CHAPTER 17 Approach to Chondral Damage in the Patellofemoral Joint
Chondral defects of the patellofemoral joint are the most common type of articular cartilage defect found in the knee.1 They also comprise a significant portion of most isolated grade IV articular cartilage defects in the knee joint. These lesions may be found incidentally but also may be a common source of pain and discomfort in the knee.2 Trochlear articular cartilage defects can be symptomatic. The approach to this joint can be complex and may require a combination of arthroscopic and open surgical techniques, up to and including arthroplasty, which is beyond the scope of this chapter.3,4 I shall primarily discuss arthroscopic techniques for chondral defects.
ANATOMY AND PATHOANATOMY
The patellofemoral joint of the knee is a complex articulation, with multiple facets on the patella and a complex, saddle-shaped trochlear groove.5–7 The articular cartilage on the patella itself is the thickest articular cartilage in the body, measuring up to 7 mm thick on the medial facet. Chondral defects on the patella may be have several causes, including degeneration, direct trauma, malalignment, and patellar instability.8–10 The mechanics of the patellofemoral joint are complex and are determined by a number of factors, including neuromuscular coordination, geometry of the trochlea, overall alignment of the extensor mechanism, including the quadriceps tendon, trochlear groove, and tibial tubercle, and soft tissue restraints such as the medial patellofemoral ligament.3,11–13 These restraints help guide patellofemoral motion and often determine whether articular cartilage damage occurs and is symptomatic. For example, excessive patellar malalignment with a laterally tilted and subluxated patella can contribute to excessive articular cartilage wear on the lateral facet of the patella.14,15 Direct trauma to the patella, such as from a dashboard-type injury, in which a flexed knee contacts the dashboard, may result in a central articular cartilage damage to the patella or trochlea.16–19 In addition, many central articular cartilage defects are noted in young athletic individuals. These often have a linear fissure in the center of the trochlea. This reflects the significant forces placed on the patellofemoral joint during activities of daily living and other forms of physical exertion. For example, the joint reaction forces on the patellofemoral joint during stair climbing are up to two to four times body weight, and jumping can create forces up to six to eight times body weight.20–25 These loads can result in failure of the underlying articular cartilage and subchondral bone.
PATIENT EVALUATION
History and Physical Examination
Patients with symptomatic articular cartilage lesions of the patellofemoral joint generally complain of anterior knee pain, particularly when ascending or descending stairs or after sitting.4 Occasionally, patients may complain of crepitus or a symptomatic click as the knee goes into flexion or extension. Elements of the history to obtain from the patient also include known or suspected rheumatologic disease, history of trauma to the knee from a direct blow, history of patellar instability, activity level of the patient, recent changes in activity level, timing of the injury, and whether the pain is acute or chronic. In patients who have already sought previous treatment, it is important to identify the nature of treatment, including physical therapy, bracing, and taping and any previous surgery. Complaints of recurrent or consistent effusions should also be identified. Knee pain diagrams often provide relevant clinical information.26
Physical examination should combine static and dynamic evaluation. The presence or absence of any effusion should be noted and the knee should be carefully palpated and evaluated for ligamentous and patellar instability. At 30 degrees of knee flexion, the patella will typically translate laterally approximately 9 mm and have a relatively firm end point because of the check rein of the medial patellofemoral ligament.27 The patella should also translate medially 7 mm and the lateral patellar retinaculum should allow the patella to be tilted to a neutral position, where the anterior surface of the patella is parallel to the ground while the patient is supine. Quadriceps development, particularly that of the vastus medialis obliquus muscle, should be assessed.4 Extensor alignment including femoral version, Q angle, and tibial rotation can provide insights into patellar tracking.
Dynamic examination of the knee should be performed as well. Abnormalities of gait should be identified.28 Evaluation of knee stability and identification of pain or crepitus while doing a step-up or step-down maneuver may help elicit specific complaints. A single leg squat test may also elicit pain and will allow evaluation of relative knee valgus or internal rotation, which can increase patellofemoral forces.
Diagnostic Imaging
Radiography
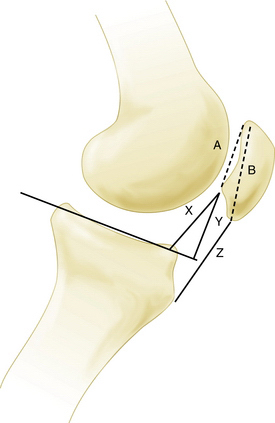
A true lateral view with overlapping femoral condyles, with less than 5% displacement, can provide valuable information regarding the relative patellar height. This can be assessed using various ratios, including the Insall-Salvati index and Blackburne-Peel method (Fig. 17-1)—the articular surface length compared with the distance from its inferior margin to the tibial plateau. This technique has been demonstrated to be the most reliable. A true lateral view can also yield information about the degree of trochlear dysplasia. The trochlear groove can be identified on the lateral x-rays, on which a dense white line of the trochlea should not intersect vvthe bone of the lateral femoral condyle (Fig. 17-2). A sunrise or Merchant view at 45 degrees of flexion can give indicate patellar tracking within the trochlea and the presence of lateral patellar tilt or subluxation. A number of measurements have been described; however, I agree with Merchant that “(f)or most patients, it is quicker and just as good to eyeball the film rather than spend time drawing lines and calculating measurements.”29
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is currently the best modality to image articular cartilage defects.30,31 Appropriate articular cartilage sequences and thin cuts often reveal articular cartilage damage, such as chondromalacia, chondral flaps, or delamination. In addition, it can also identify areas of underlying subchondral bony edema. MRI is also useful to assess abnormalities of soft tissue that may be contributing to underlying chondral damage or patellofemoral pain, such as synovitis, lesions of the medial patellofemoral ligament, tendinopathy, and articular cartilage loose bodies. MRI can also be used to perform measurements of tibial tubercle to trochlear groove distance. This can indicate conditions that could lead to patellar instability and subsequent articular cartilage damage.