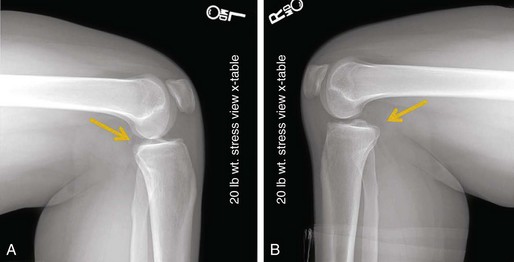
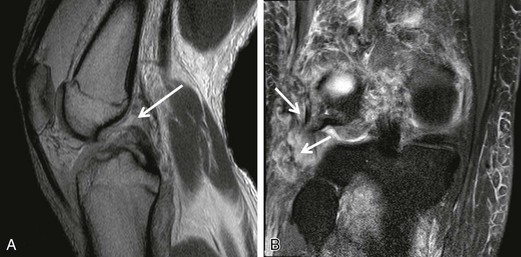
Chapter 81 Posterior cruciate ligament (PCL) injuries are infrequent; however, their treatment remains a difficult clinical problem for the treating orthopedic surgeon. Although clinical outcomes of PCL deficiency are not uniformly poor, recent studies suggest that the kinematics of the PCL-deficient knee are significantly altered from the intact state.1,2 In similar fashion to that in the anterior cruciate ligament–deficient knee, PCL deficiency redirects the forces across the knee joint.1,2 The resultant increase in pressure in the medial and patellofemoral compartments may lead to premature and severe arthrosis.3 In an attempt to restore normal stability to the symptomatic knee, most authors advocate reconstruction of the PCL. There are multiple surgical options for PCL reconstruction, with no gold standard technique. The purpose of this chapter is to present the clinical presentation of, diagnostic approach to, and surgical treatment for injury to the PCL. Furthermore, the technical aspect is focused on the double-bundle arthroscopic inlay surgical technique, because this surgical technique is currently the senior author’s (J.K.S.) preferred technique for PCL reconstruction. After discussion of the technical aspects, by way of a review of the current literature we will discuss the advantages of the double-bundle arthroscopic inlay PCL reconstruction and provide evidence as to why this is our advocated and chosen surgical technique for reconstruction of the PCL. In the acute setting there is often a history of a direct blow to the pretibial aspect of the lower extremity or a hyperextension injury to the affected knee. An effusion or swelling is often present with an acute PCL injury. A knee dislocation often results in injury to the PCL, which is likely associated with concomitant ligamentous or soft tissue injuries. In the case of severe knee trauma, 95% of patients with a PCL injury have associated ligamentous injuries. The most common associated injury is disruption of the posterolateral knee structures (approximately 60%).4 In the case of chronic PCL injuries, patients may report pain and instability with activity. On physical examination it is crucial to assess the neurovascular status of the affected limb. This is of particular importance if there is suspicion for or history of knee dislocation. Once the neurovascular competence of the injured limb has been confirmed, inspection and palpation of the knee for effusion are performed. Next, the knee should be passively taken through a range of motion, and, if the patient is capable, passive range of motion should be compared with active range of motion. The relationship of the tibial plateau and femoral condyles as well as the natural tibial step-off can be assessed with the knee in a flexed position. The Godfrey test is used to assess for a posterior sag and is performed with the lower leg elevated and the knee flexed to 90 degrees (Fig. 81-1). A posterior drawer test is also performed in 90 degrees of flexion and can evaluate the amount of posterior tibial translation. Often with traumatic PCL injury a concomitant posterolateral corner (PLC) injury is present as well. This injury pattern can be evaluated with a reverse pivot test, dial test, posterolateral drawer test, and varus stress testing at both 30 and 90 degrees of flexion. Plain radiographs (anteroposterior and lateral) of the knee are helpful in that they can rule out fracture in the acute setting and medial or patellofemoral compartment arthrosis in the chronic setting. Long-leg standing films should be obtained if any fixed or dynamic instability is suspected. Posterior tibial subluxation can be evaluated on standard lateral radiographs; however, if there is any doubt, bilateral stress radiographs should be obtained (Fig. 81-2). In the setting of a chronically PCL-deficient knee, a bone scan may be useful to identify the extent of degenerative changes that may not be detected on plain radiographs. A magnetic resonance imaging (MRI) study is an essential part of the workup of a PCL injury, not only for confirmation of PCL injury but, more important, for the assessment of associated ligamentous injuries such as those to the PLC that will affect the operative plan and ultimately the clinical outcome (Fig. 81-3). Acute isolated grade I or II PCL injuries may be treated with nonoperative, protected weight bearing and rehabilitation. Grade I or II injuries that go on to cause persistent and recurrent instability may be treated surgically. Surgically reconstructing an acute, isolated PCL tear is indicated for a grade III injury, or in the presence of a bone avulsion injury, although not all authors agree on the existence of an isolated grade III PCL injury.5–7 The majority of acute PCL injuries occur in conjunction with a knee dislocation or a multiligamentous injury necessitating surgical intervention. The timing of intervention remains controversial; however, an acute reconstruction is generally recommended in the presence of a bone avulsion injury or a combined ligamentous injury (especially a PLC injury). There are a number of surgical variables to consider before PCL reconstruction, including graft material, number of bundles, and surgical technique (transtibial versus open inlay versus arthroscopic inlay). A recent systematic review addressed the variable of number of bundles and found that although there are no clinical studies to suggest an advantage of double-bundle grafts, there are distinct biomechanical advantages to the double-bundle PCL reconstruction.8 Most recently, the evolution of the arthroscopic inlay technique has melded the advantages of both the transtibial and open inlay techniques while negating the disadvantages of each technique. For these reasons the double-bundle arthroscopic inlay technique is the PCL reconstruction of choice for the senior author of this chapter (J.K.S.) and is presented here.
Arthroscopic Double-Bundle Tibial Inlay Posterior Cruciate Ligament Reconstruction
Preoperative Considerations
Physical Examination
Radiography
Other Imaging Modalities
Indications and Contraindications
Surgical Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine