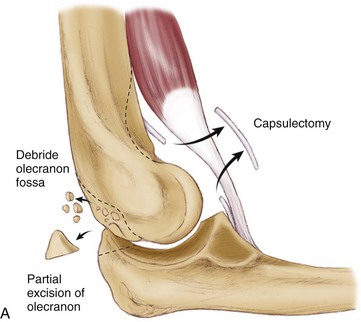
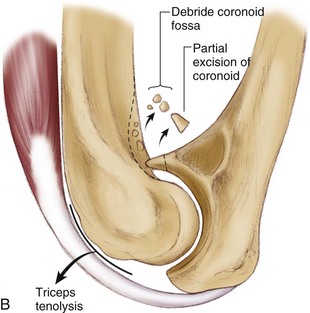
Chapter 42 Loss of mobility represents the most common complication of elbow trauma. The predisposition of the elbow to develop posttraumatic contracture has been attributed to several factors, including the intrinsic congruity of the ulnohumeral articulation, the presence of three articulations within a synovium-lined cavity, and the intimate relationship of the capsule to the intracapsular ligaments and extracapsular muscles.1–3 Several authors have evaluated the elbow motion necessary to complete daily activities; these studies have reported that a majority of activities could be reasonably performed within a functional arc of 100 degrees (30 to 130 degrees) of flexion and extension of the elbow and 100 degrees of rotation of the forearm (50 degrees each for pronation and supination).4 The inability of the elbow to achieve this motion after the occurrence of trauma may result in substantial impairment of upper extremity function, especially with the loss of elbow flexion and forearm supination, which are difficult to accommodate for. Relative contraindications to arthroscopic elbow release include severe elbow contractures with minimal joint motion, prior ulnar nerve transposition surgery, and the presence of significant heterotopic bone; these patients are more reliably treated with extensive open debridement of the elbow to restore motion and protect the ulnar nerve. If there has been previous medial elbow surgery or ulnar nerve transposition and one is considering arthroscopic release, the ulnar nerve should be isolated and protected through a medial exposure before arthroscopy. If the ulnohumeral joint shows marked degenerative changes, a simple release of the joint may not lead to improved motion and may exacerbate pain in an arthritic joint. If advanced posttraumatic arthritis is observed in the ulnohumeral articulation, salvage-type procedures are often required if surgery is undertaken.5 Arthroscopic release of a posttraumatic elbow is a technically demanding procedure that requires intimate knowledge of intracapsular elbow anatomy as well as advanced skills in elbow arthroscopy. Multiple portals are required, and diligent fluid management is essential, especially after capsulectomy when joint distention is more difficult. The use of joint retractors is typically required to achieve adequate visualization and facilitate appropriate surgical debridement.6–10 From a purely mechanical standpoint, to improve elbow extension, posterior impingement must be removed between the olecranon tip and the olecranon fossa. Anteriorly, tethering soft tissues such as the anterior joint capsule and any adhesions between the brachialis and the humerus must be released. Similarly, to improve elbow flexion, the surgeon must release any soft tissue structures posteriorly that may be tethering the joint. They include the posterior joint capsule and the triceps muscle, which can become adherent to the humerus. The surgeon must remove any bony or soft tissue impingement anteriorly, including any soft tissue overgrowth in the coronoid and radial fossae. There must be a concavity above the humeral trochlea and capitellum to accept the coronoid centrally and the radial head laterally for full flexion to occur (Fig. 42-1). We typically favor a regional block, although general anesthesia may also be considered. We then position the patient in the lateral decubitus or prone position with the affected extremity facing up and all bony prominences well padded. A rolled blanket or elbow stirrup attachment for the operative table is positioned underneath the arm, allowing the elbow to move from 90 degrees of flexion to full extension. The video monitor, shaver system, camera control unit, and light source are positioned such that the surgeon has a clear view of the monitor. After the extremity has been sterilely prepared and draped up to the axilla, the hand and forearm are wrapped with an elastic bandage to limit fluid extravasation and a sterile pneumatic tourniquet is placed as proximally as possible around the arm (Fig. 42-2).
Arthroscopic Management of Elbow Stiffness
Preoperative Considerations
Indications and Contraindications
Surgical Technique
Anesthesia and Positioning
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Arthroscopic Management of Elbow Stiffness