Athlete with Shortness of Breath
Joseph J. Bernard
Zachary A. Geidel
INTRODUCTION
Shortness of breath is a common complaint in athletes and is a frequent reason for the athlete to seek medical attention. The potential etiologies range from benign deconditioning to serious cardiac or pulmonary disorders. Cardiac conditions that can cause shortness of breath in the athlete are covered in Chapter 3. The focus of this chapter will be on two common and similar pulmonary conditions: exercise-induced asthma (EIA) and exercise-associated bronchospasm (EAB). In addition, overtraining syndrome and anemia will be reviewed as causes for shortness of breath in the athlete.
PATHOPHYSIOLOGY
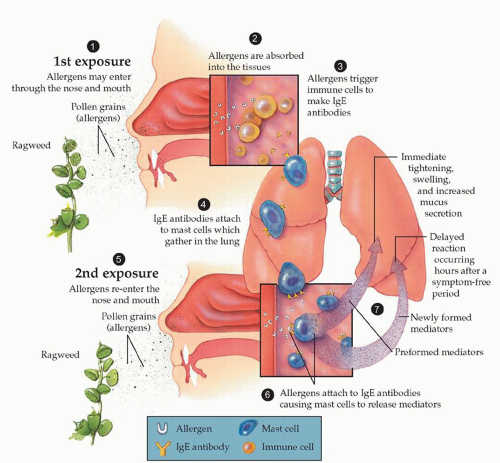
Asthma is a reversible condition of the tracheobronchial tree commonly encountered in children and young adults. The key clinical features include hyperresponsiveness that results in reversible narrowing of the airways. In 1995, the National Heart, Lung, and Blood Institute’s “Global Initiative for Asthma” developed the following definition for asthma (Fig. 4.1):
“Asthma is a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role, in particular, mast cells, eosinophils, T lymphocytes, macrophages, neutrophils, and epithelial cells. In susceptible individuals, this inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning. These episodes are usually associated with widespread but variable airflow obstruction that is often reversible either spontaneously or with treatment. The inflammation also causes an associated increase in the existing bronchial hyperresponsiveness to a variety of stimuli.”1
Asthma is an inflammatory disorder of the airways involving several different inflammatory cells and mediators (Fig. 4.2). The inflammatory response causes characteristic structural changes in the airway, including an increase in airway smooth muscle. Subsequent airway narrowing results in the symptoms associated with asthma.
EIA is the transient narrowing of the airway in an athlete with chronic asthma following exercise or physical activity. EAB refers to bronchospasm in the athlete without the underlying findings of asthma. A key differentiation with asthma is the lack of significant inflammation as the underlying etiology seen in EAB.
There are two current theories on the underlying pathophysiology of EAB. The first is the airway rewarming theory, which postulates that hyperventilation in exercise leads to cooling of the airways. Upon cessation of exercise, small bronchiolar vessels dilate and become congested with the rewarming of the airways. This results in leakage into the submucosa of the airway walls stimulating bronchoconstriction.2,3
The second mechanism, the hyperosmolarity theory, proposes that during hyperventilation with exercise, there is water loss from the airway surface leading to hypertonicity and hyperosmolarity within the airway cells. Subsequently, mediators are released causing bronchoconstriction.2,4 There is also some evidence that inflammation of the airway may be involved, similar to chronic asthma.2
A key component of normal lung function is the proper gas exchange at the alveolar level. Conditions that affect this process limit oxygenated blood from reaching the muscles and end organs. The affect on the gas exchange can result in clinical manifestations of performance decline, fatigue, and shortness of breath.
Key to the role of gas exchange is the hemoglobin molecule. In humans, the hemoglobin molecule is an assembly of four globular protein subunits. Each subunit is composed of a protein chain tightly associated with a nonprotein heme group. The heme group consists of an iron (Fe) atom held in a heterocyclic ring. The iron atom is the site of oxygen binding. Hemoglobin serves as the iron-containing oxygen transport system in red blood cells (RBCs). It transports oxygen from the lungs to the rest of the body, such as to the muscles, where it releases the oxygen load. Therefore, low levels of hemoglobin may hinder athletic performance.
Anemia refers to lower levels of hemoglobin than what is expected, resulting in a drop in one’s hematocrit. Normal values for hemoglobin levels are as follows:
Women: 12.1 to 15.1 g/dL
Men: 13.8 to 17.2 g/dL
Children: 11 to 16 g/dL
The term “sports anemia” or “athlete’s anemia” is often used to refer to the lower levels of hemoglobin seen in the athletic population, especially in elite athletes. This is not a true anemia but a normal physiologic adaptation to exercise that results in increased plasma expansion.
In addition to dilutional anemia, other potential causes in athletes may include (1) excess destruction (i.e., foot strike anemia), (2) blood loss from gastrointestinal or genitourinary tract, and (3) decreased production (i.e., iron deficiency).
Other hematologic conditions that need to be considered in athletes include sickle cell disease/trait, in which abnormal hemoglobin is produced, or thalassemia, where there is a decrease in the production of normal hemoglobin chains.
The etiology of overtraining syndrome is controversial and an area of active research. Proposed pathophysiology includes the theory that an overactive pituitary gland is primarily responsible for physiologic responses to overtraining. This in turn results in elevated cortisol levels and added stress to the body’s natural response to intense work. There is also an increase in serum creatine kinase levels and it is proposed that the body is in a state of catabolism, breaking down protein and muscle for energy. Overtraining has also been associated with overuse injuries, most commonly posterior tibialis syndrome, lower limb stress fractures, and tendonitis. It is unclear if this is due to excessive high training loads or inability of the body to recover and repair damage from training. The body’s immune system is also compromised, possibly from decrease in C-reactive protein levels after intense exercise. Also it has been proposed that an acute phase response may occur in the overtrained athlete with leukocytosis, fever, decrease in copper and zinc levels, and increase in erythrocyte sedimentation rate (ESR). This in turn leads
to an increase in colds, allergic reactions, and other infections. Psychologic factors are also manifested in overtrained athletes but much more difficult to detect at times.5
to an increase in colds, allergic reactions, and other infections. Psychologic factors are also manifested in overtrained athletes but much more difficult to detect at times.5
EPIDEMIOLOGY
EIA is seen in 80% to 90% of individuals with underlying asthma; however, many athletes only have bronchospasm associated with exercise without underlying chronic asthma.6
There is a variable reported incidence of EIA or EAB in the literature with range of 7% to 20% in the general population.7,8 The variability appears to be related to the overall low quality of the studies, small numbers, and limited patient populations. Many studies have been done in certain subgroups, such as children, and in certain sports, such as figure skating and ice hockey. It is difficult to sort out which of these athletes only have bronchospasm associated with exercise and which have underlying chronic asthma. It does appear that certain sports are at higher risk for EIA or exercise-induced bronchospasm (EIB), including Nordic skiing, track and field, soccer, hockey, football, water polo, cycling, etc.
The incidence of anemia in the general public has been reported as 4% in males and 8% in females in the United States. The incidence of iron deficiency in premenopausal women has been found to be 4% to 8% in the United States. Regular nonprofessional sport activity does not cause an increased rate of anemia or of iron deficiency in fertile women. However, physical exercise has an impact on iron status, as it reduces serum iron and transferrin saturation and elevates soluble transferrin receptor. Nearly one-fifth of recreational athletes have anemia and one-third have iron deficit; these conditions can decrease their physical performance.9 Sickle cell disease in the United States is estimated to be around 1 in 625 persons at birth; however, in black Americans the sickle gene is present in approximately 8% of the population. This reaches upward of 30% in Africa.
NARROWING THE DIFFERENTIAL DIAGNOSIS
While an exhaustive differential of conditions that might result in an athlete with exercise-associated shortness of breath are beyond the scope of this chapter, common conditions to consider include the following:
EIA
EAB (without underlying chronic asthma)
Vocal cord dysfunction
Chronic obstructive pulmonary disease
Restrictive lung disease
Cardiovascular disorder
Upper/lower respiratory infection
Deconditioning
Anemia
Overtraining
Pneumothorax (spontaneous)
Pulmonary embolism
History
When evaluating an athlete with shortness of breath, a thorough history should be obtained regarding the length of symptoms, precipitating and alleviating factors, and other associated symptoms. A past medical history of asthma would certainly make the diagnosis of EIA more likely. If there have been other associated infectious symptoms such as fever, sinus congestion, or productive cough, a respiratory infection may be likely.
Evidence-based Physical Examination
A thorough examination should be performed with special focus on the cardiovascular and pulmonary examinations. Key components of the cardiovascular examination should include bilateral blood pressure testing, cardiac auscultation, and peripheral pulse palpation. Key components of the pulmonary examination should include auscultation for expiratory wheezing and prolonged expiratory phase as well as inspiratory stridor in addition to any audible rales or rhonchi.
Diagnostic Testing
Laboratory
If clinically indicated, a complete blood count could help rule out anemia. Further iron and hemoglobin studies may be considered based on complete blood count (CBC) result and clinical scenario, including an athlete with a microcytic anemia and particularly in females and those of Mediterranean decent. This would include serum iron, ferritin, transferrin, total iron binding capacity, reticulocyte count, and possibly hemoglobin electrophoresis.
Thyroid studies, LFTs, and renal function tests may be considered. Blood tests to consider in the athlete with overtraining include CBC, cortisol level, luteinizing hormone level, testosterone level, creatine kinase level, C-reactive protein, and ESR.
Imaging
If a lower respiratory infection or spontaneous pneumothorax is suspected, a chest radiograph may be considered. Appropriate imaging studies would be indicated for suspected pulmonary embolism.
Other Testing
If clinical scenario and examination suggest cardiac findings ECG, echocardiogram, and exercise stress tests may be considered. Appropriate indications for cardiac testing are reviewed in the Chapter 3.
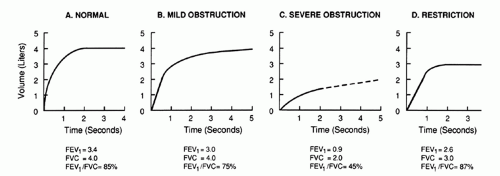
Pulmonary function tests (PFTs) are useful when looking for obstructive or restrictive lung disease. A full description of PFTs and spirometry are outlined in the following sections.
APPROACH TO THE ATHLETE WITH EXERCISE-INDUCED ASTHMA
HISTORY AND PHYSICAL EXAMINATION
Shortness of breath associated with exercise is usually the first complaint and will often prompt a workup for asthma. Athletes and coaches may have the misperception that the athlete is “just out of shape.” There is often a decrease in exercise endurance as well. Questions regarding chest tightness, coughing, or wheezing associated with sports participation should be asked. Any athlete with shortness of breath should be questioned with regard to a history of asthma or bronchodilator use.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree