CHAPTER 2 Arthroscopic and Open Anatomy of the Hip
Introduction
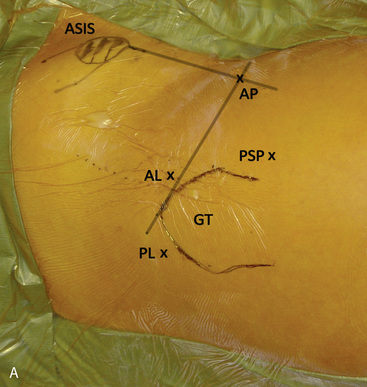
Several bony landmarks define the surface anatomy of the hip. The anterosuperior iliac spine (ASIS) and anteroinferior iliac spine (AIIS) are located anteriorly, with the former being palpable. These structures serve as the insertion points for the sartorius and the direct head of the rectus femoris, respectively. Posterolaterally, two bony landmarks are palpable: the greater trochanter and the posterosuperior iliac spine. The greater trochanter serves as the insertion point of the tendon of the gluteus medius, the gluteus minimus, the obturator externus, the obturator internus, the gemelli, and piriformis. The posterosuperior iliac spine serves as the attachment point of the oblique portion of the posterior sacroiliac ligaments and the multifidus. During arthroscopic and open access to the joint, both of these landmarks are useful tools for incision planning, and, in combination with the anterior bony prominences, for initial orientation (Figure 2-1, A).
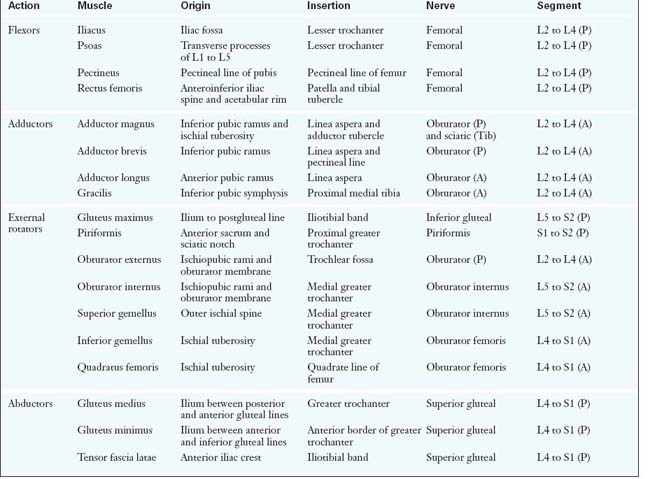
There are a total of 27 muscles that cross the hip joint. They can be categorized into six groups according to the functional movements that they induce at the joint: 1) flexors; 2) extensors; 3) abductors; 4) adductors; 5) external rotators; and 6) internal rotators. Although some muscles have dual roles, their primary functions define their group placement, and they all have unique neurovascular supplies (Table 2-1).
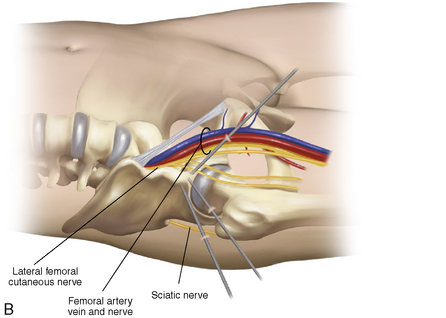
The vascular supply of the hip stems from the external and internal iliac arteries. An understanding of the course of these vessels is critical for avoiding catastrophic vascular injury. In addition, the blood supply to the femoral head is vulnerable to both traumatic and iatrogenic injury; the disruption of this supply can result in avascular necrosis (Figure 2-2).
Hip musculature
Abductors
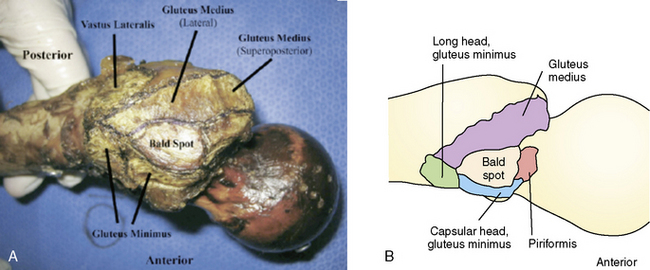
The abductors consist of the gluteus medius and gluteus minimus muscles. Both of these muscles are innervated by the superior gluteal nerve (i.e., the posterior division of L5 to S2). The TFL and the iliotibial band also contribute to hip abduction. This action is only apparent with the hip in a flexed position, and the TFL and the iliotibial band are therefore considered secondary abductors. The gluteus medius, which is the primary hip abductor, originates at the posterior external table of the iliac wing. It is completely covered by the overlying gluteus maximus as it travels distally toward its insertion at the lateral and superoposterior facet of the greater trochanter (Figure 2-3, A). The gluteus minimus fibers run in close approximation to the lateral hip capsule, onto which some of the muscle may also insert. These fibers are often the first to be encountered during hip arthroscopy procedures when establishing the anterolateral portal. The gluteus minimus, which is responsible for 25% of abduction power, runs in the same plane deep to the gluteus medius. It inserts more anteriorly on the greater trochanter, and it has a separate long head component. Recent evidence suggests that a common cause of lateral hip pain may be tears of the hip abductor insertion and not simply trochanteric bursitis. These tears are referred to as rotator cuff tears of the hip. Anatomic restoration of the insertion of the torn gluteus medius can be achieved with standard arthroscopic technique in the recently described peritrochanteric compartment. When trochanteric bursitis does exist in isolation, it is most likely located at the posterior facet or the bald spot of the trochanter (see Figure 2-3, B).
External and Internal Rotators
The external rotators include the obturator internus, the obturator externus, the superior and inferior gemelli, the quadratus femoris, and the piriformis muscles (see Figure 2-3). These small but powerful musculotendinous units act synergistically to provide the external moments that are necessary to generate lateral and rotational activities. The piriformis is the common denominator of the external rotators, and it serves as an important anatomic landmark during both the posterior approach and the surgical dislocation of the hip.
Neurovascular supply of the hip
Vasculature of the Hip
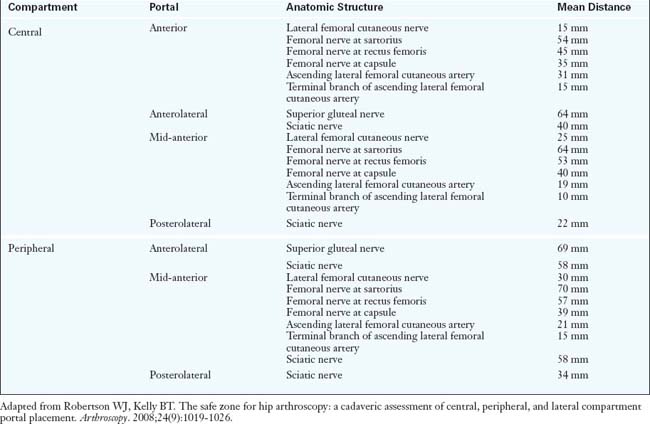
The common femoral artery is the first branch of the external iliac artery, and it traverses just anteromedial to the hip capsule as it travels distally. It is at high risk for damage during both arthroscopic and open anterior approaches to the hip. In fact, the traditional anterior arthroscopic portal is approximately 3.5 cm from the femoral neurovascular bundle (Table 2-2). During total hip arthroplasty (THA), femoral vessel injury and femoral nerve palsy have been described as arising from the incorrect placement of retractors, which can occur with all approaches to the hip. However, because the artery is a large, fairly superficial, and therefore readily palpable vascular structure, its exact location should be routinely identified and thus easily avoided.
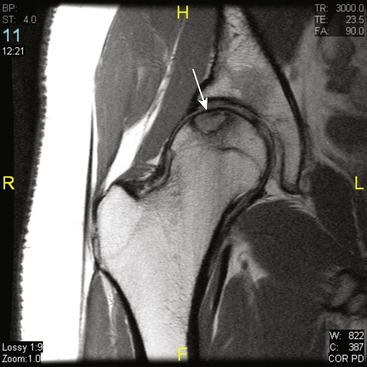
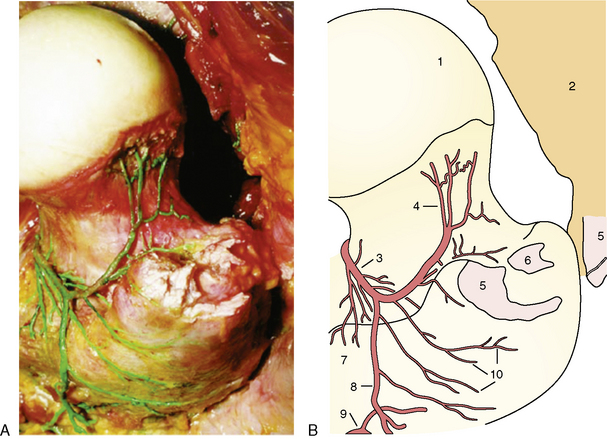
Therefore, the vessel that supplies the majority of the arterial supply to the head is the medial circumflex femoral artery, with varying contributions from the lateral circumflex femoral artery. These vessels branch off at the base of the femoral neck and then ascend toward the femoral head via the posterolateral and posteroinferior synovial retinacular folds (Figure 2-4, A and B). It is believed that disruption at this level (e.g., by a femoral neck fracture) poses the greatest risk for avascular necrosis. The lateral synovial folds, which contain the terminal branches of the medial circumflex femoral artery, can also be injured as a result of aggressive arthroscopic dissection (Figure 2-5) or open approaches. Therefore, they should be routinely identified and protected during peripheral compartment arthroscopy and during open joint-preserving hip surgery.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree