Autologous Chondrocyte Transplantation
Markus Walther
DEFINITION
There are several reasons for cartilaginous defects of the ankle:
Traumatic injury
Osteochondritis dissecans (OCD)
Degenerative changes
The necessity to treat a cartilage defect of the ankle depends on the clinical presentation. Osteochondral lesions of the talus (OLTs) are often found incidentally on screening magnetic resonance imaging (MRIs) obtained for reasons other than suspected intra-articular pathology.
Autologous chondrocyte transplantation (ACT), also known as autologous chondrocyte implantation (ACI), is one of several surgical treatment options for symptomatic cartilage defects. In my opinion, ACI is best suited for patients between 18 and 50 years of age.
ACI is indicated for management of symptomatic OLTs failing to respond to débridement, drilling, or microfracture.1,9,34
Primary ACI can be considered in lesions larger than 2 cm2 or in osteochondral lesions associated with expansive subchondral cysts (stage V lesion).57
Advantages of ACI include the following:
ACI provides a stable cartilage rim that can be maintained at the site of the OLT.
Large defects can be readily addressed with this technique.
The periosteal flap can be harvested from the adjacent medial tibia.
With carefully executed suture technique or with matrixinduced chondrocytes, shoulder lesions can be managed.
Disadvantages of the ACI for the talar dome are as follows:
ACI has Food and Drug Administration (FDA) approval only for the knee. ACI at the talus as well as matrixinduced autologous chondrocyte implantation (MACI) is considered investigational (as of January 2015).
The cost from industry for chondrocyte culture is considerable.
The procedure requires two stages to allow time for chondrocyte culture.
Reports of the traditional technique that requires a periosteal flap under which the transplanted chondrocytes are positioned suggested limitations of the technique for the talus.54 Many OLTs involve, at least in part, the talar shoulder, an anatomic region poorly suited for anatomic coverage with a periosteal flap. Recently introduced MACI may afford advantages because it does not require coverage of the defect with a periosteal flap. Histologic investigations have shown that MACI may offer an improved alternative to traditional treatments for cartilage injury by regenerating hyaline-like cartilage.57
Informed consent and patient education are imperative for ACI. ACI for the ankle lacks FDA approval. However, for larger OLTs, OLTs failing to respond to prior surgical management, or OLT with subchondral cysts, ACI provides patients and their surgeons with a potentially successful treatment avenue that did not exist before ACI. Early favorable outcomes with ACI applied to difficult OLTs justify the extra effort, education, and communication among physicians, patients, and third-party payers that may be required to proceed with ACI in the ankle.
In Europe, harvesting cells for culturing is considered part of a drug-producing process. Therefore, special permission must be sought from the local health care administration. Standard operating procedures for harvesting and transportation of the cartilage cells are mandatory for the accreditation process.
Latest developments focus on one-step, membrane-based, scaffold-enhanced cartilage repair. Mesenchymal progenitor cells migrate toward and adhere to the porous layer of the matrix which is implanted analogue to the technique described in the following text in a one-step surgery. Whereas in Europe, different membranes are approved for use in the talus, the FDA approval is still in progress.13,24,52,55
ANATOMY
Sixty-two percent of lesions are located at the medial talar shoulder; many of these are thought to be a result of OCD rather than posttraumatic.
Thirty-four percent of the lesions are located at the lateral talar shoulder; most are thought to be of traumatic origin.
Central OLTs are rare (<5%).
In the anteroposterior (AP) direction, the midtalar dome (equator) is much more frequently involved (80%) than the anterior (6%) or posterior (14%) thirds of the talar dome.
Classification of osteochondral lesions is based on arthroscopic findings.28
Grade I: intact lesions
Grade II: lesions showing signs of early separation
Grade III: partially detached lesions
Grade IV: craters with loose bodies
ACI is performed for symptomatic grade II-plus lesions (fullthickness cartilage defects).
PATHOGENESIS
Traumatic cartilage injuries are caused by short, intensive, greater-than-physiologic strain on the joint resulting in partial detachment of the talar dome cartilage. The depth of these lesions varies from superficial chondral abrasions to full-thickness osteochondral defects.39,51
OCD is a condition most frequently found in adolescents or young adults. Although the cause remains poorly defined, theories include the following:
Chronic overload
Local disturbance of blood supply to the subchondral bone associated with the affected cartilage32
Degenerative cartilage defects (degenerative osteoarthritis) develop from wear and tear of the cartilage surface as part of the aging process. An individual’s risk of developing primary osteoarthritis most likely depends on a genetically determined quality of the cartilage. Ankle instability and other conditions that impart eccentric or nonphysiologic loads to the cartilage may accelerate the process of degeneration. In exceptional cases, when such a degenerative process is limited to a focal portion of the talar dome, ACI may be considered for degenerative cartilage defects, provided the underlying cause leading to focal degeneration (ie, malalignment or chronic instability) is corrected.
NATURAL HISTORY
The natural history of a focal cartilage injury has not been linked to diffuse ankle arthritis.
Posttraumatic arthritis, which differs from an OLT, develops from diffuse injury to the cartilage surface that results in cartilage fibrillation and eventual eburnation. ACI is contraindicated for diffuse ankle arthritis.
Injury to a focal portion of the talar dome spans the spectrum from a bone bruise to a detached focal osteochondral fragment. Although an osteochondral fragment may be created at the time of injury, the focal talar dome pathology probably evolves. Many OLTs are probably asymptomatic; we know this from numerous OLTs that are found incidentally on imaging studies of the ankle obtained for reasons other than suspected intra-articular pathology. However, with persistent eccentric stresses, greater-than-physiologic loads, inadequate local blood supply, or inadequate healing time, a stable OLT may progress to an unstable one.
The difficulty is also in the symptomatology. Although some apparently unstable lesions may be asymptomatic, other OLTs that are clearly stable result in considerable symptoms directly related to the OLT.35
PATIENT HISTORY AND PHYSICAL FINDINGS
Although many patients report a specific ankle injury to account for the OLT, many do not present until months after ankle injury.14 A symptomatic OLT is in the differential diagnosis for an ankle sprain that does not heal. However, many patients with symptomatic OLTs do not recall a specific traumatic event leading to the OLT.46
In my experience, most patients presenting with symptomatic OLTs are between 20 and 50 years of age.52
Men are more commonly affected than women (ratio 1.6:1).46
Patients typically describe an ache in the ankle with activity or with the first steps after a period of rest. Occasionally, sharp ankle pain is noted with weight bearing. In our experience, mechanical symptoms of locking or catching are noted only with a completely detached osteochondral fragment. Paradoxically, OLTs may produce symptoms on the opposite side of the joint from the location of the cartilage defect.
Our preferred physical examination methods are listed here. Occasionally, symptoms may not be elicited on clinical examination.
Locking or catching: found when something interrupts the normal movement of the joint. However, it says nothing about the cause of this condition (eg, scar, joint body, osteochondral fragment, and synovitis).
Inversion test (calcaneofibular ligament [CFL]): strongly dependent on the cooperation of the patient. If positive, it is highly specific for a ruptured CFL.
Medial stability: strongly dependent on the cooperation of the patient. If positive, it is highly specific for a ruptured deltoid ligament.
Anterior drawer test (anterior talofibular ligament [ATFL]): strongly dependent on the cooperation of the patient. If positive, it is highly specific for a ruptured ATFL.
The medial and lateral corner of the talar dome should be palpated with the ankle maximally flexed to identify anterior or central OLTs; posteromedial palpation immediately posterior to the posterior tibial tendon (PTT) with the ankle maximally dorsiflexed may reproduce symptoms for posteromedial OLTs. Although anterolateral OLTs are relatively easy to palpate, posteromedial lesions are difficult to access adequately on physical examination.
We find it useful to compare the symptomatic ankle to the uninvolved contralateral ankle.
The medial and lateral corner of the talar dome should be palpated with the ankle maximally flexed to identify anterior or central OLTs; posteromedial palpation immediately posterior to the PTT with the ankle maximally dorsiflexed may reproduce symptoms for posteromedial OLTs. Although anterolateral OLTs are relatively easy to palpate, posteromedial lesions are difficult to access adequately on physical examination.
We typically dorsiflex and plantarflex the ankles with axial pressure while simultaneously applying eversion and inversion stresses to reproduce symptoms at the talar defect.
Despite appropriate provocative maneuvers, our experience has been that posterior OLTs rarely exhibit obvious clinical findings.
Associated injuries and other considerations in the differential diagnosis of chronic ankle pain should be evaluated, particularly because OLTs may be incidental findings. These include the following:
Ankle instability: positive anterior drawer test and inversion testing
Chondromatosis of the ankle: Recurrent locking of the joint and persistent effusions are typical physical findings.
Intra-articular scarring with load-dependent pain, mostly at the anterolateral aspect of the ankle joint
Inflammatory arthropathy: Although effusion and deep joint pain with weight bearing are commonly present, pain at rest and persistent joint warmth are also common features of inflammatory disease.
Pigmented villonodular synovitis (PVNS): Organized nodules of synovitis can mimic loose bodies with locking and effusion. Synovial swelling is not typical for osteochondral defects. MRI with contrast typically confirms the diagnosis of PVNS.
Hindfoot malalignment with local osteoarthritis: Edge loading of the talus can cause symptomatic local cartilage lesions. Typically, those defects include the tibial cartilage as well as the talus, which can be visualized with MRI.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs of the ankle joint, including AP, mortise, and lateral views, are obtained to rule out late-stage degenerative arthritis.
MRI with contrast is highly sensitive and specific in diagnosing osteochondral lesions as well as associated injuries.30,41
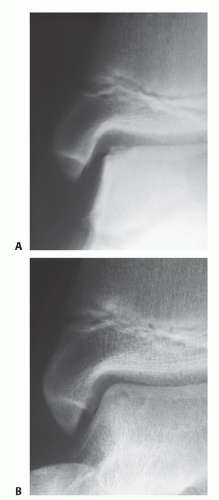
Osteochondral lesions were first classified by Berndt and Harty8 based on plain radiographs:
Stage I: compression lesion; no visible fragment
Stage II: beginning avulsion of a chip
Stage III: chip, completely detached but in place
Stage IV: displaced chip
Plain films typically offer limited information on the size and extent of the lesion and may even miss the OLT. MRI, computed tomography (CT), and arthroscopic evaluation provide greater detail of OLTs than plain radiographs.
DiPaolo classification of osteochondral lesions based on MRI15
Stage I: thickening of articular cartilage and low signal changes
Stage II: articular cartilage breached, low signal rim behind fragment indicating fibrous attachment
Stage III: articular cartilage breached, high signal changes behind fragment indicating synovial fluid between fragment and underlying subchondral bone (FIG 1)
Stage IV: loose body
Based on the greater detail of pathologic anatomy, Hepple et al30 revised the classification and included a stage V (subchondral cyst formation).
Stage I: articular cartilage damage only
Stage IIa: cartilage injury with underlying fracture and surrounding bony edema
Stage IIb: stage IIa without surrounding bony edema
Stage III: detached but undisplaced fragment
Stage IV: detached and displaced fragment
Stage V: subchondral cyst formation
The Ferkel and Sgaglione CT classification is used for preoperative planning purposes and to learn the size of the subchondral defect.20
Stage I: cystic lesion of the talar dome with an intact roof
Stage IIa: cystic lesion with communication to the talar dome surface
Stage IIb: open articular surface lesion with an overlying, nondisplaced fragment
Stage III: nondisplaced lesion with lucency
Stage IV: displaced osteochondral fragment
DIFFERENTIAL DIAGNOSIS
Syndesmosis injury
Intra-articular scarring
Subluxation or tear of peroneal tendons
Fracture or disruption of the os trigonum
Malleolar avulsion fracture
Interosseous ligament injury
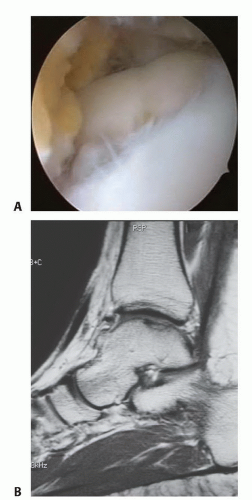
FIG 1 • A. Arthroscopic view of a full-thickness osteochondral defect at the talar dome. B. Corresponding MRI.
Anterior process fracture of the calcaneus
Lateral shoulder fracture of the calcaneus
Chondromatosis
Inflammatory joint disease
PVNS
Degenerative arthritis
NONOPERATIVE MANAGEMENT
In young patients with open physes, OCD can be managed conservatively with a high rate of complete remission (FIG 2).7,53
Acute osteochondral lesions may be treated conservatively. Acute lesions (stages I and II) require 3 weeks of immobilization. Stages III and IV lesions should be treated with a walker and partial weight bearing of 20 kg for 6 weeks.46 However, unstable osteochondral lesions, particularly those with detached fragments, should be managed operatively.
Incidentally discovered OLTs and OCD cases in adults are generally treated expectantly with regular follow-up.17,53
The literature suggests that chronic OLTs, even larger lesions, may be treated nonoperatively as well.49 Nonoperative treatment comprises nonsteroidal anti-inflammatory agents, ankle bracing, physiotherapy, corticosteroid injection, and viscosupplementation. Currently, no conservative treatment of OLTs allows resurfacing or healing of the cartilage defect.
SURGICAL MANAGEMENT
Microfracture
Arthroscopic débridement and microfracture generally represent the initial surgical management for the vast majority of OLTs, with satisfactory results in 65% to 90% of patients.6,31,45
After arthroscopic débridement of the OLT, the defect’s subchondral bone is penetrated with multiple noncontiguous passes of a specialized awl to permit the débrided defect to be populated with undifferentiated stem cells from the deeper tissues.
Over the next few months, these cells reorganize into (type II) fibrocartilage.
The biomechanical properties of fibrocartilage are different from those of hyaline cartilage; the fibrocartilage does not function in concert with the surrounding physiologic hyaline cartilage. The literature suggests that microfracture is successful in a majority of relatively small OLTs (up to 2 cm2).6,25
Autologous osteochondral transfer (osteochondral autograft transplantations [OATS] or mosaicplasty) and ACI are typically secondary surgical procedures when arthroscopic débridement and microfracture and drilling fail.
Due to inferior outcome of microfracture in OLTs larger than 2 cm2, ACI can be considered as primary surgery in large defects.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree