Arthroscopic Revision Rotator Cuff Repair
In general, the results of open revision rotator cuff repair after failure of the initial surgery have been poor. However, the reports of arthroscopic revision rotator cuff repair have been much better than those of open revision. We first reported our results of arthroscopic revision in 2004 (1), and subsequent authors have reported similarly encouraging results (2,3). We also recently completed a study of 74 revision rotator cuff repairs, the majority of which were massive tears, with a mean follow-up of 63 months (1). Despite the fact that most of these recurrent tears were massive tears, the majority of patients achieved a good or excellent functional outcome and 78% of patients were satisfied with the revision repair. In our opinion, all revision repairs of the rotator cuff should be done arthroscopically.
CAUSES OF FAILURE
There are three broad categories of patients that require a second surgery after the initial rotator cuff repair:
a. Biomechanical failure due to inadequate strength of the repair construct
b. Biologic failure to heal despite strong fixation
c. Aggressive postoperative rehabilitation causing structural failure of the repair construct
The rest of this chapter will deal with patients who have structural failure after rotator cuff repair.
CLINICAL EVALUATION
When structural failure occurs, the surgeon must decide if further surgery is indicated. A structural failure does not always result in a clinical failure. Many patients with partial healing of the cuff and a residual defect will be much better after surgery, and in these patients, nothing needs to be done. In general, patients who still have disabling pain and weakness at 9 to 12 months after surgery should be evaluated for possible revision repair.
The clinical examination is important. Active and passive range of motion are measured. We define pseudoparalysis as active elevation of <90° in a patient who has full overhead passive elevation in association with an unstable glenohumeral fulcrum; that is, there is a significant discrepancy between active and passive elevation along with the potential for anterosuperior glenohumeral escape. In primary repair cases, we have found that patients with pseudoparalysis will regain overhead motion after repair in 89% of cases (Unpublished Data). However, pseudoparalysis after a failed primary cuff repair is a poor prognostic sign, and many patients in that category with a massive rotator cuff tear will never regain overhead motion with a second surgery. In the setting of revision for massive rotator cuff tears, we have found that 43% of patients with preoperative pseudoparalysis regain active elevation to 90° or greater (Unpublished Data). In our experience, even if a patient does not regain overhead motion after revision cuff repair, function may still be greatly improved below shoulder level if subscapularis function is restored. The subscapularis is very important in personal hygiene, as it is essential for achieving enough internal rotation for independent toileting as well as for obtaining enough horizontal adduction to reach across the body and wash under the opposite axilla. These functions are essential to anyone who lives alone and wishes to be independent. Therefore, evaluation of subscapularis function (bear-hug, belly-press, Napoleon, and lift-off tests) is very important.
Another poor prognostic category is the patient who, after the initial cuff repair, cannot externally rotate to neutral (0°) with the arm at the side. These people will usually have a pseudoparalysis and often will not regain overhead function with a second repair.
If active and passive elevation are limited to the same degree, this is not pseudoparalysis. These patients are typically restricted by capsular contracture and subacromial adhesions and will generally do very well with arthroscopic capsular release and lysis of adhesions.
Imaging studies are important. Plain radiographs should be taken to evaluate for other causes of pain (e.g., chondrolysis, loose anchors, acromial fracture). An MRI scan is important, but the surgeon must not be fooled by the postoperative changes and artifacts that may occur in these patients. For example, an MRI scan taken at 3 months postoperatively can still show large areas of tendon that are undergoing revascularization that can look like a recurrent tear when the tendon is actually intact (Fig. 8.1). Also, we have found that the third-generation high-strength sutures can cause significant artifact that can mimic a small recurrent cuff tear, when in fact the cuff is intact (Fig. 8.2).
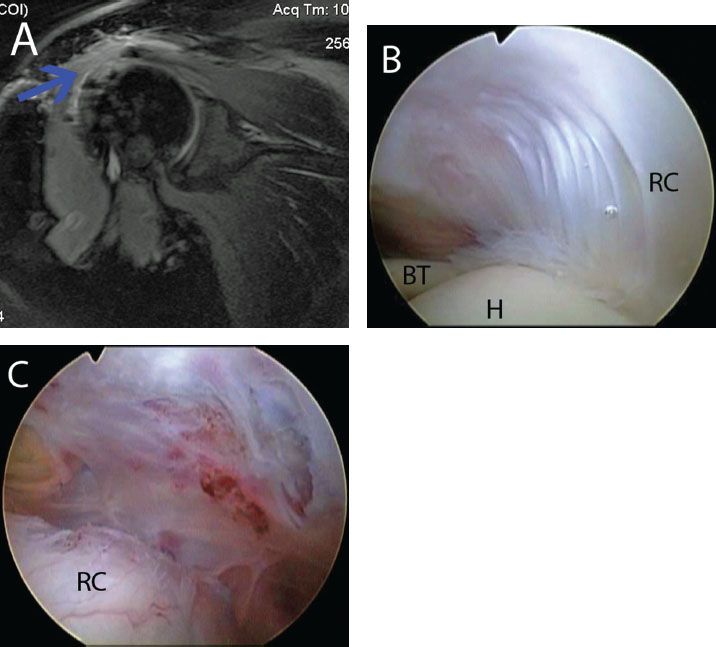
Figure 8.1 A: Three-month postoperative coronal magnetic resonance image of a right shoulder demonstrates revascularization (blue arrow) that was interpreted as a recurrent rotator cuff tear. Arthroscopic view of the same shoulder from (B) posterior glenohumeral and (C) posterior subacromial viewing portals, demonstrate a healed rotator cuff. BT, biceps tendon; H, humerus; RC, rotator cuff.
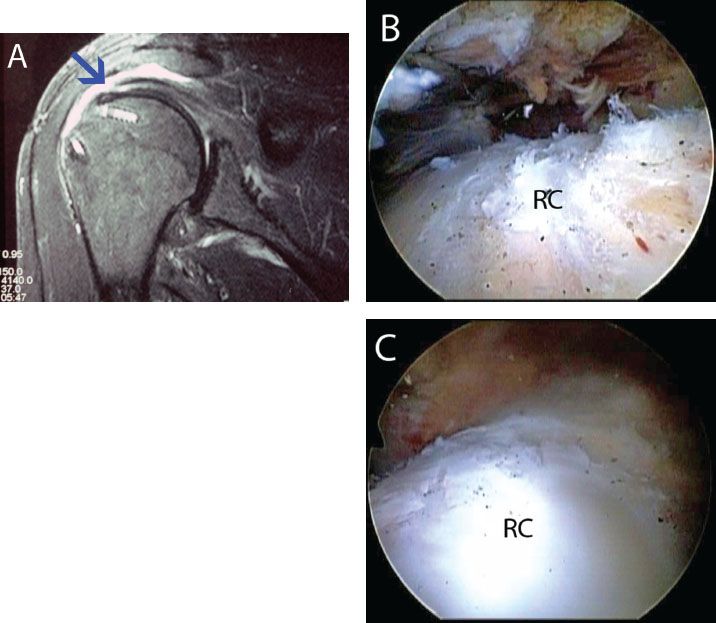
Figure 8.2 A: Postoperative coronal magnetic resonance image of a right shoulder was interpreted as a recurrent rotator cuff tear. The blue arrow demonstrates a linear signal change in the rotator cuff that is suture artifact and led to the misinterpretation by a radiologist. Arthroscopic views in the same shoulder from (B) posterior and (C) lateral subacromial portals demonstrate a healed rotator cuff. RC, rotator cuff.
The T-1 parasagittal MRI cuts are important for evaluating muscle quality, but the cuts must be taken far enough medially to transect the muscle belly, particularly in a retracted tear. Previous authors have recommended that if fatty infiltration is ≥50% of the muscle cross section, then rotator cuff repair should not be done since the patient will not improve with surgery (5). However, our experience has been notably different. We have found that most patients with fatty infiltration of the supraspinatus or infraspinatus of up to 75% will improve at least one grade in strength after cuff repair, so we routinely operate on patients with up to 75% fatty infiltration (6). The subscapularis is an exception to all the rules, as much of its function derives from a tenodesis effect. We have observed complete healing on MRI as well as reversal of pseudoparalysis in patients with 100% fatty infiltration of the subscapularis.
Another consideration in the preoperative imaging studies is to evaluate for the amount of “real estate” in the bone bed of the greater tuberosity that is available for additional suture anchor placement. If large numbers of anchors are already present, or if cystic cavitation has occurred around the anchors, then the surgeon may have to remove some or all of the existing anchors and bone graft the defects (Fig. 8.3). We prefer to do arthroscopic grafting with allograft bone chips packed into an OATS harvester (Arthrex, Inc., Naples, FL). Since it is often difficult to tell how much “good bone” is actually left in the greater tuberosity, we routinely discuss the possible necessity of an allograft bone graft and obtain patient consent to do this in all revision cases.
Finally, the MRI will usually indicate if the supraspinatus and infraspinatus are adhesed to the undersurface of the acromion. This is important to determine because we have found that, in the case of extensive tendon adhesion to the acromion, we almost always have to do a modified doubleinterval slide in order to gain enough lateral excursion of the tendons to reach the bone bed.

Figure 8.3 Preoperative radiograph of a right shoulder demonstrates multiple metallic anchors from a previous failed repair. In this scenario, bone grafting at the time of revision is often required.
ARTHROSCOPIC STEPWISE APPROACH TO REVISION CUFF REPAIR
Overview of Steps
Doing a revision repair of a massive rotator cuff tear can be a daunting undertaking, with hundreds of individual steps involved in the procedure. Therefore it is useful to break down the project into its seven basic components:
The simplistic way of thinking about revision repair of a massive cuff tear is that we begin our repair anteriorly, with the subscapularis, and gradually work our way posteriorly. Naturally, not all revisions involve massive tears, but since massive tears retear at a higher rate than small tears, the majority of revision repairs will be in massive tears.
If the revision is being done for a small- or a medium-sized retear, the situation is usually much easier. We first do an intra-articular arthroscopy and subacromial bursoscopy and identify the tear. If needed, we do an arthroscopic capsular release and subacromial lysis of adhesions (see technique in Chapter 21, “Shoulder Stiffness”). Then we repair the tear by standard techniques. If possible, we prefer linked double-row footprint reconstruction by SutureBridge or SpeedBridge techniques, but if there is tendon loss or insufficient excursion of the tendon, we do a single-row repair.
For the large and massive revision repairs, it is instructive to take an in-depth step-by-step look at the seven basic components of revision cuff repair.
Addressing the Biceps
A posterior viewing portal is established. In all revision cases that involve the subscapularis, we do an arthroscopic biceps tenotomy or tenodesis. If the patient is low demand, particularly if the arm is fat enough that a “Popeye” deformity would not be noticeable, we do a tenotomy. In the younger patient, the high-demand patient, or the patient in whom cosmesis is important, we do a biceps tenodesis at the top of the bicipital groove with a BioComposite Tenodesis screw (Arthrex, Inc., Naples, FL) and incorporate the suture limbs from that construct into the rotator cuff repair. When a biceps tenodesis is to be done, we first place half-racking sutures in the biceps arthroscopically, then do a biceps tenotomy. The half-racking sutures are then used to deliver the biceps tendon extracorporeally for placement of a whipstitch (Fig. 8.4). The tendon is then allowed to retract back into the shoulder, where it rests out of the way laterally while the subscapularis work is done.
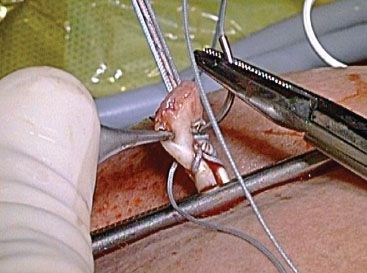
Figure 8.4 External photo demonstrating placement of a whipstitch in preparation for biceps tenodesis.
Addressing the Subscapularis and Related Structures
All of the dissection and preparation of the subscapularis, the coracoid, and the lesser tuberosity are performed through an anterosuperolateral working portal. This portal is established from outside-in while viewing the lesser tuberosity through a posterior viewing portal with a 70° arthroscope. The working portal is established so that its angle of approach into the lesser tuberosity is 5° to 10° (Fig. 8.5).
Then, the arthroscope is switched to a 30° scope while searching for and identifying the subscapularis tendon and the coracoid. Failure to switch to a 30° scope at this juncture can cause the surgeon to wander too far inferiorly while searching for the coracoid tip through a window in the rotator interval.
If the subscapularis tendon is not immediately visible at the front of the joint, it is probably retracted medially to the level of the glenoid margin. It can usually be located by placing the tip of a blunt instrument (e.g., a switching stick introduced through an anterosuperolateral portal) into the soft tissue adjacent to the glenoid rim at the level of the midglenoid notch. The midglenoid notch is the level at which the upper border of the subscapularis tendon usually crosses transversely (Fig. 8.6A). The tip of the switching stick is used to hook into the junction where the superolateral border of the subscapularis tendon joins the comma tissue at approximately a right angle (Fig. 8.6B, C). The comma is the residual portion of the medial sling that had been attached to the lesser tuberosity adjacent to the subscapularis footprint. In rare circumstances, the comma sign is not identifiable due to significant scarring. In this scenario, a window is created just anterior to the glenoid above the midglenoid notch and dissection is carried medially to the base of the coracoid where the subscapularis can be reliably identified (Fig. 8.7).
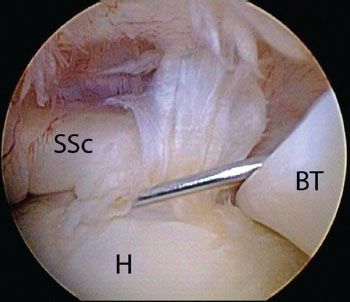
Figure 8.5 Right shoulder, posterior viewing portal with a 70° arthroscope demonstrates use of a spinal needle as a guide to create an anterosuperolateral working portal with a 5° to 10° angle of approach to the lesser tuberosity. BT, biceps tendon; H, humerus; SSc, subscapularis tendon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








