Chapter 4. Basic science in orthopaedics
By the end of this chapter you should be able to:
• Understand the general principles of joint lubrication and biomechanics.
• Understand the different types of implant used to fix fractures and orthopaedic conditions and their complications.
• Understand the different types of metals used.
• Have a clear understanding of how fractures heal.
Biomechanics
An understanding of the way the body works as a machine is essential to an orthopaedic surgeon but mechanical considerations must always come second to the clinical assessment of the individual patient. The temptation to regard the patient as a machine must be resisted; people are not machines, even if the body is.
Joint loading
The loads imposed on the joints and the direction of the forces in which they act are not always obvious from gross anatomy (Fig. 4.1a). The load across the hip, for example, is the resultant of the patient’s weight acting downwards and muscles pulling the femur medially and upwards at an angle of about 16° from the vertical. This should not be a surprise because the bone trabeculae in the femoral neck and ilium are oriented in the same direction (Fig. 4.1b). According to Wolff’s law, which states that the position of the trabeculae is dictated by the forces acting on the bone, the trabeculae are the ‘materialized trajectory of the force’.
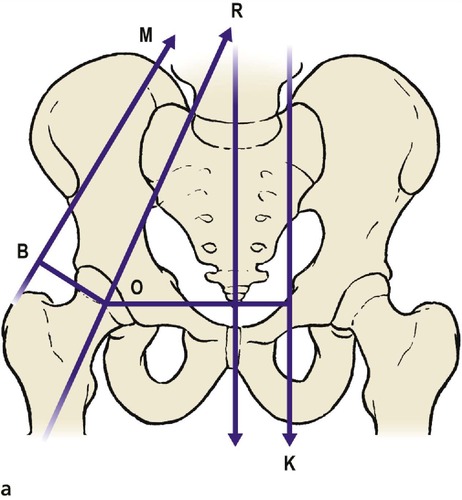 |
| Fig. 4.1a Vectors acting at the hip joint. |
 |
| Fig. 4.1b Radiograph of the pelvis to show that the trabeculae are arranged according to the line of weight transmission and follow Wolff’s law. |
When standing on one leg, the abductors act at a mechanical disadvantage because they are nearer the centre of the hip joint than the patient’s centre of gravity (L1). In consequence, they have to lift about three times body weight and the load across the hip joint is correspondingly increased. Because loading a diseased hip is painful, it is useful to reduce the load across the hip by allowing the abductor muscles to work at a greater advantage. Patients need no biomechanical knowledge to walk with an antalgic (pain-relieving) gait and quickly find that leaning the body to the side of the affected hip is less painful than walking upright because it brings the centre of gravity closer to the fulcrum and reduces the load across the joint (Fig. 4.2).
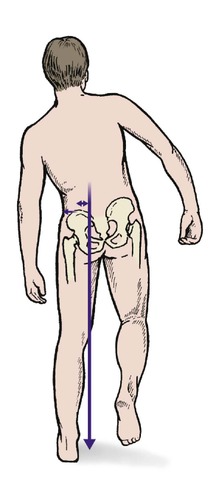 |
| Fig. 4.2 Antalgic gait tilting the pelvis reduces the load on the joint and thus the pain (see also Fig. 2.35). |
Muscles act at a mechanical disadvantage in other joints as well. The elbow and knee both have flexors and extensors so close to the axis of rotation that they must contract with a force several times greater than the weight they are lifting.
Joint lubrication
Calculations of the shear stresses on a joint surface show, among other things, that the patella has a greater shear stress imposed upon it than any other bone – seven times body weight.
Joint lubrication is complex and depends on three mechanisms (Fig. 4.3).
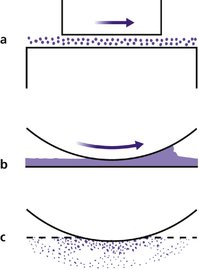 |
| Fig. 4.3 Different types of lubrication: (a) boundary lubrication; (b) surface lubrication; (c) boosted lubrication. |
Boundary lubrication
Boundary lubrication depends on molecules sliding over each other and is best for heavy loads and slow movements. Graphite is a boundary lubricant. The large hyaluronic acid-based proteoglycan molecules in synovial fluid function in the same way.
Surface lubrication
Compounds which flow between surfaces, such as oils, are the best known lubricants. Synovial fluid acts as a surface lubricant and its efficiency is increased by the ‘wedge effect’. The joint surfaces are not a perfect fit and the irregularities create a wedge of fluid at the point of contact, a little like a car ‘hydroplaning’ on a wet road.
‘Boosted’ lubrication
To improve lubrication still further, fluid from the articular cartilage is squeezed out when it is compressed. This is ‘boosted’ lubrication.
Implants
It is often necessary to insert plates, screws, prostheses and other devices in the body and much effort goes into implant materials and design. It was not always so; in the early days of internal fixation, ordinary wood screws were used to fix fractures but these were specifically designed for timber and proved unsuitable for bone. Not only did the screws rust but a wood screw, which is tapered and ideal for a fibrous material like wood, cannot be used on a dense material like cortical bone. Different types of screws, threads and bone are dealt with on page 133.
Stress risers
Bones are more flexible than metal plates. Screwing a metal plate to bone stiffens it and produces a ‘stress riser’ at each end, which can cause a fracture at the end of the plate (Fig. 4.4).
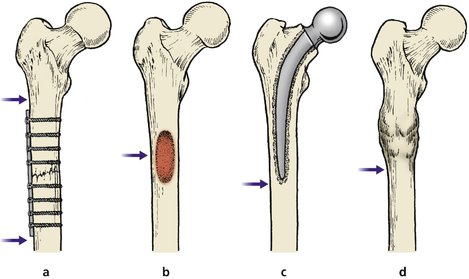 |
| Fig. 4.4 Stress risers. Bones may break at the junction of areas of differing stiffness: (a) upper and lower limits of internal fixation device; (b) tumour; (c) lower limit of hip prosthesis; (d) above or below a united fracture. |
Similar problems arise around joint prostheses. Not only do fractures occur immediately below the tip of the femoral component of a total hip replacement ( THR), but the different stiffnesses of the bone and implant mean that the interface between the two is under strain. Attempts have been made to overcome this problem by developing ‘isoelastic’ implants with the same elasticity as bone.
Holes
Drilling a hole through bone also produces a stress riser by weakening the bone, but a hole filled with a screw weakens it much less. These considerations only concern orthopaedic surgeons but it is important to appreciate that there is more to reconstructive surgery than the layman supposes.
Materials
Many materials have been used for implants, and most have proved unsatisfactory (Fig. 4.5). The salts of the constituent metals are slowly leached out of the implant over the years and some are toxic or allergenic. The ideal material must be insoluble, strong, non-toxic, non-carcinogenic, and also non-irritant in particulate form.
 |
| Fig. 4.5 An early implant. The metal was not truly inert and the screws have corroded. |
Metals
Stainless steel, perhaps the simplest implant material, contains a cocktail of different elements and is generally satisfactory, although not as strong as chrome, cobalt and molybdenum alloys of which many implants are made (Table 4.1). Prostheses are also made of almost pure titanium. Precious metals such as silver and gold are satisfactory implant materials but lack the strength required of a prosthesis, quite apart from their cost.
| Stainless steel (%) | Chrome/cobalt (%) | Titanium alloy (%) | |
|---|---|---|---|
| Iron | 62.2 | ||
| Chromium | 21.5 | 28 | |
| Nickel | 9 | ||
| Manganese | 4 | ||
| Molybdenum |









