Cerebral palsy is the most common motor disability in childhood. Orthopedic care depends on the appreciation and the identification of muscle tone abnormalities and how they affect growth and development of the child. Abnormal muscle tone is a common diagnostic feature of cerebral palsy and can include hypotonia or hypertonia. Hypertonia is the most frequent tone abnormality in children with cerebral palsy. This article reviews hypertonia and provides information on discriminating between spasticity, dystonia, and rigidity. Medication and neurosurgical options for the management of hypertonia are presented and compared.
Cerebral palsy is the most common motor disability in childhood. The management of children with cerebral palsy ideally involves a team of professionals, including physical therapists, occupational therapists, physiatrists, developmental pediatricians, and an orthopedic surgeon with clearly identified areas of expertise. The pediatric orthopedic surgeon manages contractures and alignment. Cerebral palsy was first described in 1843 by an orthopedic surgeon named William John Little. Since then, pediatric orthopedic surgeons have contributed to prognosis, management, and development of new treatments that promote improved function in the population with cerebral palsy.
Orthopedic care depends on the appreciation and identification of muscle tone abnormalities on the overlay of the growth and development of the child. Abnormal muscle tone is a diagnostic feature of cerebral palsy. Abnormal tone includes hypotonia and hypertonia. Frequently, both exist in the child. Hypertonia is the most frequent tone abnormality appreciated in the extremities of children with cerebral palsy.
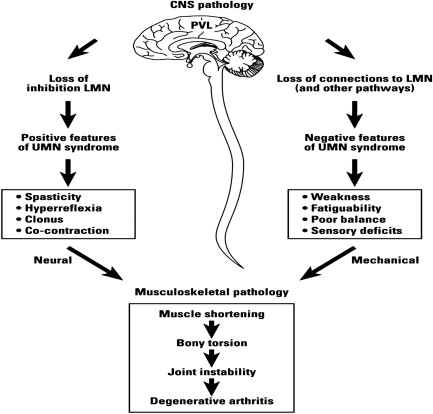
Hypertonia is caused by the upper motor neuron syndrome. The cascade of problems or impairments associated with the upper motor neuron syndrome is divided into negative and positive symptoms ( Fig. 1 ). Hypertonia is one of the positive symptoms and plays an integral role in the formation of deformities in growing children with cerebral palsy ( Fig. 2 ). Although it is not known to what extent hypertonia plays a role in the process of deformity or functional limitations, it is a major factor in reducing range of motion and inhibiting growth of muscle, which disadvantages alignment. Hypertonia and, in particular, spasticity act as a brake on the musculoskeletal system, which increases the work of walking, which in turn inhibits function.
This article reviews hypertonia and provides information on discriminating between spasticity, dystonia, and rigidity. Medication and neurosurgical options for management of hypertonia are presented and compared. The orthopedic surgeon cares for the whole child and should become familiar with commonly used tone management strategies.
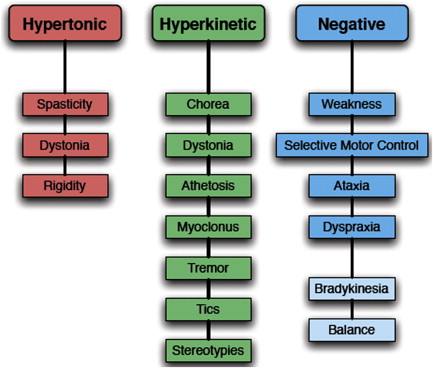
Discriminating between hypertonic syndromes
Hypertonia is defined as abnormally increased resistance to externally imposed movement about a joint perceived by the examiner. Hypertonia may be caused by spasticity, dystonia, and rigidity, alone or in combination. It is important to be able to distinguish between these syndromes because each one is its own entity and may require different types of treatments. A US National Institutes of Health–sponsored Taskforce on Childhood Motor Disorders convened to propose a set of consensus definitions in 2003 to facilitate communication of clinical findings between colleagues, to aid in the selection of patients for inclusion in research trials, to assist with prediction of clinical outcomes, and to aid in clinical decision making for appropriate treatments.
Definition of Spasticity
Spasticity is the most common tone abnormality in children with cerebral palsy. However, not all tight or hypertonic muscles are spastic. The consensus-based definition formulated by the taskforce is as follows : “Spasticity is a velocity-dependent resistance of a muscle to stretch. It is defined as having one or both of the following signs: (1) resistance to externally imposed movement increases with increasing speed of stretch and varies with the direction of joint movement, and/or (2) resistance to externally imposed movement rises rapidly above a threshold speed or joint angle.” Spasticity can vary depending on several factors such as the patient’s level of activity, level of alertness, emotional state, and discomfort. On examination, upper motor neuron signs such as hyperreflexia, clonus, and Babinski response are commonly present. Spasticity is a result of injury to the central nervous system that produces an upper motor neuron lesion. Secondary consequences of the injury occur all the way to the muscle fiber. Fibers may have increased variability in size, and in some cases there is an increase in the number of type I muscle fibers and a deficiency of type IIb muscle fibers. Spasticity is thought to be the most common tone abnormality in children with cerebral palsy, and it is certainly seen as a common consequence of injury to the white matter of the brain, such as periventricular leukomalacia caused by the stretching of the pyramidal tracts from intraventricular hemorrhage. However, many children have additional dynamic hypertonia, which is attributable to other disorders such as the crossed extensor reflex, causing scissoring that contributes to decreased function. Children with damage only to the corticospinal tracts are more likely to have pure spasticity. Typically these children have periventricular leukomalacia as premature infants and have a typical spastic diplegic pattern of spasticity where legs are more involved than arms, fair to good trunk control, and learning disabilites more than intellectual disabilities.
Definition of Dystonia
Careful examination of children with cerebral palsy discloses mixed tone abnormalities. As spasticity treatments have evolved, such as the selective posterior rhizotomy, it is apparent that dystonia underlies some of the more complicated clinical pictures and impacts prognosis. A child with evidence of increased tone on examination that is not improving with standard anti-spasticity treatments may also be suffering from an underlying dystonia. The consensus-based definition formulated by the Taskforce on Childhood Motor Disorders is as follows : “Dystonia in childhood is a movement disorder in which involuntary sustained or intermittent muscle contractions cause twisting and repetitive movements, abnormal postures, or both.” Dystonia can cause hypertonia if there is dystonic muscle contraction opposing passive movement of the limb being tested by the examiner, which is referred to as dystonic hypertonia. Dystonia can also be classified in relation to the region of the body that is affected. Focal dystonias affect a single body part, segmental dystonias affect contiguous body parts, and multifocal dystonias affect 2 or more noncontiguous body parts. On examination, dystonia can be observed while the patient is at rest or is sometimes triggered by a voluntary task. The physiology behind dystonia involves cocontraction of antagonist muscles, overflow of electromyographic activity onto uninvolved muscles during voluntary movement, and involuntary activation of muscles during passive shortening, which may be the result of damage to deeper structures of the brain, including the basal ganglia, which acts as a feedback loop for cortical activity. Children with damage to the basal ganglia or its connecting pathways may present with dystonia or mixed tone abnormalities such as spasticity with an underlying dystonia. Typically these children have more complex etiologies such as hypoxic ischemic encephalopathy, equal involvement of upper and lower extremities, fair to poor trunk control, and are more likely to have intellectual disability. On careful examination, many children with cerebral palsy will have dystonia.
Definition of Rigidity
Rigidity is defined as a condition in which any joint is unable to be moved. However, the consensus definition describes rigidity as cases in which all of the following are true : “(1) the resistance to externally imposed joint movement is present at very low speeds of movement, does not depend on imposed speed, and does not exhibit a speed or angle threshold; (2) simultaneous co-contraction of agonists and antagonists may occur, and this is reflected in an immediate resistance to a reversal of direction of movement about a joint; (3) the limb does not tend to return toward a particular fixed posture or extreme joint angle; and (4) voluntary activity in distant muscle groups does not lead to involuntary movements about the rigid joints, although rigidity may worsen.”
Other hyperkinetic movement disorders
Some other hyperkinetic movement disorders include chorea, myoclonus, restless legs syndrome, tics, and tremors. These hyperkinetic disorders are usually involuntary, but they occasionally occur voluntarily as part of a compulsion. Chorea refers to involuntary, irregular, purposeless, nonrhythmic, abrupt, rapid, unsustained movements that seem to flow from one body part to another. Myoclonus is a sudden, brief, shock-like jerk caused by a muscle contraction or relaxation. Restless legs syndrome refers to the phenomenon that describes an unpleasant crawling sensation in the legs while at rest. Tics are abnormal movements (motor tics) or sounds (phonic tics). Tremor is an oscillatory, usually rhythmic and regular, movement affecting one or more body parts.
Other hyperkinetic movement disorders
Some other hyperkinetic movement disorders include chorea, myoclonus, restless legs syndrome, tics, and tremors. These hyperkinetic disorders are usually involuntary, but they occasionally occur voluntarily as part of a compulsion. Chorea refers to involuntary, irregular, purposeless, nonrhythmic, abrupt, rapid, unsustained movements that seem to flow from one body part to another. Myoclonus is a sudden, brief, shock-like jerk caused by a muscle contraction or relaxation. Restless legs syndrome refers to the phenomenon that describes an unpleasant crawling sensation in the legs while at rest. Tics are abnormal movements (motor tics) or sounds (phonic tics). Tremor is an oscillatory, usually rhythmic and regular, movement affecting one or more body parts.
The importance of distinguishing between hypertonia and other hyperkinetic disorders
It is important to distinguish between hypertonia and hyperkinetic movement disorders because they are treated differently. In addition, results of surgical treatment vary depending on the type of tone abnormality. Anticipating or predicting outcomes improves with accurate identification of the tone abnormality. Tone management is essential before and after orthopedic surgery to ensure best results. Postoperative comfort and care, with a focus on pain control and tone management, are essential for a positive functional outcome.
How spasticity and dystonia are measured
Clinical grading scales for either spasticity or muscle tone have primarily been used to assess spasticity. Scales used for the clinical assessment of spasticity are categorized according to their assessment technique and quantification.
The Ashworth Scale is named after the person who first described the principle of muscle tone assessment by scoring on a 5-point scale the resistance encountered in a specific muscle group by passively moving a limb at one specified velocity through its range of motion. This scale is known as the original Ashworth Scale. The Ashworth Scale has 3 modifications, all sharing the same principle. The first modification was made by the addition of an intermediate score, making it a 6-point scale: the Modified Ashworth Scale–Bohannon. A second modification combined the Ashworth Scale and the Modified Ashworth Scale–Bohannon and added grading for the severity of spasticity: the Modified Ashworth Scale–Peacock. A third modification, the New York University Tone Scale, combined the Ashworth Scale with range of motion at a fast velocity stretch.
The Tardieu Scale is derived from the principle of spasticity assessment by joint angle measurement at different velocities of muscle stretch. When hypertonia is measured using the Tardieu Scale, spasticity is clinically assessed by passive movement of the joints at 3 specified velocities. The intensity and duration of the muscle reaction to the stretch are rated on a 5-point scale with the joint angle at which this muscle reaction is first felt. Later, the scale was simplified to the Modified Tardieu Scale, which defines the moment of “catch,” seen in the range of motion of a particular joint angle at a fast passive stretch.
There are other ways to clinically measure spasticity, but the Modified Ashworth Scale and the Tardieu Scale are the 2 most popular methods.
The Barry-Albright Dystonia Scale allows one to quantify dystonia. This scale is a 5-point, criterion-based, ordinal scale designed to assess dystonia in 8 regions of the body: eyes, mouth, neck, trunk, and the 4 extremities. Dystonia is graded as none (score 0), slight (1), mild (2), moderate (3), or severe (4). Individual scores for each region are added for a total score. Each region has specific descriptors for scoring, but the following general rules apply: slight dystonia is present less than 10% of the time, mild dystonia does not interfere with function or care, moderate dystonia is characterized as interfering with a functional activity, and severe dystonia prevents the performance of the activity. It is important to use a scale that is consistent and complementary to the orthopedic examination. Dynamic problems seen on the functional examination, such as scissoring, may be combined problems of spasticity and an underlying movement disorder.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








