Anterior Cruciate Ligament Reconstruction with Patellar Tendon Autograft: Principles of Rehabilitation
K. Donald Shelbourne MD
Camiron Pfenning MD
Scott E. Lawrance MS, PT, ATC, CSCS
The patellar ligament, more commonly referred to as the patellar tendon, is a strong, thick, fibrous band passing from the patella to the tibial tuberosity.
The anterior cruciate ligament (ACL) provides stability against anterior stress applied to the tibia.
The cruciate ligaments enable the knee to both roll and slide for maximum motion while still maintaining contact and stability.
Most ACL injuries can be diagnosed with a careful patient history, emphasizing mechanism of injury, coupled with good physical examination technique. Diagnostic imaging or procedures usually are not necessary to establish the diagnosis of an ACL tear but can be useful when assessing menisci, subchondral bone, and other ligamentous structures.
Although a variety of mechanisms can lead to an ACL tear, sports competition against another player that involves twisting, jumping, pivoting, cutting, and landing unpredictably, together with sudden changes in direction, exposes the ACL to injury.
After an ACL tear, the patient will walk with a bent-knee gait if he or she is able to tolerate any weight-bearing activity. It also is common to observe that the patient will have difficulty lifting the leg onto the examining table.
After examining the ACL, the other cruciate ligaments need to be assessed. Injury to the medial and/or lateral meniscus also is common when the ACL is torn, with a 69% incidence of meniscal injury after an acute ACL tear.
If the diagnosis is still in question after a thorough history and a complete physical examination, the immediate approach involves reducing the athlete’s pain and swelling and then reevaluating a few days later. An ACL tear does not require immediate surgery; rather, it involves minimizing patient discomfort and restoring full range of motion, regardless of the ultimate treatment decision.
With the appropriate rehabilitation process and long-term exercise program, many patients can maintain an active lifestyle with an ACL-deficient knee. This option is most appropriate for those individuals who do not participate in recreational sports activities or engage in other high-risk activities that involve twisting or rotational forces through the lower extremity.
In athletes who choose nonoperative treatment or who want to complete their current season before reconstruction, it is crucial to evaluate the menisci before this type of therapy is allowed. A magnetic resonance imaging (MRI) evaluation is an excellent way to determine the status of the menisci.
If surgery can be delayed without having episodes of instability, a preoperative rehabilitation program can be used and schedules adjusted to perform the surgery under more ideal conditions. This delay in surgery decreases postoperative complications.
Postoperative rehabilitation begins in the operating room with placement of the patellar tendon graft. It is critical that full range of motion, including hyperextension, is achieved at this point to ensure that the graft has not been overtensioned, resulting in a captured joint that prevents full range of motion.
Complications during rehabilitation are much easier to prevent than they are to treat. The patient needs to have a thorough understanding of the goals of each phase of rehabilitation.
This chapter focuses on ACL reconstruction with the patellar tendon autograft and rehabilitation for the ACL injury as well as the graft site. The patellar ligament, more commonly referred to as the patellar tendon, is a strong, thick, fibrous band passing from the patella to the tibial tuberosity.
Anatomy
An understanding of normal knee anatomy is paramount when attempting ACL reconstruction and rehabilitation.
Bony Anatomy
The stability of the knee joint depends on the ligaments that connect the femur and the tibia as well as the surrounding muscles and their tendons. The knee consists of the tibiofemoral joint and the patellofemoral joint composed of three separate bones: (a) the femur superiorly, (b) the tibia inferiorly, and (b) the patella anteriorly. The bones are enclosed in the joint capsule, which is lined with synovium that produces synovial fluid to help protect and nourish the joints. The osseous structures involved in knee anatomy include the patella, the femoral condyles, and the tibial plateaus. The patella is a sesamoid bone that is wider at the proximal end than at the distal end and acts as a fulcrum to assist in extension of the quadriceps muscle. When the knee is extended and the quadriceps muscles are relaxed, the patella can be pushed both medially and laterally so that the underlying facets can be palpated.
Deep to the patellar tendon is the infrapatellar fat pad. The tibiofemoral joint has medial and lateral compartments, corresponding with the medial and lateral femoral condyles, which articulate with the medial and lateral tibial plateaus. In the patellofemoral joint, the patella articulates with the femoral trochlea only. The medial and lateral tibial plateaus are palpable just beneath their corresponding femoral condyles. Laterally, just below the tibial joint line, is the Gerdy tubercle, which is the attachment site for the iliotibial band.
Musculature
The musculature of the knee includes the quadriceps, sartorius, gracilis, and semitendinosus muscles. The quadriceps mechanism proximal to the patella consists of the vastus lateralis, rectus femoris, vastus intermedius, and vastus medialis. The vastus medialis obliquus, which is the most distal and medial part of the vastus medialis, consists of obliquely oriented fibers attached to the patella. Broad, fibrous medial and lateral patellar retinacula expand on both sides of the patella and attach to the iliotibial band laterally and to the vastus medialis obliquus medially. The quadriceps muscles function principally in extension, but the hamstrings are involved in the flexion mechanism. The sartorius, gracilis, and semitendinosus muscles help to protect the knee against rotatory and valgus stress.
Ligaments
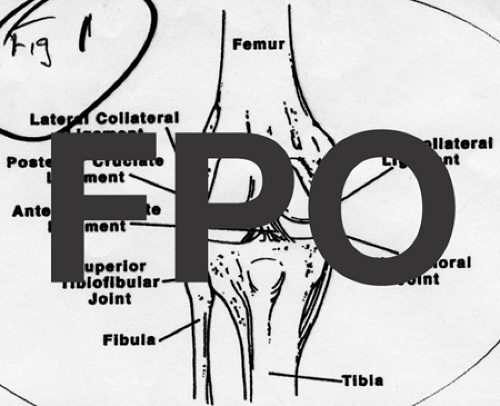
Four major ligaments are involved in knee stability. The posterior cruciate ligament (PCL) provides stability against posterior stress applied to the tibia, and the ACL provides stability against anterior stress applied to the tibia. The lateral collateral ligament (LCL) provides lateral stability against varus stress, and the medial collateral ligament (MCL) provides medial stability against valgus stress. Although this chapter focuses primarily on ACL injuries, it is important to understand the interactions between all the ligaments of the knee joint (Fig 44-1).
The cruciate ligaments criss-cross within the center of the joint and join the femur and the tibia. The PCL originates on the lateral aspect of the medial femoral condyle and attaches behind the intercondylar area of the posterior surface of the tibia. When the knee is flexed and weight bearing, the PCL tightens and provides stabilization. On the other hand, the ACL originates on the tibial plateau both anterior and lateral to the medial tibial spine, and it inserts onto the medial aspect of the lateral femoral condyle. The ACL is composed of an anteromedial band and a posterolateral band, which are named based on their tibial attachment sites. When the knee is fully extended, the ACL is taut to prevent posterior displacement of the femur on the tibia and hyperextension of the knee joint. Medial stability is provided
statically by the MCL. From anterior to posterior, the lateral structures of the knee are the iliotibial band, lateral capsule, popliteus, LCL, biceps femoris, and lateral head of the gastrocnemius. All these structures contribute to lateral stability. The superficial MCL runs from the medial epicondyle, crosses the joint line, and can be palpated medially, on the posterior half of the medial aspect knee. The deep MCL is not palpable as a discrete structure.
statically by the MCL. From anterior to posterior, the lateral structures of the knee are the iliotibial band, lateral capsule, popliteus, LCL, biceps femoris, and lateral head of the gastrocnemius. All these structures contribute to lateral stability. The superficial MCL runs from the medial epicondyle, crosses the joint line, and can be palpated medially, on the posterior half of the medial aspect knee. The deep MCL is not palpable as a discrete structure.
Menisci
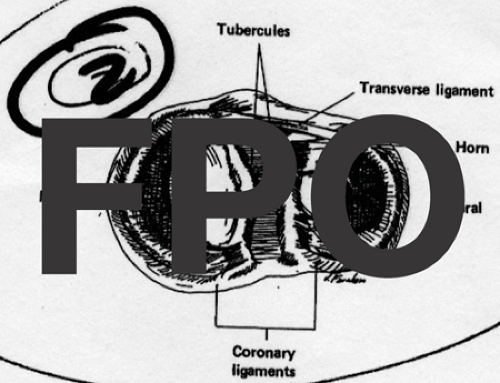
The menisci are crescent-shaped, fibrocartilaginous structures that lie between the hyaline cartilage surfaces of the femur and the tibia. Inferiorly, the menisci attach to the tibia via the coronary ligaments. The lateral meniscus is nearly circular and covers more of the tibial articular surface than the medial meniscus does (Fig 44-2).
Biomechanics of the Knee
The overall motion of the knee is controlled by interactions between ligaments, other supporting soft-tissue structures, and constraints of the articular surfaces. Unfortunately, when structures become damaged, the overall motion of the knee usually is altered. To understand injury mechanisms and to develop rehabilitation protocols for knee injuries, it is important to look at the basic biomechanics of the individual ligaments, the interaction between the ligaments, the role of the meniscus, and the functions of the patellofemoral joint.
The cruciate ligaments enable the knee to both roll and slide for maximum motion while still maintaining contact and stability. If knee flexion involved purely a sliding motion, then the femur would strike the posterior tibial plateau and limit flexion. Conversely, if knee flexion involved only a rolling motion, then the femur would roll off the back of the tibia. Fortunately, the ACL and PCL enable the knee to perform important movements. Knee flexion is limited by a combination of ligaments as well as leg and thigh muscles, but extension is limited by the ligaments, the joint capsule posteriorly, and joint compression.
The ACL is the primary restraint against anterior tibial translational force, providing 85% of the anterior restraining force at 90 degree of flexion (1). The posterolateral bundle of the ACL is tight in extension, whereas the anteromedial bundle of the ACL in tight in flexion. The PCL provides 94% of restraint against posteriorly directed force at 90 degree of flexion. Together, the ACL and PCL are secondary stabilizers and provide some resistance to varus stress if the primary lateral structures have been disrupted.
The menisci are important for transmitting load across the knee and for distributing forces throughout the underlying articular cartilage. They increase the contact surface area between the round femoral condyles and the relatively flat tibial plateau on the medial side and the convex tibial plateau on the lateral side. When all or part of the meniscus is removed, the contact pressure between the femur and the tibial articular surfaces increases and may predispose patients to early joint surface wear (2). During normal walking, which causes knee-joint forces of two- to fourfold normal body weight, menisci bear 40% to 50% of the total load transmitted across the joint in extension and 85% of the compressive load at 90 degree of flexion. On the medial side, load is shared equally between the medial meniscus and the articular surfaces. The lateral meniscus, however, bears most of the lateral-side load transmission, making degenerative changes after a partial lateral meniscectomy more common than after a partial medial meniscectomy.
Depending on the type of activity, the forces across the patellofemoral joint vary. The patellofemoral joint increases the lever arm and, therefore, increases the efficiency of the quadriceps muscle. This joint also allows the quadriceps force to be transmitted around an angle without significant loss of energy from friction. In addition, the patellofemoral joint provides functional knee stability under load with the patella’s opposing force against the distal femur.
History
When clinically evaluating an athlete with an acute knee injury, it is helpful to obtain a clear and concise history and to perform a thorough and accurate physical examination. Most ACL injuries can be diagnosed with a careful history, emphasizing mechanism of injury, coupled with good physical examination techniques. Diagnostic imaging or procedures usually are not necessary to establish the diagnosis of an ACL tear but can be useful when assessing menisci, subchondral bone, and other ligamentous structures. In addition to listening to the athlete’s recollection of the injury, encourage the athlete to include information such as his or her year in school, position played in the particular sport, additional athletic activities, and future athletic aspirations; this information will help to guide treatment decisions (3).
Although a variety of mechanisms can lead to an ACL tear, sports competition against another player that involves twisting, jumping, pivoting, cutting, and landing unpredictably, together with sudden changes in direction, expose the ACL to injury. Fetto and Marshall (4) described two basic mechanisms of injury: (a) a valgus force applied to a flexed knee with the leg in external rotation, and (b) hyperextension of the knee with the leg internally rotated. The incidence of ACL injury is higher among people who participate in high-risk sports, such as basketball, football, skiing, and soccer. For example, a college football player may have as much as a 16% chance of an ACL injury during his 4-year career (5). On the contrary, ACL tears are uncommon in hockey, because these athletes do not fix their feet to the ground. When comparing all sports, noncontact mechanisms account for more ACL tears than contact mechanisms do (6).
An ACL injury typically is described as a major, unexpected, traumatic event that forced the athlete to the ground. Athletes immediately indicate that they experienced a “big-deal” injury, and few will be able to continue participation in the game secondary to pain, swelling, and instability of the knee. In fact, in most cases, the officials will pause the game, and the athlete will require assistance getting off the field. Generally, no reason exists to perform a knee examination on the playing field; it is more important to recognize the typical patterns of injury to further direct evaluation and treatment.
 Fig 44-3. The patient’s knee after an acute anterior cruciate ligament injury usually will develop a hemarthrosis and will lack full extension. |
Frequently, an athlete will describe the injury as the sensation of hearing or feeling a “pop” when the knee “came apart” or “gave away.” If evaluated within the first 12 hours after injury, the athlete often will have a hemarthrosis along with difficulty in weight-bearing activities. An athlete with an ACL injury likely will have difficulty achieving full knee extension, because the ACL stump does not fit in the intercondylar notch. The majority of knees that have a traumatic hemarthrosis (i.e., an intra-articular accumulation of blood in the joint) will have injury to the ACL (Fig 44-3) (7).
Most ACL injuries will be diagnosed based on the history described above. It is important, however, to broaden your knowledge about the minority of patients who may have atypical presentations. Some patients may suffer an ACL injury secondary to less significant trauma and only have a minimal hemarthrosis. Athletes with chronic ACL deficiency may describe intermittent locking or may explain situations involving multiple giving-way episodes before their most recent injury that prompted medical care. For these patients with a history of other knee injuries, it is important to delve further into their history to establish an accurate diagnosis before jumping immediately to a surgical procedure.
Physical Findings
Examination of a knee injury can be guided by the history to confirm the suspected diagnosis. After an ACL tear, the patient will walk with a bent-knee gait if he or she is able to tolerate any weight-bearing activity. The patient also commonly will have difficulty lifting the leg onto the examining table. After examining the patient’s gait, both lower extremities must be entirely exposed and well supported beyond the heel to allow an accurate examination. Before examining the injured knee, the physician should obtain a
baseline for comparison by first examining the uninjured knee, which also helps to gain the patient’s confidence.
baseline for comparison by first examining the uninjured knee, which also helps to gain the patient’s confidence.
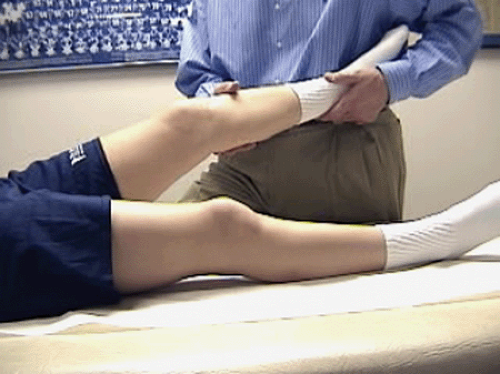
The athlete must be comfortable and relaxed during the examination. The Lachman test, which is the most reliable and reproducible examination method to confirm an ACL injury, should be performed first (8,9). If the Lachman test is performed correctly in an acute setting, it has a sensitivity of 87% to 98% for detecting an ACL tear. Allowing the hip to rotate externally and supporting the knee in slight flexion will facilitate relaxation. One hand should firmly grasp the femur while the other is positioned below the joint, grasping the tibia to allow anterior translation. A quick, firm motion pulling the tibia anteriorly while stabilizing the femur by pushing it posteriorly allows the examiner to appreciate the degree of translation and the quality of the end point. Increased translation and a soft or absent end point compared with an uninjured knee can confirm the ACL injury. It is more important to interpret the Lachman test as positive or negative than it is to quantify the amount of laxity (Fig 44-4).
To perform the Lachman test correctly, the physician must practice and perform numerous knee examinations. Many inexperienced physicians will immediately begin the knee examination with the anterior drawer test (i.e., translation of the tibia forward relative to the femur with the knee in 90 degree of flexion). Torg et al. (10), however, found this test to be positive in only 50% of ACL injuries if the posterior horn of the medial meniscus and/or the posterior capsule were intact. The Lachman test, when performed accurately, is the physical diagnostic test of choice, but the flexion– rotation drawer test also can be performed acutely. This test also is less anxiety-provoking for the patient compared with the classic pivot–shift test. While the physician cradles the calf and flexes the knee, a posteriorly directed force on the tibia will cause reduction of the tibia as the femur rotates from an externally rotated position (Fig 44-5).
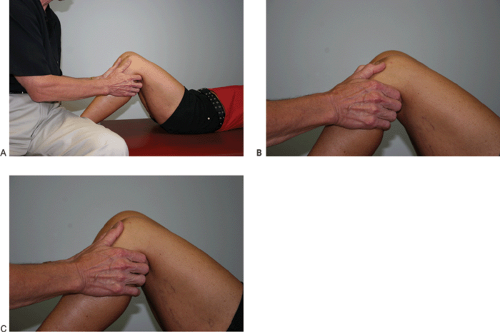
After examining the ACL, the MCL, LCL, and PCL need to be assessed for injury. Testing of the MCL and LCL is performed with the patient’s leg relaxed and the thigh supported by the table. The physician holds the foot with the lower leg off the side of the table and gently stresses the MCL at 30 degree of flexion (Fig 44-6). When testing the LCL, the examiner places a hand behind the knee and uses the other hand to hold the patient’s foot and ankle to stress the LCL at 30 degree of flexion (Fig 44-7). Compared to ACL injuries, PCL injuries are not as common or as disabling but are frequently misdiagnosed. The posterior drawer test is the most sensitive and specific for PCL injury (11). The posterior drawer is performed with the patient lying supine. The hip is flexed approximately
45 degrees, and the foot rests firmly on the evaluating surface. The examiner sits lightly on the patient’s forefoot to stabilize the leg. The proximal calf muscles are cradled in the examiner’s fingers both medially and laterally, with the thumbs resting on the tibial articular landmarks on either side of the patellar tendon. The amount of anterior tibial plateau projecting anterior to the femoral condylar surface is evaluated by direct palpation. The proximal tibia is pushed straight posteriorly with a firm and smooth motion, and the change in alignment of the tibial plateau in reference to the femoral condyles is evaluated (Fig 44-8).
45 degrees, and the foot rests firmly on the evaluating surface. The examiner sits lightly on the patient’s forefoot to stabilize the leg. The proximal calf muscles are cradled in the examiner’s fingers both medially and laterally, with the thumbs resting on the tibial articular landmarks on either side of the patellar tendon. The amount of anterior tibial plateau projecting anterior to the femoral condylar surface is evaluated by direct palpation. The proximal tibia is pushed straight posteriorly with a firm and smooth motion, and the change in alignment of the tibial plateau in reference to the femoral condyles is evaluated (Fig 44-8).
Injury to the medial and/or lateral meniscus is common when the ACL is torn, with a 69% overall incidence of meniscal injury after an acute ACL tear (3). The classic “O’Donoghue terrible triad,” which is described as an ACL, MCL, and medial meniscal tear, is an unusual clinical entity among athletes (12). In fact, a triad of ACL, MCL, and lateral meniscal tear is more common in athletes with a combined injury (13). Meniscal trauma frequently occurs in association with ACL injury, but joint-line tenderness with an acute ACL tear does not necessarily indicate meniscal tears (14).
Imaging
Even though the diagnosis of an ACL injury usually can be established with the combination of a history and physical examination, four plain-film radiographic views are recommended for further assessment. Our routine examination includes a Rosenberg posteroanterior weight-bearing view in 45 degree of flexion (15), bilateral lateral views with 60 degree of knee flexion, and bilateral Merchant patellofemoral views (16). The Rosenberg view is used as a standard technique to better evaluate joint-space narrowing compared with an anteroposterior view. In addition, the posteroanterior view provides an accurate method for evaluating the intercondylar notch width of the femur. We have shown that the incidence of ACL tears is related to notch width as measured radiographically and have confirmed the correlation between our radiographic measurement and our measurement intraoperatively in a series of patients (17,18). We found no significant differences in the ACL tear rates between men and women with notch widths of equal size. Women, however, do tend to have narrower notch widths, which is a possible explanation for why the initial ACL tear rate is higher for women than for men (18).
Most often, plain-film radiographs of patients with an acute ACL injury are normal. In some patients, however, a Segond fracture (i.e., an avulsion fracture from the lateral capsule tearing off the tibia) is seen.
Unfortunately, many MRIs are ordered after an acute knee injury without any proven indication. The accuracy of diagnosing an ACL tear by MRI is high (19), but MRI is not necessary because of the dependability and precision of the history and physical examination. Management rarely is altered by MRI findings, but occasionally, the imaging may influence treatment decisions. At the time of an acute ACL injury, a displaced bucket-handle meniscal tear is uncommon. However, MRI can be useful in the chronic setting, when a patient cannot extend his or her knee after a new giving-way episode, in which a displaced bucket-handle meniscal tear is more common. In addition, MRI can be helpful when a meniscal injury is suspected in a skeletally immature athlete or when an athlete with a likelihood of future meniscal injury desires to return to play with a knee brace. Finally, in patients with chronic ACL deficiency, an MRI can be used to determine the etiology of extension loss.
Decision Making
If the diagnosis is still in question after a thorough history and a complete physical examination, the immediate approach involves reducing the athlete’s pain and swelling and then reevaluating the knee a few days later. This approach often will avoid unnecessary, expensive diagnostic tests, such as MRI, examination under anesthesia, or arthroscopy. Fortunately, an acute ACL tear does not require immediate surgery; rather, involves minimizing patient discomfort and restoring full range of motion, regardless of the ultimate treatment decision. The only reason for doing acute ACL surgery would be when the lateral-side structures are injured, because no reliable reconstructive procedures exist for chronic lateral instability.
Although most individuals who sustain an ACL tear are active in some type of sports activity, their expectations after injury are very broad, depending on their stage of life. Adolescents and younger adults most often want to return to their preinjury sport or level of activity and are unable to do so with an unstable knee. Many older adults, however, may be willing to modify their activities to avoid further injury and, thus, the need for surgical intervention.
Nonoperative Treatment
Reconstruction of the ACL is an elective procedure for most individuals. With the appropriate rehabilitation process and long-term exercise program, many patients can maintain an active lifestyle with an ACL-deficient knee. This option is most appropriate for those individuals who do not participate in recreational sports activities or engage in other high-risk activities that involve twisting or rotational forces through the lower extremity.
The natural history of a knee with an ACL injury is important to consider when determining whether a patient is an appropriate candidate for nonoperative treatment. We have found, as have other investigators, that younger, school-aged athletes with an untreated ACL injury will not be able to participate in most sports without an increased rate of the knee giving way and, thus, are at risk for significant intra-articular damage (20,21). Individuals who have multiple giving-way episodes have a high incidence of subsequent symptomatic meniscal and chondral injuries, with premature degeneration of the joint (22,23). Older patients have a less clearly defined course. In these patients, nonoperative treatment revolves around rehabilitation of presenting symptoms along with activity modification and a dedicated exercise program that maintains good knee function.
Although most school-aged athletes should undergo ACL reconstruction, there is a group, most often because of skeletal immaturity, that will not undergo ACL reconstruction once the knee has returned to a quiescent state. In this group, patient education and avoidance of high-risk sports are critical. Following return of normal range of motion and strength, the athlete often receives a functional knee brace—with a warning that it will not prevent a giving-way episode if he or she returns to cutting and pivoting activities. Previously, knees of preadolescent athletes were stabilized by performing extra-articular reconstructions or primary repair of the ACL, thus avoiding open tibial and femoral growth plates and the potential complication of growth disturbance. These procedures
have not been shown to have better long-term results than those with nonoperative treatment (21,24). Therefore, we feel it is best to wait until the athlete has reached a level of skeletal maturity that allows intra-articular reconstruction when the risk of growth disturbance is minimal.
have not been shown to have better long-term results than those with nonoperative treatment (21,24). Therefore, we feel it is best to wait until the athlete has reached a level of skeletal maturity that allows intra-articular reconstruction when the risk of growth disturbance is minimal.
We use Tanner staging (25), allowing athletes to compare themselves to a series of drawings, along with menstrual history, recent growth history, height of the parents, and serial radiographs demonstrating blurring of the physes to determine when reconstruction is safe. The characteristics of Tanner stages 3 and 4 include the onset of menses, slowing of the preadolescent growth spurt, and radiographs demonstrating blurring of the physes. It is safe to proceed with an intra-articular reconstruction, with little fear of growth disturbance, as long as the procedure is performed so that bony blocks and fixation are not placed across the physes. This approach to surgery may result in the athlete missing one or two seasons of competition (usually at the junior-high level), but most patients usually are compliant with this plan, thus avoiding additional chondral and meniscal injuries. Our results using this criterion and performing an autogenous bone–patellar–bone reconstruction have resulted in no growth abnormalities and excellent clinical results (26).
For athletes who choose nonoperative treatment or who want to try to complete their current season before reconstruction, it is crucial to evaluate the menisci before allowing this course. Magnetic resonance imaging is an excellent way to determine the status of the menisci, because it is noninvasive and does not require ionizing radiation. If repairable meniscal tears are demonstrated, we advise the athlete not to return to play and, instead, to undergo ACL reconstruction at the time of meniscal repair because of the greater likelihood of meniscal healing and the prevention of further instability episodes. If no meniscal damage is present and full range of motion and strength have returned, we allow athletes to return to play if they are already involved in a low-risk sport or they play at a low-risk position in their sport (i.e., lineman in football) and it is their final year of competition. The risks must be discussed with the athlete and the family, with the stipulation that if the knee gives out, the athlete must stop participation. These situations are rare, however, and should be treated on a case-by-case basis.
As of this writing, no study has demonstrated that bracing an ACL-deficient knee will prevent episodes of instability when the athlete returns to cutting and pivoting sports, but several studies have shown a decrease in anterior tibial translation at low levels of force. If the athlete and family decide that they do not want to proceed with ACL reconstruction, it must be understood that activity modification (i.e., avoiding twisting, cutting, and deceleration activities) will be necessary to prevent giving-way episodes. If the athlete attains and maintains full range of motion and at least 90% strength of the contralateral lower-extremity strength, low-risk sports, such as running, bicycling, and swimming, can be performed.
Nonoperative treatment of an ACL injury can be successful if the patient is willing to modify his or her lifestyle to avoid additional giving-way episodes. For many patients, this is difficult to accomplish. Bonamo et al. (27) found that despite a regimented strengthening program, including sport-specific exercises, 40% of 79 recreational athletes who sustained an ACL tear and elected to have nonoperative treatment had to modify their athletic activity significantly to avoid giving-way episodes, but only 9 patients (11%) demonstrated excellent results. Hawkins et al. (20) and Andersson et al. (28) similarly found that 75% to 80% of prospectively followed, ACL-deficient patients who were treated nonoperatively could not return to level I or II sports activities, although most could participate in some lower-risk sports. In fact, Daniel et al. (29) found that an athlete’s inability to return to sports is what brings that athlete to surgical treatment. Others have found that even with a mild grade of instability or with a patient who is relatively sedentary, half will fare poorly with nonoperative treatment (30). Both Warren (31) and Daniel et al. (29) found that the outcome of nonoperative treatment worsens as the severity of laxity increases, particularly in those who continue to participate in high-risk sports. Finally, studies do confirm that patients with chronic anterior instability develop meniscal tears (usually medial) with greater frequency and, in addition, are more likely to have chondral injuries compared with those having acute ACL injury.
Operative Indications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree