CHAPTER 15 Arthroscopic Capsular Plication and Thermal Capsulorrhaphy
Basic science
The surrounding capsular envelope consists of three ligaments: the iliofemoral ligament (i.e., the Y ligament of Bigelow), the pubofemoral ligament, and the ischiofemoral ligament (Figure 15-1). The iliofemoral ligament has a medial and lateral limb proximally, and distally it forms a deep circular band that surrounds the femoral neck in a leash-like fashion; this area is called the zona orbicularis. This “Y ligament” is the strongest, and it prevents the anterior translation of the hip during extension and external rotation when its fibers tighten. In flexion, these fibers loosen, which leads to a “screw home” effect in full extension. The pubofemoral ligament is slightly inferior to the iliofemoral ligaments, and it also controls external rotation in extension. The ischiofemoral ligament is a posterior structure that controls internal rotation in flexion and extension. Other secondary hip stabilizers include the ligamentum teres and the psoas tendon, which may provide important stability in cases of dysplasia or static ligament deficiencies.
Brief history and physical examination
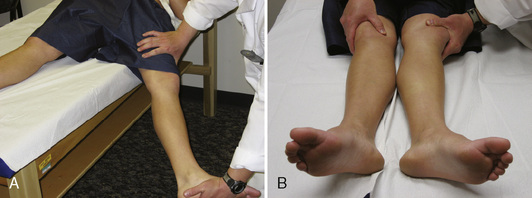
During the physical examination, the patient’s spine should first be examined to rule out other causes of hip pain. This should be followed by an examination of the elbows, hands, and knees to look for signs of hypermobility. Attention should also be paid to the patient’s skin and eyes. Next, the range of motion of both hips should be assessed. These patients often have an increased range of motion as a result of capsular laxity, but any significant increase in internal rotation should heighten one’s suspicion of increased femoral anteversion or other osseous abnormalities. This is followed by a thorough neurovascular examination that includes the reflexes. Next, specific hip testing should be performed, including the Ober test, the bicycle test, the psoas test, and the impingement test. In many cases, this process alters dynamic stabilizers (e.g., the iliopsoas) and leads to psoas and flexion contractures, internal coxa saltans, low back pain, and sacroiliac joint pain. Finally, hip-specific testing for capsular laxity should be performed. Patients with this condition will usually experience anterior hip pain while in the supine position with passive hip extension and external rotation (Figure 15-2, A). Patients may also have increased external rotation in full extension and distraction on the affected side (see Figure 15-2, B). Philippon and colleagues classified capsular laxity on the basis of these physical examination findings from grade 1 (mild) to grade 4 (severe), with grade 4 representing collagen vascular diseases.
Imaging and diagnostic studies
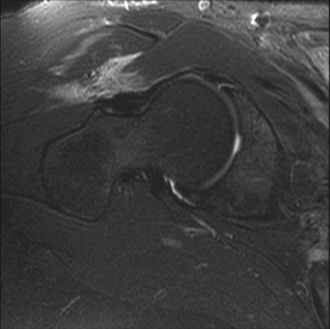
Magnetic resonance imaging (MRI) is critical for the evaluation of atraumatic instability. In the acute setting of traumatic hip injuries, numerous studies have demonstrated that MRI may aid in the diagnosis of chondral injuries, loose bodies, labral tears, femoral head contusions, sciatic nerve injuries, and ligament disruptions. Likewise, in the setting of chronic atraumatic injuries, MRI is also very useful to find subtle derangements in capsulolabral structures (Figure 15-3) as well as osteonecrosis.
Indications
Surgical technique
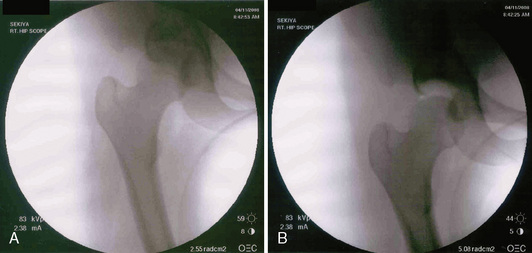
At this point, both of the patient’s feet are well padded, and the patient’s extremities are well secured to the fracture table. A well-padded perineal post is placed in between the patient’s extremities. The nonoperative limb is placed in full extension and mild abduction and then in minimal traction. The operative limb is put through a traction maneuver, which consists of abduction around the perineal post, axial traction, and adduction. Appropriate traction is then confirmed fluoroscopically. In cases of capsular laxity, minimal traction is usually needed to adequately distract the joint (Figure 15-4). The limb is then placed in internal rotation, which decreases the amount of hip distraction, reduces femoral anteversion, and subluxes the femoral head anteriorly, which enables the easy instrumentation of the joint. At this point, traction time is noted and documented.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree