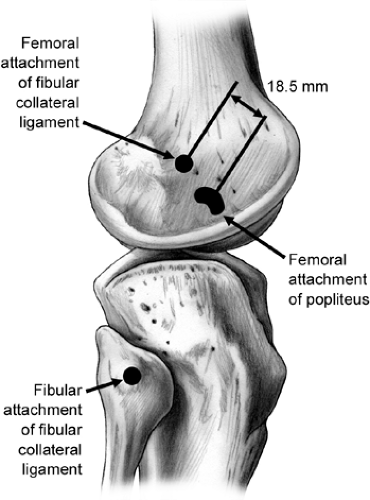
The lateral side of the knee is composed of the iliotibial band, the lateral collateral ligament (LCL), the fabellofibular ligament, the arcuate ligament, the popliteus tendon, the popliteal-fibular ligament and the capsule (Fig 33-12).
The iliotibial band is the most superficial and inserts on Gerdy’s tubercle. The LCL runs from the lateral epicondyle of the femur to the head of the fibula, and blends with the insertion of the biceps tendon.
The fabellofibular ligament is between the lateral ligament and the arcuate ligament. The arcuate ligament is a variable condensation of the posterior capsule. The popliteus tendon originates from the popliteus muscle on the back of the tibia, and wraps around the posterior aspect to insert just anterior to the epicondyle of the femur (Fig 33-13). The popliteal-fibular ligament connects the tendon to the posterior aspect of the head of the fibula. The popliteus tendon arises below the LCL in a small sulcus on the lateral femoral condyle, passes under the LCL, descends into the popliteus hiatus, then passes under the arcuate ligament, and becomes extra-articular before finally joining its muscle belly.
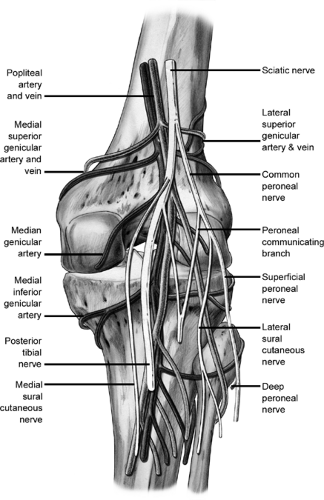
The neurovascular structures, popliteal artery and vein, and popliteal nerve lie between the heads of the gastrocnemius muscle (Fig 33-14). The artery is slightly lateral, and lies directly behind the posterior horn attachment of the lateral meniscus. The nerve and artery can be retracted laterally with the medial head of the gastrocnemius to approach the PCL and the posterior aspect of the joint.
Meniscus
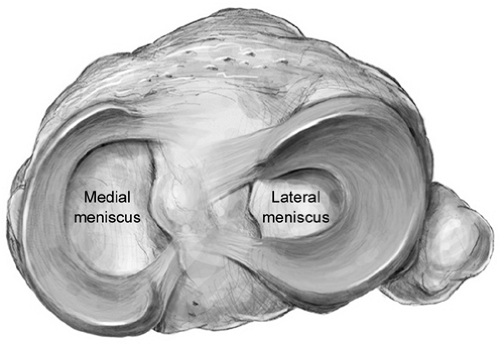
The medial and lateral meniscus are concentric lamellae that serve to deepen the tibial contact of the tibia, and provide stability to the femur (Fig 33-15).
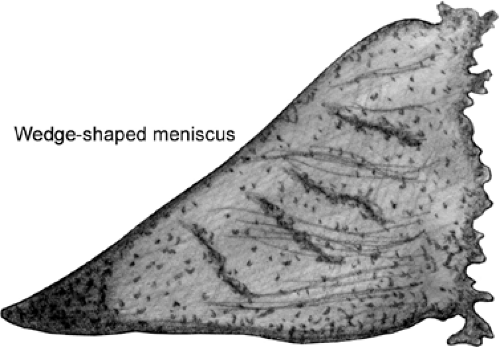
The peripheral border of the meniscus is thick and wedge shaped with attachments to the capsule. The medial meniscus is 3.5 cm in length and is thicker posteriorly than anteriorly (Fig 33-16). It is attached to the posterior aspect of the tibia. The anterior attachment is variable, and in some cases, has no bony attachment. The transverse ligament is a variable structure that connects the anterior medial to the anterior lateral meniscus. There is less anterior to posterior motion of the medial meniscus on range of motion of the knee.
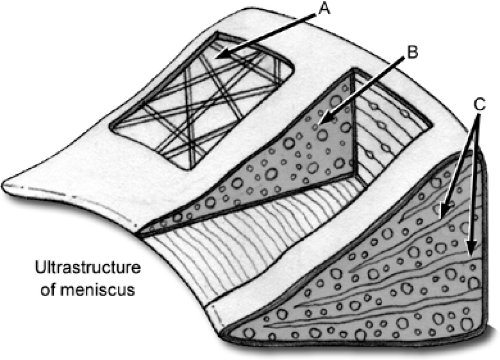
The composition of the meniscus is: 75% water, 20% collagen (Type I 90%, Type II, III, V, VI 3%), proteoglycans, noncollagenous proteins, lipids, and 2% cells (fibrochondrocytes, fibroblasts, mast cells, myofibroblasts). The collagen ultra-structure of the meniscus is composed of fine random fibers-A, the main bundle of circumferential fibers-B, and small radial fibers-C to reinforce the structure (Fig 33-17).
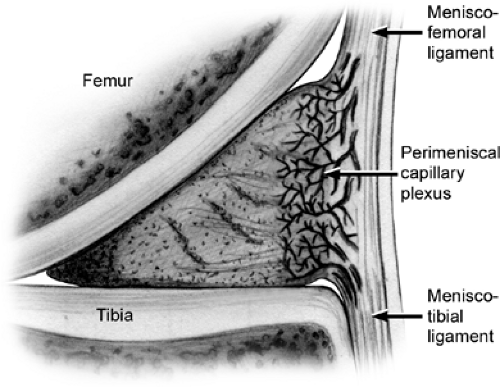
The outer one third of the meniscus is vascular, and thus has more potential to heal. This vascularity persists into adulthood (Fig 33-18). The lateral meniscus is larger, and has more motion as the knee flexes. The lateral meniscus is attached posterior to the tibia and to the meniscal femoral
ligaments. On the lateral aspect, the popliteus tendon leaves an open hiatus in the attachment of the meniscus.
ligaments. On the lateral aspect, the popliteus tendon leaves an open hiatus in the attachment of the meniscus.
Articular cartilage is a thin layer of specialized connective tissue lining the articulations of diarthrodial joints. Properties which are unique to this tissue enable an almost frictionless joint movement and afford protection to the underlying bone from excessive load and trauma by dissipating the forces produced during movement.
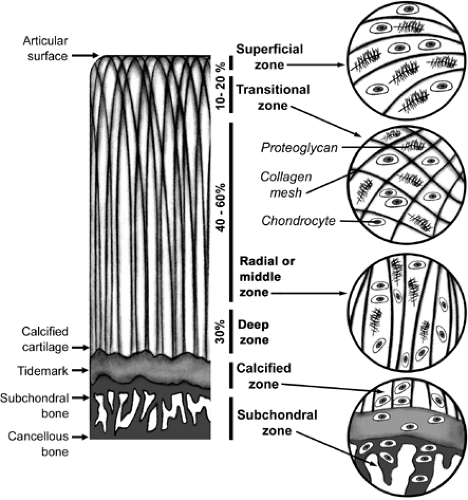
The structural organization of articular cartilage can be divided into four major zones: superficial, middle, deep, and calcified zones (Fig 33-19). Each zone is distinctly structured with cells and extracellular matrix (ECM) organized in specific patterns. The cells, known as chondrocytes, make up 1% to 2% of the total weight of the articular cartilage. On
the other hand, the ECM, which makes up the rest of the cartilage, is generally composed of Type II collagen, glycoaminosglycans, and proteoglycans.
the other hand, the ECM, which makes up the rest of the cartilage, is generally composed of Type II collagen, glycoaminosglycans, and proteoglycans.
Tendons and ligaments are tissues with unique biomechanical properties. Tendons have adequate strength to sustain the high tensile forces during muscle contraction, yet have adequate compliance to angulate around bone surfaces and move underneath retinacula to vary the direction of muscle tension. Ligaments are supple, permitting natural movements of bones to which they attach, yet are strong in providing resistance to external forces to a joint.
The function of tendons is to attach muscle to bone and produce joint motion via the transfer of forces from muscular tensile forces to bone. Tendons also permit the muscle belly to be at an ideal distance from the joint it acts on to prevent an excessive muscle length between origin and insertion.
The role of the ligaments and joint capsules is to increase the mechanical stability of the knee joint, guide normal kinematics or joint motions, and to prevent excessive joint motion, which may damage articular cartilage and menisci. These structures play an integral role in knee joint motion even though they are passive (i.e., they do not actively produce joint motion).
Tendons and ligaments are primarily composed of collagen, a fibrous protein, giving them great strength and flexibility. Ligaments are poorly vascularized and generally have 75% collagen composition somewhat less than tendons (2). The orientations of the parallel collagen fibers help determine the biomechanical behavior of the individual knee ligaments. Collagen fibrils in the joint capsule are less parallel than ligaments, resulting in increased compliance, but decreased resistance to linear forces. Since the biochemical composition of tendons and ligaments of humans are identical to some other species such as rabbits and dogs, a significant amount of research on tissue biomechanics has been applied from these animal studies.
In the knee, the ligaments are the most important static stabilizer of the joint. The knee ligaments’ role is to stabilize the knee, prevent abnormal kinematics, and any abnormal displacements that may damage the articular cartilage. There are four zones pertaining to the insertion of ligaments into bone (this also applies to tendons).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree