Chapter 47  Articular Cartilage Rating Systems
Articular Cartilage Rating Systems
INTRODUCTION
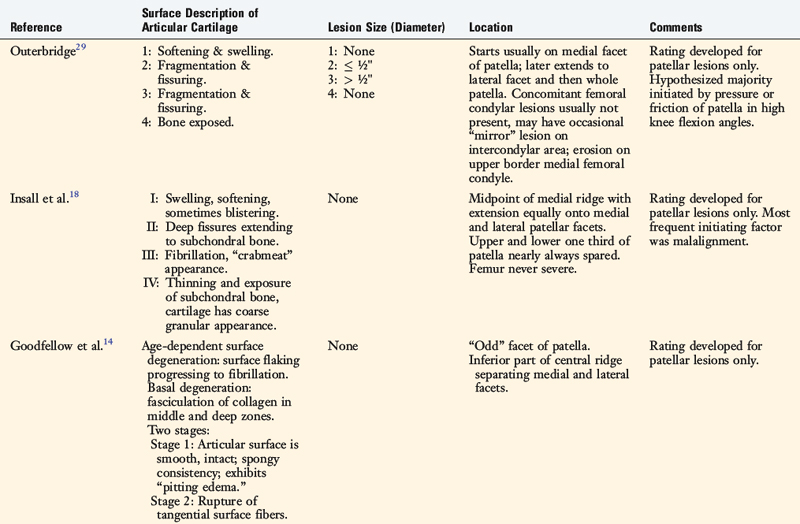
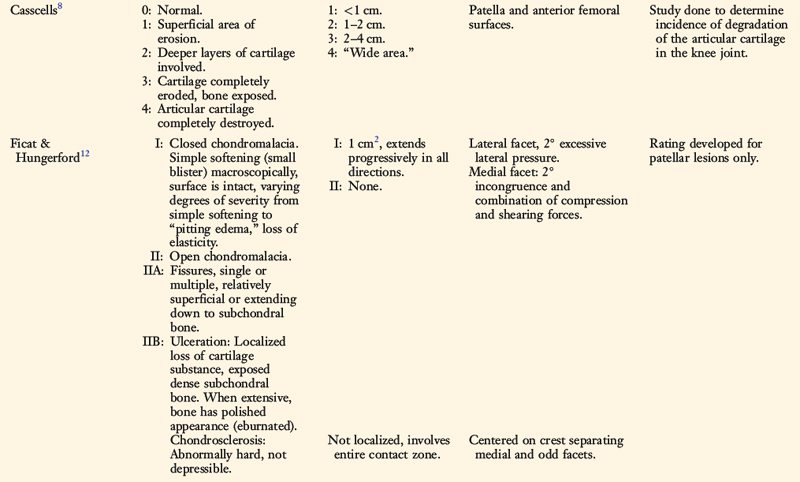
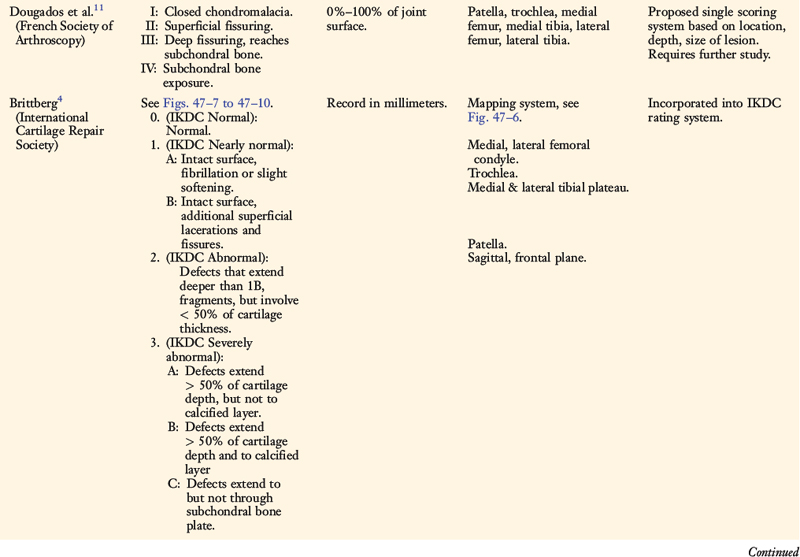
Many systems have been proposed to classify lesions of the articular cartilage in the knee joint (Table 47-1). The cartilage systems published in the 1960s and 1970s introduced grading schemes for lesions located only in the patellofemoral joint and documented the most frequent locations of damage in this compartment.13,14,18,29 The first of these patellofemoral classification systems, proposed by Outerbridge,29 remains one of the most commonly used schemes to grade lesions located in all three compartments of the knee (patellofemoral, medial tibiofemoral, and lateral tibiofemoral).10 As arthroscopy and imaging techniques have evolved, a few investigators 17,28 and societies (International Cartilage Repair Society [ICRS], French Society of Arthroscopy [SFA]) have proposed articular cartilage rating systems that are far greater in sophistication in classifying lesions, as is described later. These systems are useful for formal clinical investigations to determine the etiology and prognosis of partial and full-thickness cartilage injuries after various knee injuries22 and to determine the indications and outcomes of cartilage resurfacing procedures including mosaicplasty and autologous chondrocyte implantation (ACI).6
REVIEW OF PUBLISHED ARTICULAR CARTILAGE RATING SYSTEMS
Outerbridge
In 1961, Outerbridge29 introduced a system for grading articular cartilage lesions in the patellofemoral joint. The four-gradient scale was based on the appearance of the cartilage and, in two of the levels, the size of the lesion. A grade 1 lesion was defined as softening and swelling of the cartilage. A grade 2 lesion involved fissuring and fragmentation in an area less than ½” in diameter. A grade 3 lesion involved fissuring and fragmentation in an area greater than ½” in diameter. In a grade 4 lesion, the cartilage was eroded down to subchondral bone. This rating system did not specify the location, depth, or exact size of the lesion.
Insall
Insall and coworkers18 proposed a classification system for patellofemoral articular cartilage lesions that was composed of four stages based on the cartilage appearance. The first stage consisted of swelling, softening, and blistering of the cartilage. The second stage included lesions with deep fissures that extended to subchondral bone. The third stage involved fibrillation and a “crabmeat” appearance. In the fourth stage, thinning of the cartilage and exposure of subchondral bone in some areas were noted, with the remainder of the cartilage demonstrating a “coarse granular appearance.” This rating system also failed to specify the location, depth, and size of the lesion.
Critical Points REVIEW OF PUBLISHED ARTICULAR CARTILAGE RATING SYSTEMS
Cincinnati Knee Rating System
SFA System (French Society of Arthroscopy)
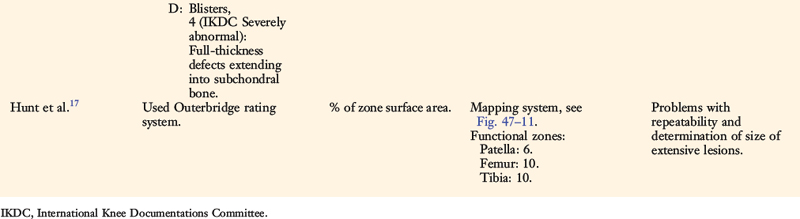
International Cartilage Repair Society
Hunt
Goodfellow
Goodfellow and associates15 described two different types of disorders of articular cartilage in the patellofemoral compartment: age-dependent surface degeneration and basal degeneration. Age-dependent surface degeneration was usually found on the odd facet, was often present in middle-aged patients, and became even more frequent with increasing age. These lesions involved surface flaking that progressed to fibrillation and, finally, subchondral bone exposure. The authors believed these lesions were asymptomatic in younger patients, but could become painful as degenerative joint disease in later years.
Casscells
Casscells8 used a rating system to describe lesions located on the undersurface of the patella and femoral condyles in an anatomic cadaveric investigation. The five-level gradient classification included both cartilage appearance and size of the lesion. Grade 0 indicated normal surfaces with no gross lesions present. Grade 1 included small, superficial areas of cartilage erosion, 1 cm or less in diameter. Grade 2 lesions were 1 to 2 cm in diameter and involved the “deeper layers” of cartilage. Grade 3 indicated lesions that were 2 to 4 cm in diameter in which the cartilage was completely eroded and subchondral bone was exposed. Grade 4 designated cartilage that was “completely destroyed,” often involving complete loss of the entire articular surface.
Ficat and Hungerford
Ficat and Hungerford12 described a two-stage classification system for lesions in the patellofemoral compartment based on the appearance of the cartilage. Stage one was described as closed chondromalacia in which the surface was intact but the degree of severity varied from simple softening to “pitting edema” and loss of elasticity. Stage two was defined as open chondromalacia. This stage was subdivided into two groups: A, single or multiple fissures that were either relatively superficial or extended down to subchondral bone; and B, ulceration or localized loss of cartilage substance, exposed dense subchondral bone that represented the final stage of cartilage destruction.
Cincinnati Knee Rating System
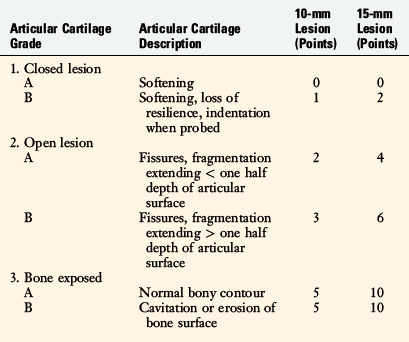
In 1989, Noyes and Stabler28 proposed a new articular cartilage classification system that included four variables: the appearance of the cartilage (as visualized arthroscopically), the depth of the lesion, the size (diameter) of the lesion, and the location of the lesion. A point scaling system was devised for research purposes to facilitate statistical analyses (Table 47-2).
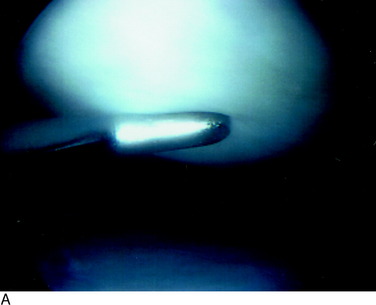
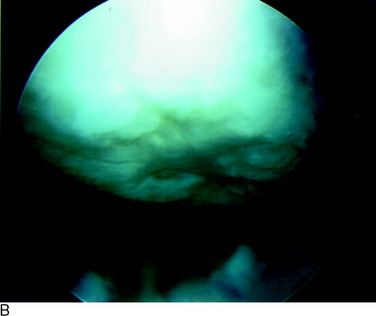
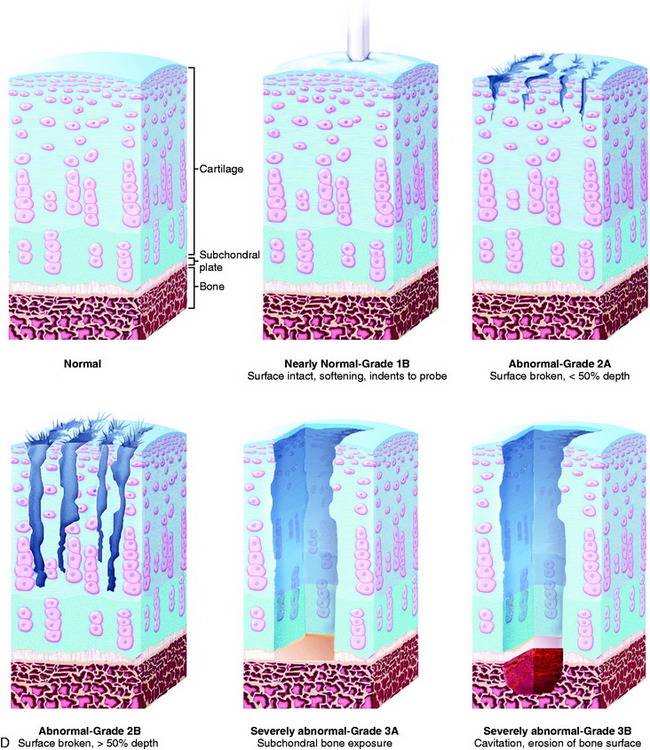
Grade 1A corresponds to a moderate degree of softening of the cartilage compared with its normal resilient appearance (Fig. 47-1A). Grade 1B designates complete loss of resilience, resulting in full indentation of the surface when probed (see Fig. 47-1B). This grade is reserved for lesions in which a severe softening of the cartilage exists without gross surface breakage. This description indicates the initial stage of cartilage deterioration characterized by diminished glycoproteins and early collagen fiber deterioration.28 These lesions, which commonly involve the undersurface of the patella, have a high potential to progress to an open lesion.
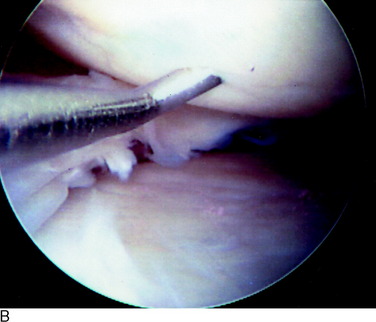
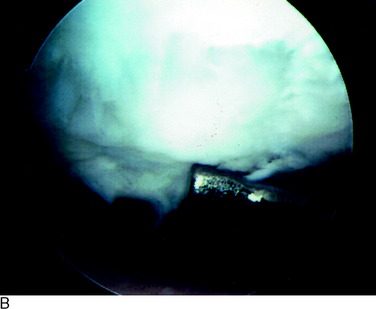
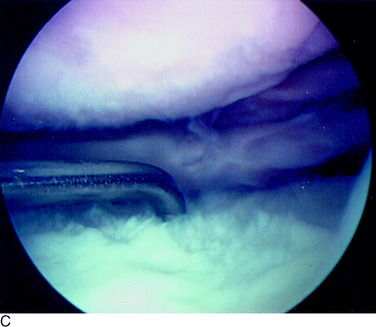
A grade 2A lesion (Fig. 47-2A) is an open disruption of the cartilage surface, including cracks, surface blisters, fissures, fibrillations, and fragmentations that extend less than one half of the thickness of the cartilage. Grade 2B lesions (see Fig. 47-2B and C) are similar in appearance, but extend greater than one half of the thickness of the cartilage. Superficial lesions with fibrillation-type changes are usually easily distinguishable from deeper lesions that involve lacerations, clefts, and fragmentation down to bone. Chondrosclerosis is classified as a grade 2 lesion, because the surface is abnormal. Lesions that have two or three deep lacerations that extend through the cartilage surrounded by otherwise normally appearing cartilage are graded as 2B.
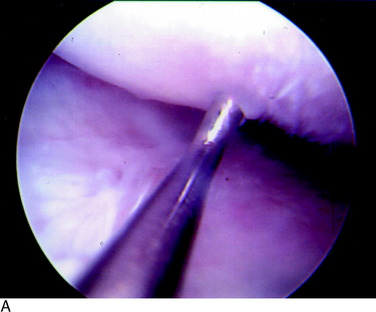
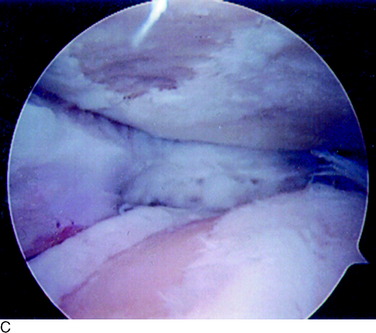
A grade 3A lesion (Fig. 47-3A) indicates a surface with exposed bone in which the normal bony contour remains. The most severe lesion, grade 3B (Fig. 47-3B and C), indicates cavitation or erosion of the bone surface. An example of a grade 3B lesion is an osteochondritis dissecans lesion in which there is loss of the subchondral bone. Other examples are lesions in which grooving of the bony surface is visualized or those involving fractures that extend through the subchondral bone.
The size of all lesions is determined using a calibrated nerve hook probe. The size is recorded according to one of five categories ranging from less than 10 mm to greater than 25 mm (see Table 47-1). A schematic illustration of all grades is shown in Figure 47-3D.
Figure 47-4A illustrates how this classification system is used to record the visual appearance of articular cartilage lesions. The patella has a 10-mm grade 2A lesion that is surrounded by a larger closed area of softening (1B) that extends 20 mm in diameter. The trochlea has a large area of extensive softening as well, graded as a 1B that is 25 mm in diameter. The medial femoral condyle also has a large area of extensive softening, measuring 15 mm in diameter. A “kissing” lesion is found on the medial tibial plateau of a grade 2A lesion that is 10 mm in diameter. The lateral femoral condyle has a complex lesion; 10 mm of exposed bone (3A) is surrounded by an open lesion of fragmentation of 20 mm in diameter (2B), which is in turn surrounded by a closed lesion of soft cartilage that extends to 25 mm (1B). The lateral tibial plateau has a large 2B lesion, 15 mm in diameter. For research purposes, the lesions may be quantified on a scaling system to allow statistical analysis (see Table 47-2). Any lesion that is less than 10 mm in diameter, or graded 1A, is not considered clinically significant and, therefore, no points are given. Figure 47-4B illustrates the points awarded for the lesions noted in the example.
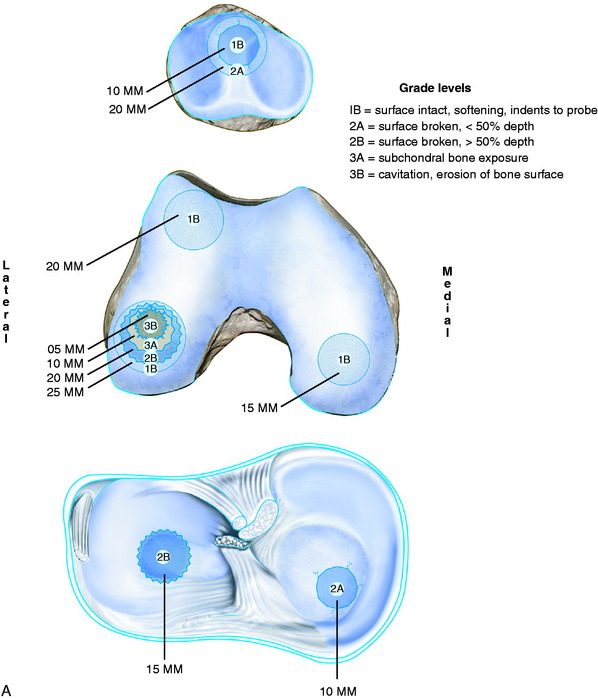
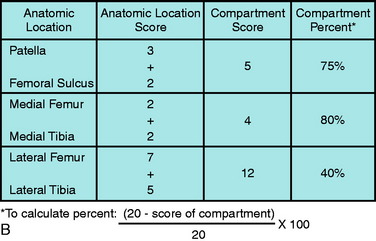
FIGURE 47-4 A, An example of the grading of articular cartilage lesions found at arthroscopy. B, Scoring system for articular cartilage lesions (see Table 47-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree