Arthroscopically Assisted Triangular Fibrocartilage Complex Débridement and Ulnar Shortening
Brandon P. Donnelly
Randall W. Culp
DEFINITION
The triangular fibrocartilage complex (TFCC) is a homogenous anatomic structure located on the ulnar aspect of the wrist that is responsible for distal radioulnar joint (DRUJ) stability and transfers load across the wrist from the ulnar carpus to the distal ulna.21
Injury to the TFCC and subsequent synovitis is associated with ulnar-sided wrist pain, weakness of grip, and painful clicking about the DRUJ often resulting in patient disability.
Ulnocarpal abutment or ulnar impaction syndrome is characterized by ulnar-sided wrist pain associated with a TFCC tear and accompanying variable chondromalacia of the ulnar head, lunate, and triquetrum surfaces. The degenerative process typically occurs in ulnar positive or neutral variance from chronic compressive overloading of the ulnocarpal joint.
Arthroscopic TFCC débridement is indicated for centrally based lesions and may be combined with ulnar shortening in light of concomitant ulnocarpal abutment.
ANATOMY
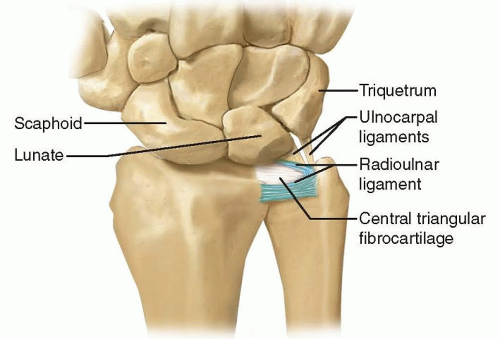
The TFCC is a confluence of cartilaginous and ligamentous structures that span and support the DRUJ and ulnocarpal articulations. It arises from the distal aspect of the radial sigmoid notch and inserts into the base of the ulnar styloid and fovea (FIG 1).
The ulnocarpal complex, consisting of the ulnolunate ligament, ulnotriquetral ligament, and extensor carpi ulnaris (ECU) subsheath, spans the ulnocarpal joint.
The superficial limbs of the dorsal and palmar radioulnar ligaments insert onto the base of the ulnar styloid, whereas the deep limbs insert into the fovea.11
The central articular disc is a thin fibrocartilage structure, spanning from the distal rim of the sigmoid notch and blends with the radioulnar ligaments.
PATHOGENESIS
Acute, Palmer I, TFCC injuries typically result from an axial load in ulnar deviation, combined with forearm rotation. Biomechanically, the TFCC becomes compressed and stretched between the ulna and lunate producing a tear.
These injuries typically occur in falls on a pronated outstretched hand or activities that require forceful ulnar deviation of the wrist (eg, golf and racquet sports).
Intra-articular distal radius fractures show a high incidence of concomitant tears of the triangular fibrocartilage, 50% to 84%.6,13 However, many of these tears are minimally symptomatic and do not require surgical intervention.16
Chronic degenerative tears of the TFCC are associated with ulnar positive variance and ulnar carpal impaction (FIG 2).
Ulnar positive variance occurs with any condition that causes a relative greater ulnar than radial length at the wrist. These include distal radius malunion, Essex-Lopresti lesion, developmental positive ulnar variance, and premature radial physeal closure.
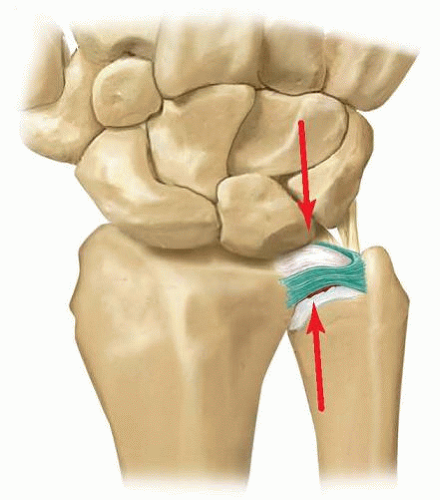
FIG 2 • Ulnar abutment. The TFCC is compressed between the proximal ulnar lunate and the distal ulnar head.
Degenerative tears result from chronic load to the ulnar side of the wrist. In an ulnar neutral wrist, the ulnar carpus absorbs 18% of axial load. This increases to 42% when ulnar variance is increased 2.5 mm and decreases to 4.3% when ulnar variance is decreased 2.5 mm.20
NATURAL HISTORY
The natural history of Palmer type I TFCC tears is not well understood. Many type IA lesions without instability respond to nonoperative management.22 In a long-term follow-up, Mrkonjic et al16 showed that distal radius fracture associated TFCC tears with a stable DRUJ showed some increased laxity and decreased grip strength but did not require routine surgical treatment.
Surgical débridement for failed conservatively treated type IA lesions showed excellent success.18 However, high failure rates were noticed when TFCC débridement alone was performed in the ulnar positive wrist.15
Types I B, C, and D tears may result in clinical instability of the DRUJ and require surgical intervention to restore stability.
Degenerative tears (type II) are nontraumatic with a natural history that shows TFCC attrition in more than half of patients older than 50 years of age.3 Also, after the fifth decade, 100% of TFCCs evaluated showed an abnormal appearance but usually asymptomatic.4
Symptomatic degenerative tears typically have progressive degenerative changes that involve the ulnocarpal joint surfaces, which may or may not strictly follow the progressive cascade in accordance with Palmer’s classification: TFCC wear (IIA), ulnar or lunate chondromalacia (IIB), central TFCC perforation (IIC), lunotriquetral ligament tear (IID), and arthritic changes of the lunate and triquetrum (IIE).
It is possible to have components of a type I traumatic tear in a wrist with a preexisting degenerative TFCC, in which an acute flap causes mechanical symptoms. In this case, arthroscopic débridement alone may not improve symptoms and ulnocarpal decompression is warranted.
PATIENT HISTORY AND PHYSICAL EXAMINATION
Patients often report ulnar-sided wrist pain occurring after a fall. They may also complain of clicking, catching, weakness, localized swelling, and a sense of instability.
Physical examination reveals swelling over the ulnar wrist, with focal tenderness over the TFCC and distal ulna.
Fovea sign—direct pressure applied to the fovea region that reproduces their pain had 95.2% sensitivity and 86.5% specificity for TFCC foveal disruption and/or ulnotriquetral ligament injury.24
Ulnocarpal palpation—pain at the ulnocarpal joint suggests synovitis or TFCC pathology.
TFCC stress test—ulnar deviation and axial loading of wrist reproduces a painful click with forearm rotation.
Ulnocarpal stress test—pain reproduced during pronation and supination of the forearm with the wrist in ulnar deviation
Pisiform boost test—increased pain of passive and active ulnar deviation with dorsally directed pressure applied over the palmar aspect of the pisiform, resulting in a lifting of the carpus
The DRUJ must be assessed for instability with shuck or “piano key” test. The distal radius is held in one hand and the other hand stresses the distal ulna volarly and dorsally in neutral rotation, pronation, and supination. This must be compared to the contralateral side.
Instability suggests disruption of the radioulnar ligaments.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The radiographic evaluation of a patient with ulnar abutment should include a standard wrist series, a Palmer 90 × 90 neutral rotation view19 and a fully pronated grip stress view.25
The Palmer 90 × 90 view places the forearm in neutral rotation while the elbow is flexed to 90 degrees and the shoulder is abducted to 90 degrees. The static ulnar variance is calculated from this view (FIG 3).
The fully pronated grip stress view has the shoulder adducted to the patient’s side and slightly externally rotated, the forearm is pronated, and the patient is asked to make a fist of maximum intensity. An increase ulnar variance indicates dynamic variance.
Ulnar impaction is suspected in a patient with an ulnarzero or ulnar-plus variance. Subchondral cystic and sclerotic joint changes in the lunate indicate probable ulnar impaction (FIG 4).
Magnetic resonance imaging (MRI) evaluation of the triangular fibrocartilage can aid in diagnosis especially in central tears. Magnetic resonance (MR) arthrogram has been shown to be more sensitive than standard MR imaging but can have higher false positives.12,23
On T2 imaging, an intact TFCC has a homogenous low signal.
An MRI should be considered for ulnar impaction syndrome in the absence of clear radiographic findings. Characteristic early findings include bone hyperemia in the lunate, triquetrum, and ulnar head, which has low signal intensity on T1-weighted images and high signal intensity on T2-weighted images (FIG 5A,B).9
DIFFERENTIAL DIAGNOSIS
TFCC tear
Ulnocarpal impaction
Ulnocarpal synovitis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree