Anesthesia
Hip arthroscopy is performed under general anesthesia with muscle relaxation to facilitate hip joint distraction. We have had good success with preoperative fascia iliaca blockade to minimize intraoperative and postoperative opioid consumption (
26). Controlled hypotensive anesthesia is utilized as well, with target systolic blood pressure ≤ 90 mm Hg, to minimize bleeding and facilitate visualization during the procedure.
Patient Positioning
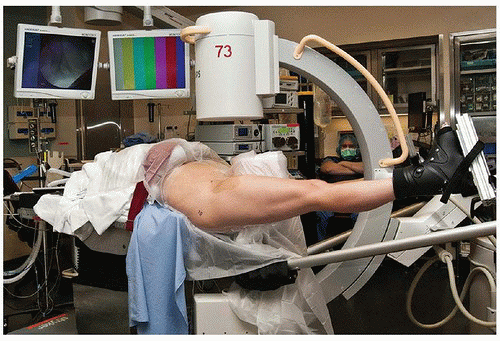
Supine (
27) and lateral (
28) positioning for hip arthroscopy have been described. We routinely utilize supine positioning, as this is typically more familiar to operating room personnel and can be accomplished using a standard fracture table. Once general anesthesia has been administered, a well-padded radiolucent perineal post is inserted into the traction table and the patient is moved towards the foot of the bed until the post is in contact with the perineum. The post should be lateralized towards the operative hip so that it primarily contacts that medial upper thigh. This provides a fulcrum against which to distract the hip and theoretically reduces direct pressure on the pudendal nerve, possibly avoiding pudendal nerve injury (
29,
30,
31). The contralateral arm can be left on an arm board to the patient’s side while the ipsilateral arm is draped over the chest and secured. Next, the patient’s feet are secured in traction boots in a well-padded fashion using cast padding and Coban self-adhesive wrap. The operative foot must be particularly secure to prevent slippage during the application of traction. Once the feet are secured, the foot of the table can be removed. The non-operative leg is placed in approximately 45 degrees of abduction, while the operative leg is kept in neutral rotation, slight abduction, and full extension (
Fig. 7-6).
Fluoroscopy Positioning
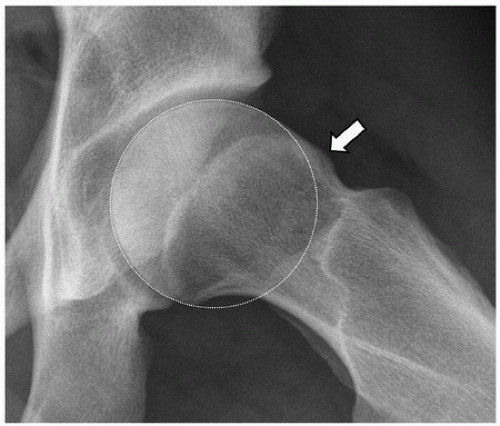
Ensuring that adequate fluoroscopic images can be obtained prior to prepping and draping is crucial to the success of any hip arthroscopy, in order to carry out the preoperative plan. Slight traction is applied to both legs to stabilize the pelvis. The C-arm is brought in between the legs and the beam is centered over the operative hip. The preoperative AP pelvis radiograph is displayed on a separate operating room monitor while AP fluoroscopic images are obtained. The C-arm is then adjusted until the AP fluoroscopic image closely replicates the AP pelvis radiograph. The lateral acetabulum and medial teardrop are good landmarks to use to confirm similarity between images, and the lateral acetabulum will help
identify the amount of crossover and overcoverage that should be resected. This step eliminates any discrepancies in radiographic acetabular coverage markers between the preoperative radiographs and the fluoroscopy images. Next, the C-arm gantry is rotated to a near horizontal and then horizontal position, and the ability to obtain an adequate oblique lateral and cross-table lateral, respectively, is confirmed. Note that the greater trochanter may obscure the distal femoral neck on oblique and lateral images, which, if not remedied, may cause a failure to recognize and treat distal impinging Cam lesions.
Application of Traction
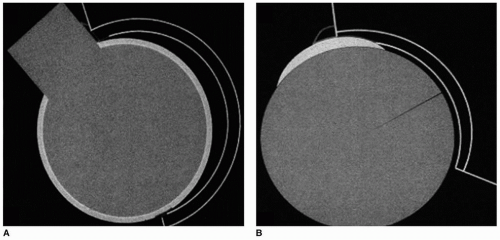
At least 8 to 10 mm of hip joint distraction must be obtained in order to introduce arthroscopic instruments into the hip joint without causing iatrogenic chondral and/or labral damage (
32). This typically requires 25 to 50 pounds of traction (
27). In-line traction is applied to the operative leg, and countertraction is applied to the nonoperative leg. Initial traction is applied with the operative hip slightly abducted, and subsequent adduction will assist with joint distraction, due to the fulcrum of the perineal post.
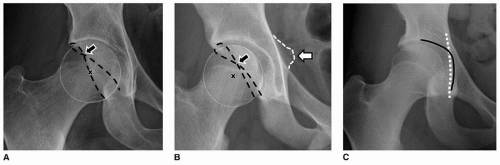
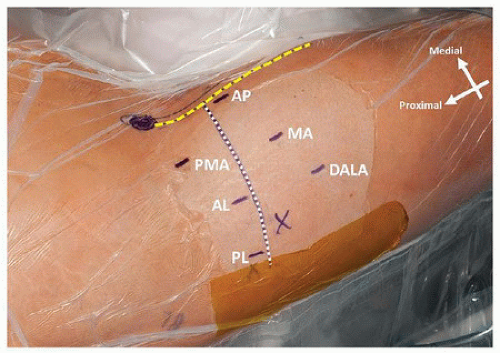
Anatomic landmarks for portal placement are identified only after joint distraction is established to prevent migration of the skin relative to the underlying bony landmarks. The first landmarks to identify and mark are the anterior superior iliac spine (ASIS) and the tip of the greater trochanter. Two perpendicular lines are then drawn: one from the ASIS distally to the center of the patella and one from the tip of the trochanter anteriorly to the intersection with the first line (
Fig. 7-7). Subsequent portal placement should be kept lateral to the ASIS-to-patella line to minimize risk of femoral nerve injury (
33,
34).
The vast majority of hip arthroscopy for FAI in our practice is performed using two portals— midanterior (MA) and AL. A spinal needle through the posterolateral (PL) portal is used for outflow purposes. Under fluoroscopic guidance, a 6-inch spinal needle is advanced from the AL portal starting point towards the hip joint at an insertion angle of approximately 15 degrees towards the floor and 15 degrees cephalad. As the spinal needle is advanced into the joint, care must be taken to avoid piercing the labrum and avoid damaging the femoral articular cartilage. To aid in this, the needle is aimed just proximal to the femoral head (as far from the labrum as possible) with the bevel towards the head (to minimize risk of iatrogenic cartilage injury) (
35).
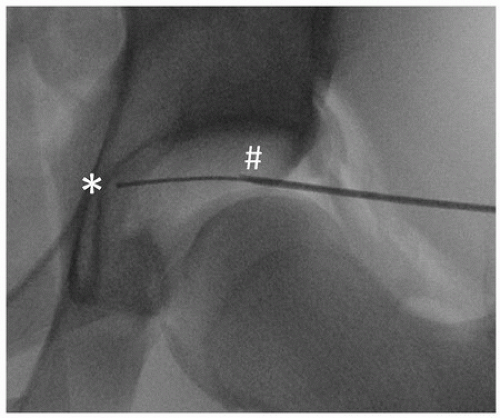
Once the spinal needle is in the hip joint, the stylet is removed and air is injected into the joint to create an air arthrogram. A second AP fluoroscopic image is obtained. If the spinal needle has migrated proximally, it may be within the labrum and should be removed and positioned more distally. If the spinal needle remains stationary after the air arthrogram, it is safe to proceed with instrumentation of the hip joint. A Nitinol wire is threaded through the spinal needle until resistance is met. Position is checked on fluoroscopy, and the guide wire should be seen abutting the medial acetabular wall (
Fig. 7-8). If the guide wire does not advance all the way to the medial wall, it may be too anterior or posterior and the spinal needle should be repositioned accordingly. If needed, a lateral fluoroscopic image can help determine anteroposterior placement of the spinal needle.
After confirming proper intra-articular position, a skin incision is made over the guide wire. A 4-mm dilator is passed over the guide wire followed by the 4.5-mm arthroscopy trocar. This step should be performed with a twisting motion and slow, controlled pressure to minimize the risk of plunging and damaging the articular cartilage after the hip joint capsule is pierced. The 70-degree arthroscope is introduced into the hip joint dry with the inflow turned off.
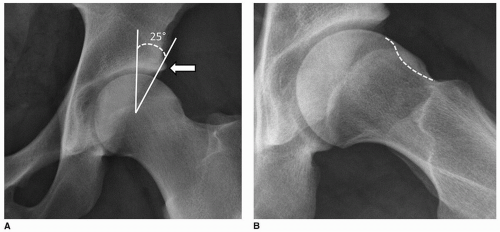
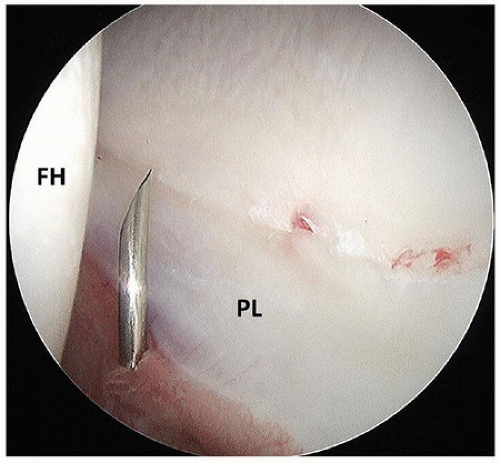
Under direct visualization, the PL outflow portal is now established. Looking posteriorly, the “V” between the posterior labrum and the femoral head is identified (
Fig. 7-9). The 6-inch spinal needle is advanced from the PL portal starting point to the center of this “V.” The typical trajectory is 5 degrees towards the ceiling and 5 degrees cephalad, with slight convergence to the camera in the AL portal.
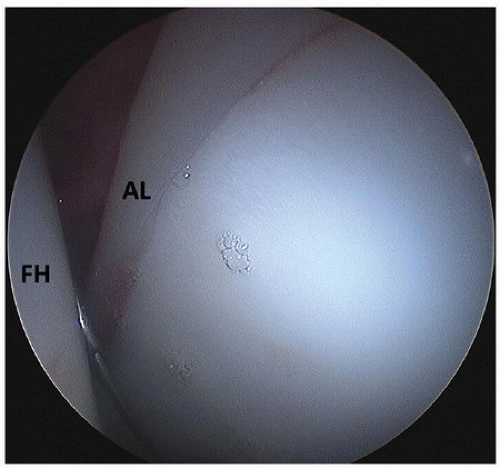
Next, the MA portal is established under direct visualization. Looking anteriorly, the “V” between the anterior labrum and the femoral head is identified (
Fig. 7-10). The 6-inch spinal needle is advanced from the MA portal starting point to the apex of this “V,” with a typical trajectory of 25 degrees towards the floor and 35 degrees cephalad. Once the spinal needle is properly positioned, the stylet is removed and a Nitinol guide wire is inserted. A skin incision is made, and the 4-mm dilator is threaded over the wire, followed by a 6-mm dilator.