CHAPTER 20 Anterior Cruciate Ligament Repair
Anterior cruciate ligament (ACL) repair is not a new idea, having first been reported by the Mayo Robinson in 1885.1 Prior to 1970, little emphasis was given to repairing the ACL. Most techniques centered on repairing extra-articular structures with the idea that a competent ACL was not required for normal knee function. Conservative treatment of ACL tears resulted in poor healing rates and a high incidence of instability.2,3 Primary repair alone did not improve results.4–6 Reasons for this lack of healing potential were thought to be lack of blood clot formation, insufficient blood supply, differences in intrinsic cell migration, impaired growth factor ability, and the effect of synovial fluid on cell morphology.7,8
In the 1970s, Marshall and colleagues9 increased interest in repairing ACL tears; their technique used primary suture repair. Good results with the repair of proximal tears were obtained. Two randomized studies2,3 have shown no difference in functional outcomes between repair and conservative treatment with about one third in each group having residual instability. Subsequent focus centered on reconstruction of the torn ACL rather than repair.10 With better understanding of ACL anatomy, including ligamentous function and insertion footprint anatomy, interest in repair of the ACL has resurfaced. Recent basic science research11–15 looking at growth factors, gene therapy, and tissue-friendly scaffolds has shown promise for future progress in ACL repair.
ANATOMY
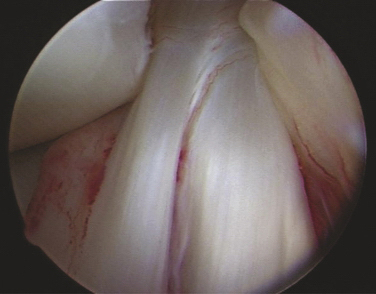
The ACL has been described anatomically in two bundles, one anterior medial (AM) and one posterior lateral (PL; Fig. 20-1). Whereas the primary function of the larger anterior medial bundle is to resist anterior translation of the tibia on the femur, the posterior lateral bundle also resists abnormal anterior lateral rotation of the tibia on the femur.
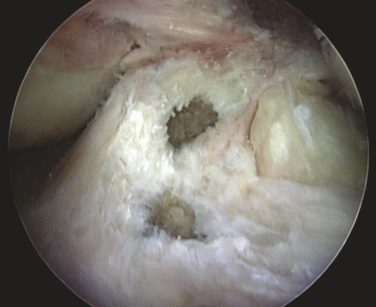
This attention to multiple ligamentous fiber attachment sites has led to the concept of ACL femoral and tibial footprints (Fig. 20-2). A goal of preserving or reconstructing attachment sites corresponding to the footprints should more closely restore the natural function of the ACL.
The ACL arises from a fossa in front of and lateral to the anterior spine in a footprint that averages 11 mm medial to lateral and 17 mm front to back.16 Its average length is 38 mm, with a width of 10 mm in its midpoint. It inserts on the posterior medial surface of the lateral femoral condyle. Its blood supply is via the middle geniculate artery and it is innervated by branches of the tibial nerve.
PATIENT EVALUATION
History and Physical Examination
Have the patient lie supine, close to the edge of the examination table. Rest the heel of the patient’s injured extremity just off the edge of the table, with the calf fully supported on the table (Fig. 20-3A). This position will allow about 10 degrees of knee flexion and usually the thigh muscles will relax. Accessing the presence of even a small effusion is easy by gently pushing side to side on each side of the patella. Performing a Lachman test is also enhanced by this position, along with medial and lateral stability (see Fig. 20-3B).
Next, while seated, gently abduct the hip and flex the knee off the side of the bed to 90 degrees. Keeping the thigh on the table, stabilize the foot between your knees (see Fig. 20-3C). Grasping the proximal tibia with both hands allows a gentle posterior drawer test to be performed.
Bring the knee to 25 degrees of flexion and, with both hands, a quick jerk forward will usually detect the presence or absence of an end point. This maneuver is especially helpful with large patients in whom a routine Lachman test is difficult to perform simply because of the size of the leg or the presence of muscle spasm (see Fig. 20-3D).
Diagnostic Imaging
Every examination of the knee should include at least four high-quality x-rays—standing anteroposterior (AP) at 0- and 30-degree, lateral, and sunrise patellar views. Subtle bony injuries such as articular and Segond fractures17 can be identified. A rim fracture of the patella or lateral femoral condoyle can be helpful in differentiating between a patella dislocation and acute ACL tear, both of which may present with hemarthrosis and muscular spasm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree