CHAPTER 3 Arthroscopic Management of Tibial Plateau Fractures
ANATOMY
As reviewed by Lubowitz and colleagues,1,2 the knee is anatomically designed well to achieve its function—providing stability, bending and rotational range of motion, and transmission of load. The tibia is the major weight-bearing bone of the knee joint. At its proximal articular surface, the tibia widens to form medial and lateral condyles. Between the condyles, the intercondylar eminence serves as the attachment for the menisci and the anterior and posterior cruciate ligaments. The relatively flattened condylar portions of the proximal tibia compromise the weight-bearing aspects of the plateau. The medial and lateral condyles articulate with corresponding medial and lateral femoral condyles.
PATIENT EVALUATION
History and Physical Examination
Classic patient history is trauma as a result of a fall or motor vehicle versus a pedestrian accident.1,2 Tibial plateau fractures are common in sports, particularly in skiers. Avulsion fractures commonly occur in children and adolescents, with 50% caused by a fall from a bicycle. However, it is sometimes misunderstood that this condition occurs only in the young. Although less common, ACL avulsion also occurs in adults.
Diagnostic Imaging
Standard radiologic knee trauma views usually reveal plateau fractures, but displaced fractures and compression fractures can be missed. X-rays are not accurate for determining the amount of depression when a compression fracture component is visible. Computed tomography (CT) with three-dimensional reconstruction provides precise information regarding the extent and pattern of articular and extra-articular components of the fracture. In addition to CT scanning to assess bony pathology, magnetic resonance imaging (MRI) is also recommended. MRI is the examination of choice for soft tissue injuries associated with tibial plateau fractures.
TREATMENT
Indications and Contraindications
The key point is that surgery is generally indicated based on fracture classification. The Schatzker classification of tibial plateau fractures is illustrated in Figure 3-1. I recommend ARIF for all type III fractures, and ARIF should be considered for types I, II, and IV fractures. Arthroscopy-assisted surgery for Schatzker type V and VI fractures (skin incision and plating, with arthroscopy but no arthrotomy), can also be considered. Chen and associates3 have reported 85.1% and 90% satisfactory results for types V and VI fractures, respectively (Table 3-1).
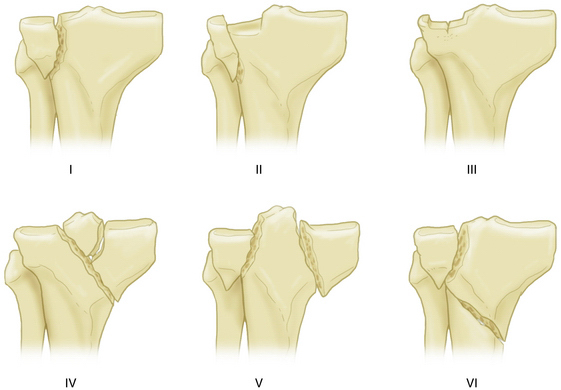
FIGURE 3-1 Schatzker classification of tibial plateau fractures.
(Adapted from Lubowitz J, Elson W, Guttmann D. Part I: arthroscopic management of tibial plateau fractures. Arthroscopy. 2004;20:1063-1070.)
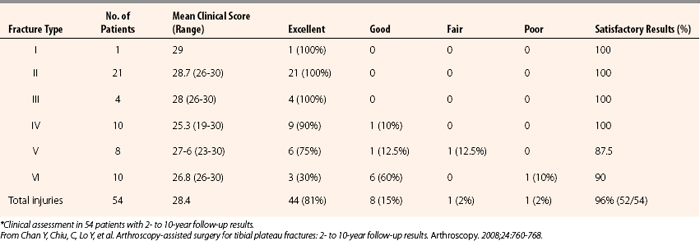
TABLE 3-1 Results of Arthroscopic Reduction and Internal Fixation of Schatzker Types V and VI Tibial Plateau Fractures*
The Meyers and McKeever classification of tibial intercondylar eminence fractures is illustrated in Figure 3-2. Surgery is indicated for type I fractures if they are associated with meniscus tears or other concomitant pathology that requires arthroscopy. Otherwise, these may be immobilized at or near full extension. Aspiration of hemarthrosis may result in substantial pain relief. There is sufficient evidence that surgery should be strongly considered for type II bird’s beak pattern fractures because of the high association of anterior horn of the medial (or occasionally the lateral) meniscus lodged within the fracture site.2,4–7 Closed reduction may be attempted for large type IIIB fractures because associated condylar contact may allow bony reduction after aspiration and hyperextension. For displaced type III fractures, ARIF is the state of the art procedure.2
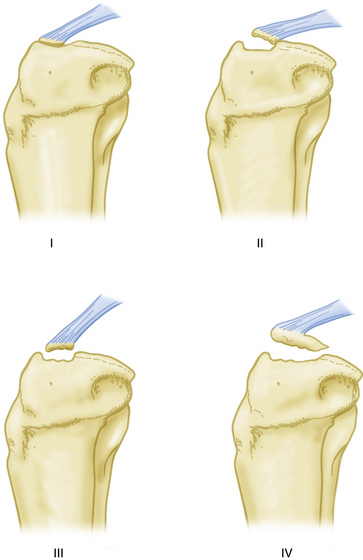
FIGURE 3-2 Meyers and McKeever classification of tibial plateau fractures.
(Adapted from Lubowitz, J, Elson, W, Guttmann, D. Part II: arthroscopic treatment of tibial plateau fractures: intercondylar eminence avulsion fracture. Arthroscopy. 2005;21:86-92).
An impressively large series by Chan and coworkers3 is summarized in Table 3-1. The key point is that fracture types I, II, III, and IV had 100% satisfactory results. Fracture type V had 87.5% satisfactory results and Schatzker type VI had 90% satisfactory results.
Hunter and Willis8 have described the outcome of suture or screw fixation of Myers and McKeever types II and III tibial intercondylar eminence fractures. At 32.6-month follow-up, the mean Tegner score was 6.35 and mean Lysholm score was 94.2. The best outcomes were seen in younger patients. No significant differences were seen in outcome with regard to type of fixation.
Conservative Management
As noted,1 not all fractures of the tibial plateau require surgery. Fractures that are stable and minimally displaced may be amenable to cast immobilization, or bracing may allow early motion (but with delayed weight bearing). Other indications for nonoperative treatment may include injuries to the peripheral (submeniscal) rim of the plateau, a unique fracture pattern, and fractures in older adult, low-demand, or osteoporotic patients. Meyers and McKeever type I tibial intercondylar eminence fractures may be immobilized near full extension. Aspiration may relieve pain in patient with intense hemarthrosis.








